The Current State of Transradial Access:A Perspective on Transradial Outcomes,Learning Curves, and Same-Day Discharge
2018-09-17JenniferRymerMDMBAandSunilRaoMD
Jennifer A. Rymer, MD, MBA and Sunil V. Rao, MD
1Duke Clinical Research Institute, Durham, NC, USA
Abstract The adoption of transradial access in the United States and internationally has been growing over the past few years. In the population of patients presenting with acute coronary syndromes, particularly ST-elevation myocardial infarction,transradial access has the benefit of fewer vascular and bleeding complications and lower mortality rates over transfemoral access. We will examine the current evidence supporting transradial access for several patient populations, including those patients presenting with acute coronary syndromes. We will review the literature regarding the learning curve for transradial access with new operators, as well as experienced transfemoral operators new to transradial access. Finally,we will investigate the role of transradial access in same-day discharge for stable patients undergoing percutaneous coronary intervention.
Keywords: transradial; percutaneous coronary intervention; learning curves; outcomes; same-day discharge
lntroduction
Transradial access for cardiac catheterization and percutaneous coronary intervention (PCI) is widely used in Europe, Canada, and Asia. With increasing evidence that the radial approach reduces bleeding, vascular complications, and the time to ambulation after the procedure compared with the femoral approach, its adoption in the United States has been increasing [1–3]. In this review, we present the current state of evidence regarding transradial access, outcomes, and use.The literature on the outcomes associated with transradial intervention (TRI) versus transfemoral intervention (TFI) is examined, with a focus on bleeding and vascular complications, as well as patient preference. The challenges of the TRI learning curve are reviewed with a discussion of differences in outcomes by operator experience and caseload. We then examine the differences in the TRI learning curve by procedural setting, including ST-segment elevation myocardial infarction (STEMI), as well as patient and procedural complexity. Evidence for the safety of sameday discharge (SDD) after TRI is described, along with the potential economic benefits for health systems using a strategy of TRI and SDD. We also describe the existing barriers at many hospitals for pursuing an established SDD program for post-PCI patients.
Radial versus Femoral Access:Outcomes
Bleeding Complications and Death
The most common complications after PCI are bleeding and vascular complications, ranging from local access site hematomas to large retroperitoneal bleeds [4]. The incidence of clinically significant bleeding after PCI in the contemporary era is estimated to range between 0.6 and 14% depending on the definition, method of ascertainment, and clinical scenario [4, 5]. As post-PCI bleeding severity increases, the adjusted hazards of both 30-day and 6-month death increase in a stepwise fashion [6].A subanalysis of the ACUITY trial demonstrated that in patients who experienced an in-hospital major bleeding event, there was an association with increased 30-day death (7.3 vs. 1.2%,P< 0.0001)and stent thrombosis (3.4 vs. 0.6%,P< 0.0001)compared with patients who did not experience major bleeding events [7]. Major bleeding events after PCI have also been associated with increased costs [8]. From the REPLACE-2 and HORIZONSAMI trials, bleeding (defined by the Thrombolysis in Myocardial Infarction score) was associated with an increased risk of 1-year death [hazard ratio(HR) 3.17, 95% confidence interval (CI) 2.51–4.00,P< 0.00010] [9]. Furthermore, non-access site bleeds were associated with a higher risk of 1-year death than access site bleeds (HR 3.94, 95%CI 3.07–5.15,P< 0.0001 versus HR 1.82, 95% CI 1.17–2.83,P= 0.008).
