Clinical observation of abdominal acupuncture for subhealth insomnia
2018-09-12FengHua冯骅DingMin丁敏XiangYi向谊
Feng Hua (冯骅), Ding Min (丁敏), Xiang Yi (向谊)
Abstract Objective: To assess the clinical efficacy of abdominal acupuncture for subhealth insomnia.Methods: Eighty-two cases of subhealth insomnia were randomly divided into an observation group (41 cases) and a control group (41 cases). The control group was treated with conventional acupuncture. The observation group was treated with Bo’s abdominal acupuncture on the basis of conventional acupuncture. Six treatments constituted one treatment course.The measuring scale of traditional Chinese medicine syndrome for subhealth state (MSSSHS) and Pittsburgh sleep quality index (PSQI) scores were compared between the two groups after two courses, to estimate the efficacy of abdominal acupuncture for subhealth insomnia.Results: One case dropped out from the observation group, while 2 cases dropped out from the control group. The MSSSHS score and PSQI score both declined after the treatment in the two groups (all P<0.05). The MSSSHS and PSQI scores in the observation group were significantly lower than those in the control group (both P<0.05).Conclusion: The abdominal acupuncture is effective for subhealth insomnia, and it can enhance the effect of conventional acupuncture.
Keywords: Acupuncture Therapy; Abdominal Acupuncture; Fatigue Syndrome, Chronic; Subhealth; Sleep Disorders;Insomnia
On January 16, 2006, China Association of Chinese Medicine proposed a third state between health and illness, namely subhealth in Discussing and Analyzing Prevention and Cure Strategy of Traditional Chinese Medicine According to Characteristic of Subhealth Condition[1]. Insomnia is a common symptom in subhealth population, together with the presence of dreaminess and early awakening. Mild-to-moderate insomnia affects nearly 98.5% in all subhealth patients,while severe insomnia affects only 1.5%[2]. Insomnia will lead to memory disorders, loss of attention, decreased learning and work capability, and is usually concomitant with chronic fatigue. Such vicious circle will cause grave impact on patients’ daily learning, working activity and social communication. For subhealth is a mental disorder other than physical sickness, Western medicine mainly applies sedative and hypnotic drugs for treatment. However, such medicine will cause adverse reactions such as drowsiness, dizziness or withdrawal reaction. Besides, long-term administration of such drugs will lead to drug resistance, causing dependence,and an unsatisfactory overall effect[3]. Acupuncture treatment can boost immune functions in human body and correct mind-body imbalance to intervene subhealth state[4]. To achieve maximum advantages of acupuncture, we used abdominal acupuncture in this study to treat subhealth insomnia, and the report is now given as follows.
1 Clinical Materials
1.1 Diagnostic criteria
Conforming to the diagnostic criteria of subhealth in Interpretation on Clinical Guideline of Chinese Medicine on Subhealth[5]. Main symptoms include fatigue, sleep disturbance or physical pain; psychological symptoms included depression, anxiety, fear, memory deterioration, or difficulty concentrating; decreased frequency of interpersonal communication or tension in interpersonal relationship which indicated a decreased social adaptive capability.
1.2 Inclusion criteria[6]
Conforming to the diagnostic criteria above; with a disease duration over 3 months, together with a decreased adaptability, and recurrent discomforts; main symptom was insomnia, and distresses and impaired social functions caused by unsatisfactory sleeping quality or quantity; Pittsburgh sleep quality index (PSQI)score over 7 points; without the administration of hypnotics; informed consent.
1.3 Exclusion criteria
Women during pregnancy or lactation; unable to cooperate with treatment schedule in this research;receiving other clinical researches in the resent 3 months; nervous system diseases which may cause sleep disorders.
1.4 Statistical methods
The data processing was done using the SPSS version 17.0 software. Measurement data were expressed as mean ± standard deviation (±s), and compared by t-test. Enumeration data were expressed as percentage and compared by Chi-square test. P<0.05 indicated statistical significance.
1.5 General data
A total of 82 subhealth patients with insomnia were included between July 2015 and March 2016 from the Acupuncture-moxibustion Department, Wuxi Hospital of Traditional Chinese Medicine, Jiangsu Province.According to their visiting sequence, they were randomized with the random number table into an observation group of 41 cases and a control group of 41 cases. During the observation period, 1 case dropped out from the observation group while 2 from the control group. These 3 cases all dropped due to work.Finally, 79 cases were included, with 40 cases in the observation group and 39 cases in the control group. By analysis, the differences in gender, age and disease duration were not statistically significant between the two groups (all P>0.05), indicating that the two groups were comparable (Table 1). The study flow chart is shown in Figure 1.
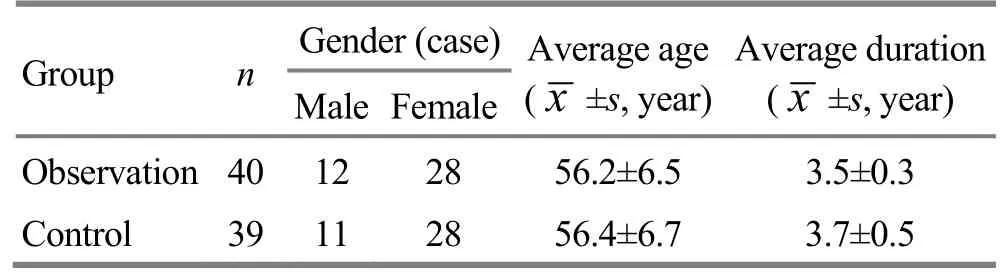
Table 1. General data comparison