There are data from both observational studies and randomized controlled trials (RCTs) associating post-PCI bleeding with worsened outcomes,and demonstrating decreased bleeding and death in patients undergoing TRI. A subanalysis of the National Cardiovascular Data Registry (NCDR)CathPCI Registry found a lower risk of bleeding and vascular complications among patients undergoing TRI compared with TFI [1]. In another observational study of patients from the NCDR CathPCI Registry, Rao et al. [10] demonstrated that post-PCI bleeding was associated with an increased risk of both short-term and long-term recurrent bleeding, major adverse cardiovascular events(MACEs), and all-cause death. In the STEMIRADIAL trial, 702 patients were randomized to undergo either femoral (n= 359) or radial (n= 348)access [11]. The cumulative incidence of major bleeding and vascular complications (1.4 vs. 7.2%,P= 0.0001), as well as net adverse clinical events(a composite of ischemic and bleeding events) (4.6 vs. 11.0%,P= 0.0028), was significantly lower in the TRI group than in the TFI group. In the Radial Versus Femoral Randomized Investigation in ST-Elevation Acute Coronary Syndrome (RIFLESTEACS), patients undergoing primary or rescue PCI for STEMI were randomized to undergo radial access (n= 500) or femoral access (n= 501) [12].Radial access was associated with lower rates of non-coronary artery bypass graft (CABG) bleeding (7.8 vs. 12.2%,P= 0.026), access site bleeding (2.6 vs. 6.8%,P= 0.002), cardiac death (5.2 vs. 9.2%,P= 0.020), and MACEs (7.2 vs. 11.4%,P= 0.029). Furthermore, in the Minimizing Adverse Haemorrhagic Events by Transradial Access Site and Systemic Implementation of Angiox (MATRIX) trial, the outcomes of radial access were compared with those of femoral access in acute coronary syndrome (ACS) patients with or without ST-segment elevation undergoing invasive management [13]. More than 8400 patients were randomized to undergo radial or femoral access, and the 30-day co-primary outcomes were MACEs and net adverse clinical events, including Bleeding Academic Research Consortium major bleeding unrelated to CABG. Patients undergoing radial access had significantly fewer MACEs(8.8 vs. 10.3%, rate ratio 0.85, 95% CI 0.74–0.99,P= 0.0307) and net adverse clinical events (9.8 vs. 11.7%, rate ratio 0.83, 95% CI 0.73–0.96,P= 0.0092). These differences were primarily driven by increased Bleeding Academic Research Consortium major bleeding unrelated to CABG and all-cause death in the femoral access arm.These trials demonstrate that the radial approach is associated with improved outcomes, particularly in STEMI patients, and that these improved outcomes are primarily driven by reduced bleeding.
Although radial access is associated with less major bleeding and improved short-term death outcomes, it is clearly not used more in patients with higher bleeding risks [14] – a phenomenon termed the “risk-treatment paradox.” Mamas et al. [14] examined the baseline bleeding risks of 348,689 patients undergoing PCI procedures, and demonstrated a 35% reduction in the risk of death at 30 days [odds ratio (OR) 0.65, 95% CI 0.59–0.72,P< 0.0001] with radial access. However, radial access was used less in the patients with the highest risk of bleeding complications, whereas patients with the lowest risk of bleeding complications were most likely to undergo TRI. As the radial approach is increasingly adopted, it will be important to use radial access in patients at higher risk of bleeding whenever technically feasible.
Vascular Complications
In addition to bleeding complications, common vascular complications associated with TFI include groin hematomas, arteriovenous fistulae, arterial pseudoaneurysms, and retroperitoneal hematomas.The incidence of TFI vascular complications has been reported in the literature to range between 1 and 5% of cases, in part depending on whether the patient was undergoing PCI versus a diagnostic catheterization [15–17]. Reductions in TFI vascular complication rates have been variably linked with lower rates of vascular closure device (VCD)failures and decreasing arterial sheath sizes [15,18]. Applegate et al. [18] demonstrated a reduction in all TFI vascular complications over a 7-year period at a high-volume center associated with use of smaller arterial sheaths and fewer VCD failures.The existing literature on the impact of VCDs on TFI vascular complication rates is contradictory and controversial. In a large meta-analysis of manual compression versus VCD use, there was no significant difference in the rate of vascular complications among patients treated with VCDs versus manual compression [19]. However, another large metaanalysis of VCDs found an association between VCD use and increased groin hematomas and pseudoaneurysms [20]. In the ISAR-CLOSURE trial, a large randomized multicenter trial of manual compression versus use of extravascular or intravascular VCDs in transfemoral coronary angiography(not PCI), use of VCDs was noninferior to manual compression with respect to the rates of vascular complications [21]. Despite these contradictory data, VCDs are commonly used in clinical practice,with estimates from the NCDR CathPCI Registry approximating that they are used in more than 45%of TFI procedures [22].
Radial access, however, has in contrast been associated with decreased vascular access complications. The Radial Versus Femoral Access for Coronary Intervention (RIVAL) trial randomized 7021 patients with ACS undergoing an early invasive strategy to undergo either femoral (n= 3514)or radial (n= 3507) access [2, 4]. The primary outcome was the incidence of 30-day net adverse clinical events defined as a composite of death,myocardial infarction, stroke, or major bleeding.Although there were no significant differences in the primary outcomes among patients undergoing femoral versus radial access, there were significantly fewer 30-day major vascular complications in the TRI group. Moreover, in a subgroup analysis of women randomized in the RIVAL trial, major vascular complication rates were significantly reduced with the use of radial access (3.1 vs. 6.1%,HR 0.5, 95% CI 0.32–0.78,P= 0.002) [23]. Women represent a group at particularly high risk of bleeding and vascular complications, and the SAFEPCI for Women trial compared radial and femoral access in women undergoing coronary angiography or PCI. Although it was terminated early for lower than expected bleeding and vascular complication rates [24], there was a significant difference in both bleeding and vascular complications among women undergoing cardiac catheterization or PCI. These results are also consistent with those in patients undergoing complex PCI [25].
lmproved Outcomes in ACSs
In the ACS population, there is ample support for TRI from recent RCTs for reducing death, primarily by decreasing bleeding [26, 27]. Andò and Capodanno [28] performed a meta-analysis of four recent, high-quality trials of TRI versus TFI in the ACS population. In more than 17,000 pooled patients, TRI was associated with reductions in access site bleeding [relative risk (RR) 0.36, 95%CI 0.28–0.47,P< 0.01], major bleeding (RR 0.57,95% CI 0.37–0.88,P= 0.011), MACEs (RR 0.86,95% CI 0.75–0.98,P= 0.25), and all-cause death(RR 0.73, 95% CI 0.59–0.90,P= 0.003). The findings of this meta-analysis are notable in that they represent the outcomes of ACS patients with and without STEMI. Reduced death because of bleeding reductions has been particularly demonstrated in the STEMI population. In RIFLE-STEACS,which investigated outcomes in the STEMI population only, the composite outcome of net adverse clinical events (13.6 vs. 21.0%,P= 0.003) and cardiac death (5.2 vs. 9.2%,P= 0.020) was significantly reduced in the TRI arm versus the TFI arm [12]. Additionally, in an analysis of RIVAL comparing outcomes of TRI versus TFI between non-ST-segment elevation myocardial infarction(NSTEMI) patients and STEMI patients, the primary composite outcome of death, myocardial infarction, stroke, and non-CABG-related major bleeding was significantly reduced in the STEMI subgroup (3.1 vs. 5.2%,P= 0.026) but in not the NSTEMI subgroup (3.8 vs. 3.5%,P= 0.49) [26].However, after stratification of patients randomized in the MATRIX trial by presentation for NSTEMI versus STEMI, there was reduction in all-cause death (Pint= 0.11), regardless of ACS type for patients undergoing TRI versus TFI [27].Although there is some contradictory evidence for the mortality benefits of TRI in NSTEMI, the benefit of TRI in the STEMI population has been well established. Table 1 lists major TRI RCTs according to whether patients had stable cardiovascular disease or ACS.
Patient Preference
When one is examining TRI versus TFI, it is important to consider the importance of patient preference for the access site. Several studies have demonstrated patient preference for radial over femoral access [32–34]. In the recently published PREVAS study, patients who had undergone elective coronary angiography or PCI were surveyed to assess their preference for key treatment characteristics related to vascular access (i.e., bleeding, switch of access site, postprocedural vessel quality, mobilization and comfort, and overnight stay) [32]. The factors that were most important to patients included bleeding(31.3%), length of hospitalization (22.6%), and mobilization (20.2%) – areas in which TRI has an advantage over TFI. Furthermore, patients who had undergone both types of access during prior PCI procedures were significantly more likely to prefer radial access (71.1%,P< 0.001). In the SAFE-PCI for Women trial, patients assigned to radial access more often preferred radial access (77.2%) over femoral access during a repeated procedure (26.8%,P< 0.001) [24, 33]. Other studies have shown that most patients (88.6%) undergoing radial access prefer SDD [34]. Overall, patients tended to prioritize procedural characteristics most associated with radial access, and would prefer radial access during repeated PCI procedures.
The Transradial Learning Curve
Despite the noted benefits of the radial approach,several barriers have resulted in slower adoption of this approach, including concerns over the learning curve. This has directly affected the uptake of radial access for primary PCI, where the data show the biggest advantage of the radial approach. Concerns over prolonged door-to-balloon (DTB) time and the potential need for crossover to femoral access are related to proficiency with the radial approach,which can be achieved once the learning curve has been overcome [35, 36]. Additionally, the learning curve for radial access may differ according to the population (i.e., women and the elderly) [24] and the setting in which it is being used [37].
Operator Experience and Outcomes:Quantifying the Learning Curve
Several studies examined the impact of operator experience with TRI cases and procedural outcomes [38–41]. Specifically, Huded et al. [38]recently published an analysis of the effect of operator TRI case experience on TRI outcomes in more 4000 attempted TRI procedures over a 7-year period, during which a large, tertiary care center adopted the radial approach. Increased operator experience was significantly associated with improved procedural outcomes, including decreased radial artery cannulation failure, femoral crossover, contrast medium dose, and fluoroscopy time. Operators with more than 100 TRI cases had the lowest odds of radial artery cannulation failure, while operators with more than 200 TRI cases had the lowest odds of femoral crossover, the lowest mean contrast medium dose, and the lowest mean fluoroscopy time. Additionally,with increasing institutional experience, the radial artery cannulation failure rate fell from 4.9 to 2.0%(P= 0.071) over the study period, and the rate of femoral crossover decreased from 4.3 to 3.2%(P= 0.034). These results are consistent with best practice guidelines that recommend a graduated approach based on increasing experience before operators are allowed to perform more complex,radial STEMI or PCI cases [42].
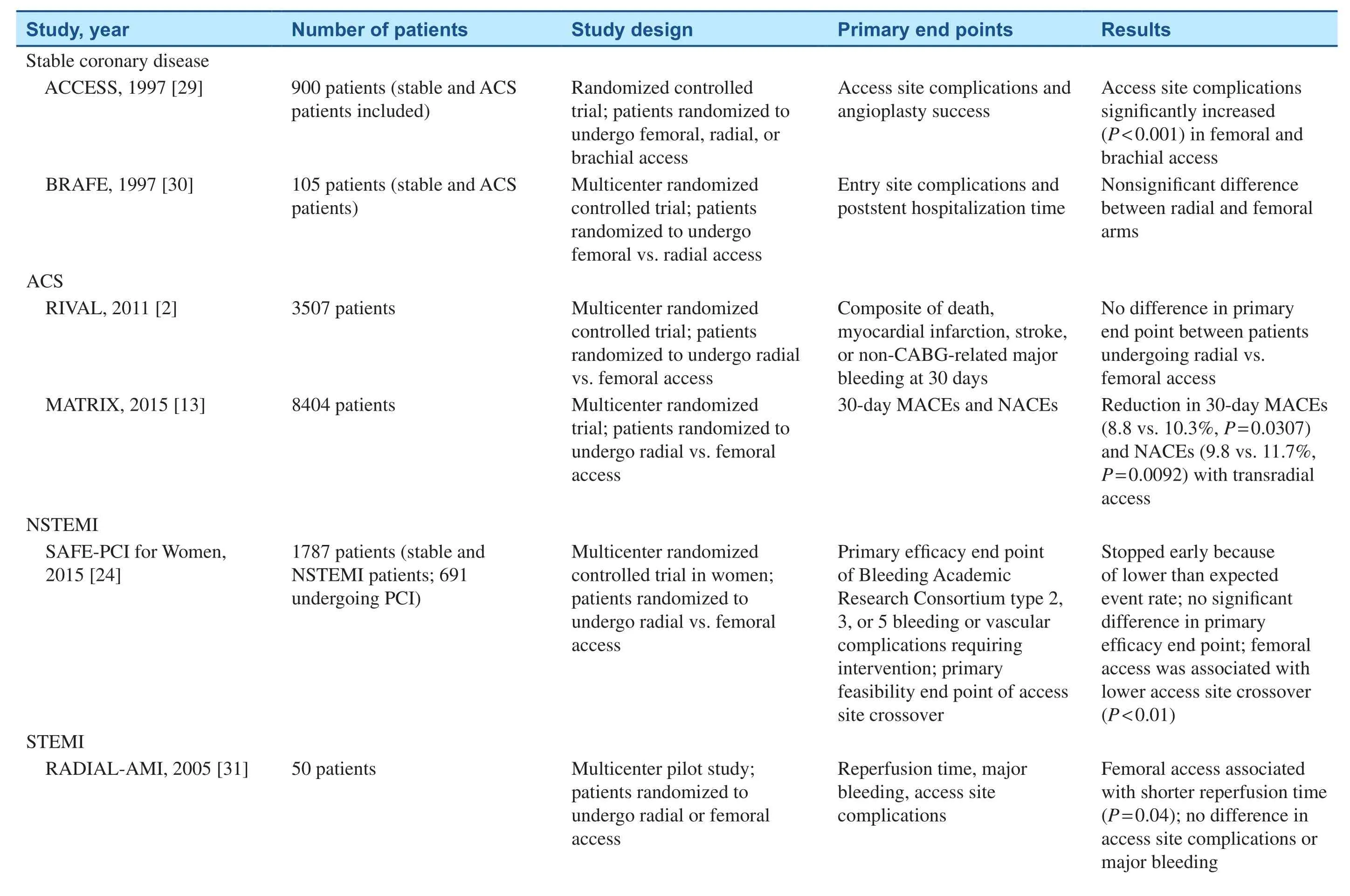
Table 1 Summary of Major Randomized Controlled Trials of the Transradial Approach in Stable Coronary Disease and Acute Coronary Syndrome (ACS).
Other analyses have also examined the effect of the TRI learning curve on patient outcomes.Barbash et al. [39] analyzed the outcomes of two cohorts of patients: the last 250 patients who underwent femoral access before the adoption of a TRI program and the first 239 patients who underwent radial access after the adoption of a TRI program.The cohort of TRI patients was further divided into five groups to analyze the differences in outcomes among the earliest TRI groups compared with the later TRI groups, thus examining the TRI learning curve. Barbash et al. [39] found no significant differences in fluoroscopy time, rates of stent thrombosis, and death rates among the five subgroups. As the cases of only two high-volume TFI operators were analyzed, perhaps a limitation of this study might be that operators skilled at TFI may have a different learning curve than those with less overall experience. Although this analysis did not seem to demonstrate significant differences in outcomes during early and later TRI cases, other multicenter studies have demonstrated case number thresholds, after which the learning curve is overcome.

dna etiS sseccA laidarsnarT yb stnevE cigahrromeaH esrevdA gniziminiM ,XIRTAM ;tneve ralucsavoidrac esrevda rojam ,ECAM ;tfarg ssapyb yretra yranoroc ,GBAC -retni yranoroc suoenatucrep ,ICP ;noitcrafni laidracoym noitavele tnemges-TS-non ,IMETSN ;tneve lacinilc esrevda ten ,ECAN ;xoignA fo noitatnemelpmI cimetsyS rof sseccA laromeF susreV laidaR ,LAVIR ;emordnyS yranoroC etucA noitavelE-TS ni noitagitsevnI dezimodnaR laromeF susreV laidaR ,SCAETS-ELFIR ;noitnev .noitcrafni laidracoym noitavele tnemges-TS ,IMETS ;noitnevretnI yranoroC ?)deunitnoc(1 elbaT
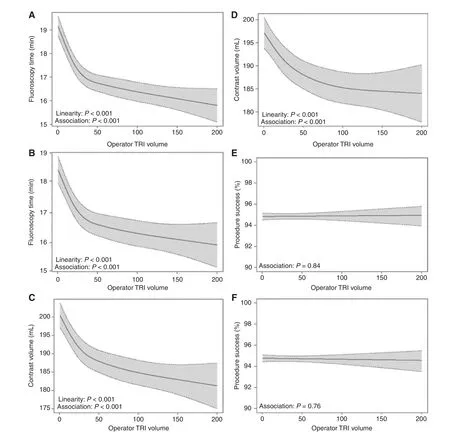
Figure 1 The Association Between Operator Transradial Intervention (TRI) Volume/Experience and Procedural Outcomes.The curves demonstrate the unadjusted and adjusted relationships between TRI volume and fluoroscopy time (A and B,respectively), unadjusted and adjusted relationships between TRI volume and contrast medium volume (C and D, respectively),and unadjusted and adjusted relationships between TRI volume and procedural success (E and F, respectively). Dotted lines represent 95% confidence intervals. (Reproduced from Hess et al. [40].)
A large NCDR analysis of 54,561 TRI procedures performed by new TRI operators demonstrated a significant association after adjustment between TRI volume and both fluoroscopy time and contrast medium volume used [41]. There was a steep reduction in fluoroscopy time and contrast medium volume used compared with their earlier procedures, with an inflection point at 30–50 procedures. After 50 TRI procedures had been performed, continued reduction in fluoroscopy time and contrast medium volume used was demonstrated; however, the slope was flatter (see Figure 1). For outcomes, including procedural success, vascular access complications, and inhospital death, there was no significant difference during the learning curve despite more complex procedures being performed, as operators continued to increase their radial volume. Similar results were demonstrated in a Canadian study of 1672 patients undergoing nonurgent PCI, where the control group consisted of operators who had performed more than 300 TRI procedures compared with less-experienced operator groups [42]. The rates of radial access failure were significantly higher in the subgroup that had performed only 1–50 TRI procedures compared with the control group (7 vs. 2%,P< 0.01). Again, the learning curve for TRI success, when assessed by contrast medium volume used, fluoroscopy time, and access failure, plateaued after 50 TRI procedures had been performed. These studies highlight the importance of experienced mentorship for inexperienced TRI operators and trainees, but most importantly illustrate the relative safety of the TRI learning curve for patients. Additionally, as there is potentially less catheter manipulation in transradial PCI compared with transradial diagnostic angiography, the need for mentorship and experience with transradial diagnostic catheterizations before transradial PCI is performed is likely important.
STEMl and High-Risk, Complex PCl
The learning curve for radial STEMI comes with additional challenges and a concern for impact on DTB time and femoral crossover [36]. For highrisk, complex PCI cases, there are also additional concerns, such as accessing and managing patients who may be hemodynamically unstable and eventually require additional large-caliber hemodynamic support. Best practice guidelines recommend that operators should perform primary PCI only after having successfully performed 100 elective TRI procedures with a femoral crossover rate of 4% or less [42]. Additionally, operators should consider bailout to femoral access or the contralateral radial access site if radial access takes more than 3 min,and femoral site preparation should occur in higherrisk patients, who may need additional, urgent hemodynamic support.
Although there are few analyses specifically focused on DTB time with TRI, there are several large clinical trials with data on clinical volume,operator experience, and DTB time [36]. In the RIVAL trial, the time from randomization to completion of PCI was longer in TRI cases in low- and intermediate-volume TRI centers [2]. However, in TRI procedures performed at high-volume centers(more than 146 TRI procedures per operator per year), the time from randomization to completion of PCI was not significantly different from that for TFI procedures (55 vs. 51 min,P= 0.78). In the STEMI-RADIAL trial, which included only four high-volume radial centers, there was no significant difference in DTB time among patients undergoing PCI using the radial or femoral approach [12].These results suggest that DTB time when the radial approach is used does not significantly differ from that when TFI is used if it is performed by more experienced operators.
Another common concern within the interventional community that has contributed to slowed adoption of the radial approach for STEMI has been concern for radial access failure and the need for femoral crossover [36]. A Canadian study of more than 1600 patients undergoing TRI cited the most common reasons why the least experienced operators (1–50 prior TRI procedures) had access failure, which included radial artery spasm (38%),subclavian tortuosity (16%), poor guide catheter support (16%), inability to access the radial artery(10%), and existence of a radial artery loop (7%)[41]. In addition to actual puncture failures, there is concern that navigating the tortuous arm and subclavian artery vasculature could lead to increased vascular access–related time (VART), potentially leading to an overall increase in DTB time [43].Despite these concerns, Azzalini et al. [43] demonstrated that although VART increased from a mean of 4.1 min for successful radial access to 10.3 min when femoral crossover was required, this increase in mean VART did not have any significant impact on the primary end point, the final corrected Thrombolysis in Myocardial Infarction frame count.Other analyses have demonstrated higher rates of femoral crossover among inexperienced operators compared with more experienced operators [2, 11,41]. In the RIVAL trial, the overall femoral crossover rate was 7.6%; however, among the highest tertile of operator experience, femoral crossover dropped to 4.0% [2]. In RIFLE-STEACS, the rate of TFI crossover due to radial failure hovered around 6.0% for expert operators compared with 1.0% due to femoral access failure [11]. Femoral crossover in the hands of the expert operators was associated with negligible time delay. Although most crossover rates are higher for TRI procedures with even the most experienced operators, there does not seem to be evidence for worsened outcomes or a clinically significant increase in DTB time.
The TRI learning curve differs not only by the setting but can also differ by procedural complexity [22]. An analysis of the TRI learning curve in unprotected left main coronary artery (ULMCA)PCI found no significant differences in procedural success, contrast medium volume used, procedural and fluoroscopy time, and MACEs among patients who underwent TRI ULMCA PCI versus TFI ULMCA PCI performed by an inexperienced operator [44]. Other observational studies have demonstrated comparable TRI and TFI procedural success and short-term outcomes after ULMCA PCI when performed by experienced operators [45, 46]. A recent observational study of the radial approach to chronic total occlusions (CTOs) did not show any significant differences in procedural success,bleeding complications, procedural duration, or radiation dose for transfemoral versus transradial CTOs when performed by experienced operators[47], although more complex CTO procedures may require at least one femoral access site to facilitate support and passage of equipment. Furthermore, a meta-analysis demonstrated an association with significant improvement in procedural success among those transradial CTO procedures performed at a later time compared with those performed earlier in the centers’ experiences [48]. For particularly complex procedures such as CTOs, the choice of access site should take into account the support needed and equipment compatibility. Further studies are needed to better understand the differences in the learning curve in more complex PCI cases.
Same-Day Discharge
The concept of SDD after PCI has resulted from a combination of patient preference, feasibility,and increasing economic pressures. In the United States, hospital payment for PCI by the Centers for Medicare & Medicaid Services was based on an inpatient rate; however, over time, PCI became considered an outpatient procedure that had lower hospital payment [49, 50]. PCI now qualifies for inpatient payment only if two midnights are spent in the hospital with justification [51–53]. Thus many hospitals and health systems are considering SDD for selected PCI patients to increase bed availability, patient satisfaction, and financial margins.
Several analyses have further examined the safety of SDD versus an overnight stay for patients undergoing largely elective TRI [54, 55]. A large meta-analysis of 13 studies (both randomized and observational studies) with 111,830 patients was performed to examine the safety of SDD [54]. The total rate of complications for SDD versus an overnight stay was 6.5 vs. 5.5% (OR 1.20, 95% CI 0.82–1.74) for the RCTs, and 4.7 vs. 9.6% (OR 0.67, 95%CI 0.27–1.66) for the observational studies. The incidence of 30-day rehospitalization after PCI for SDD versus an overnight stay was 4.0 vs. 3.6% (OR 1.10, 95% CI 0.70–1.74) for the RCTs and 8.0 vs.9.6% (OR 0.62, 95% CI 0.10–3.98) for the observational studies. Finally, the incidence of MACEs after PCI for SDD versus an overnight stay was 1.3 vs. 1.3% (OR 0.99, 95% CI 0.45–2.18) for the RCTs and 0.6 vs. 1.2% (OR 0.59, 95% CI 0.06–5.57) for the observational studies. Additionally, Gilchrist et al. [55] compared a population of 100 patients undergoing TRI and with SDD with the Society for Cardiovascular Angiography and Interventions/American College of Cardiology consensus on outpatient PCI, and found that only 15% of the SDD patients would have met the criteria for early discharge, with the remainder being considered “high risk” by the consensus statement. Many of these patients were older than 70 years, lived more than 20 miles from the PCI hospital, and had undergone complex PCI. None of these patients were readmitted for complications related to the PCI procedure that would have been addressed by an overnight stay. Gilchrist et al. suggested that the patient population that may be acceptable for SDD after undergoing TRI may be safely expanded at many PCI centers. As further data accrue regarding the safety of SDD for patients with higher-risk features who remain stable after PCI, the criteria for SDD eligibility will likely continue to expand.
The Business Case for SDD
Although there are sparse data on the economic impact of SDD for patients undergoing TRI, several recent studies have demonstrated that avoiding an overnight stay after PCI is associated with cost savings for the hospital [53, 56]. Amin et al. [53] used the NCDR CathPCI Registry to examine 279,897 PCI procedures, of which 9.0% involved radial access and 5.3% involved SDD. Only 1.2% of the procedures involved both radial access and SDD.The hospital cost associated with TRI plus SDD was$13,389 (95% CI $13,161 to $13,607), while TFI procedures with an overnight stay were associated with a cost that was $3689 (95% CI $3486 to $3902,P< 0.0001) higher. Similarly, the Canadian Early Discharge After Transradial Stenting of Coronary Arteries (EASY) trial randomized 1005 patients to receive a bolus of only abciximab and TRI coronary stenting plus SDD or to an overnight hospitalization with a 12-h abciximab infusion [56]. A cost analysis performed 30 days after discharge found that the mean cumulative cost for the SDD group was 1117 ± 1554 Canadian dollars versus 2258 ± 1328 Canadian dollars for the overnight group, with a mean difference of 1141 Canadian dollars favoring SDD. The study authors concluded that most of the additional costs in the overnight group resulted from the additional hospital day.
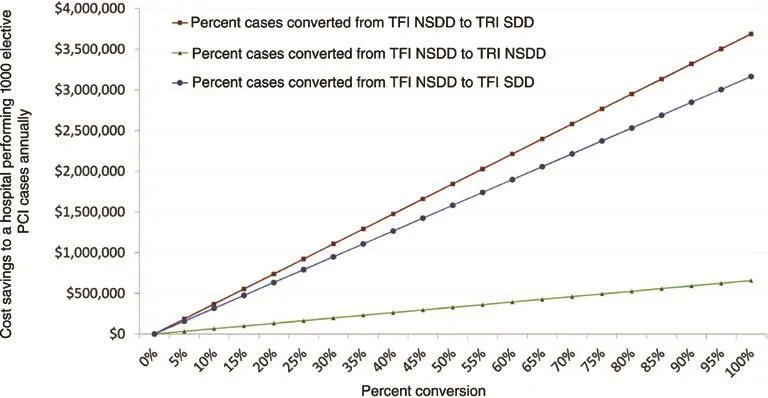
Figure 2 Cost savings to a hospital performing 1000 elective percutaneous intervention (PCI) procedures annually when converting from transfemoral intervention and non-same-day discharge (TFI NSDD) to transradial intervention and same-day discharge (TRI SDD), transfemoral intervention and same-day discharge (TFI SDD), or transradial intervention and non-sameday discharge (TRI NSDD). (Reproduced from Amin et al. [53].)
As more than 600,000 PCI procedures are performed in the United States annually [57], transitioning an overnight stay to an SDD in appropriate patients has the potential to have a large economic impact on hospitals and health care systems. In 2016 the US Department of Health and Human Services ranked PCI procedures as the second most common cause of increased costs in short inpatient stays of Medicare patients [49]. As there is now the Centers for Medicare & Medicaid Services “two-midnight rule,” patients are now categorized as outpatients if their hospitalization does not include two midnights. Thus, aside from those presenting with ACS, almost all patients undergoing PCI are considered “outpatients” for reimbursement purposes. There are several estimates that if post-PCI patients are categorized as outpatients but not discharged on the same day,these hospitalizations could result in increased costs on the order of $2000 to $4000 per PCI for the hospitals [49, 51, 58, 59]. As demonstrated in Figure 2, SDD should be considered in all patients who have undergone a successful PCI procedure without post-PCI complications and have a stable access site and adequate home support. Although this strategy for SDD can certainly include patients undergoing TFI procedures, radial access more readily lends itself to an SDD strategy.
Despite increasing economic incentives to pursue SDD in many elective PCI patients, several barriers remain [60]. Features associated with an overnight stay compared with SDD included creatinine clearance of 60 mL/min or less, larger sheath size, and increased use of bivalirudin and glycoprotein IIb/IIIa inhibitors [60]. In an analysis from the NCDR CathPCI Registry, nearly 100,000 PCI patients who were eligible for outpatient reimbursement were assessed, with the finding that that rate of post-PCI SDD increased from 32.8 to 66.3% (P< 0.001) [61]. Among patients with the highest risk of death, the proportion of these high-risk patients who were not admitted increased from 17.0 to 19.8%, perhaps not a desired result of SDD programs. Vora et al. [61] concluded that outpatient reimbursement classification should be tied to predicted the risk of death to better target the appropriate post-PCI patients for SDD. Current hospital culture and practice may also stand as a barrier to effectively triaging appropriate post-PCI patients to SDD, as hospitals may be reluctant to drastically change practice patterns. These analyses highlight that the likely greatest barriers to SDD include existing hospital culture, reluctance to change practice patterns, and the need to develop a triage algorithm to effectively select appropriate patients for SDD.
When one is considering an algorithm for appropriate SDD, there are five important patient care and procedural domains to consider as defined by Abdelaal et al. [54]. Even if patients had an uncomplicated procedure, they may not besuitablefor discharge because of poor health literacy,poor social support, and frailty. Secondly, patients considered for SDD should have anoptimal procedural outcome[54], defined as “successful PCI(excellent angiographic result, without significant residual stenosis after stenting, and Thrombolysis in Myocardial Infarction 3 flow without dissection or thrombus), no compromise (i.e., reduced flow) of a side branch at least 2 mm in diameter,and no postprocedural chest pain.” Additionally,stabilization of vascular accesswith appropriate hemostasis and without evidence of vascular complications should be determined before SDD is considered. Furthermore, there should be a process for teaching and instructing the patient on the importance of dual antiplatelet therapy if SDD is considered. Finally, and most importantly, there should be apostprocedural processwhereby the patient is provided with discharge instructions and contact information, and a phone call is made the next day to assess how the patient is doing at home.
Conclusions
The current state of evidence supports radial access as the preferred approach for PCI, as it can decrease bleeding and vascular complications, can reduce the time to mobility after cardiac catheterization,and is generally preferred by patients who have undergone both approaches during prior procedures. Importantly, the radial approach has been shown to reduce death in high-risk patients such as those with ACS and, in particular, STEMI undergoing primary PCI. The best outcomes from TRI are achieved by operators who are proficient with the radial approach and use it as the default access in all patients, thereby avoiding the risk-treatment paradox. Becoming proficient with TRI requires overcoming the learning curve, which is relatively shallow. With rising economic pressures, the combination of radial access and SDD should be strongly considered for appropriate patients undergoing outpatient PCI.
杂志排行
Cardiovascular Innovations and Applications的其它文章
- Speckle Tracking Echocardiography ldentifies lmpaired Longitudinal Strain as a Common Deficit in Various Cardiac Diseases
- Current Status of Coronary Atherectomy
- The Use of Direct Oral Anticoagulants for Prevention of Stroke and Systemic Embolic Events in East Asian Patients with Nonvalvular Atrial Fibrillation
- Bioresorbable Vascular Scaffold in the Midportion of the Left Anterior Descending Artery for Cardiac Allograft Vasculopathy in a Cardiac Transplant Patient
- The Contemporary Role of Femoral Artery Access
- Cardiovascular Innovations and Applications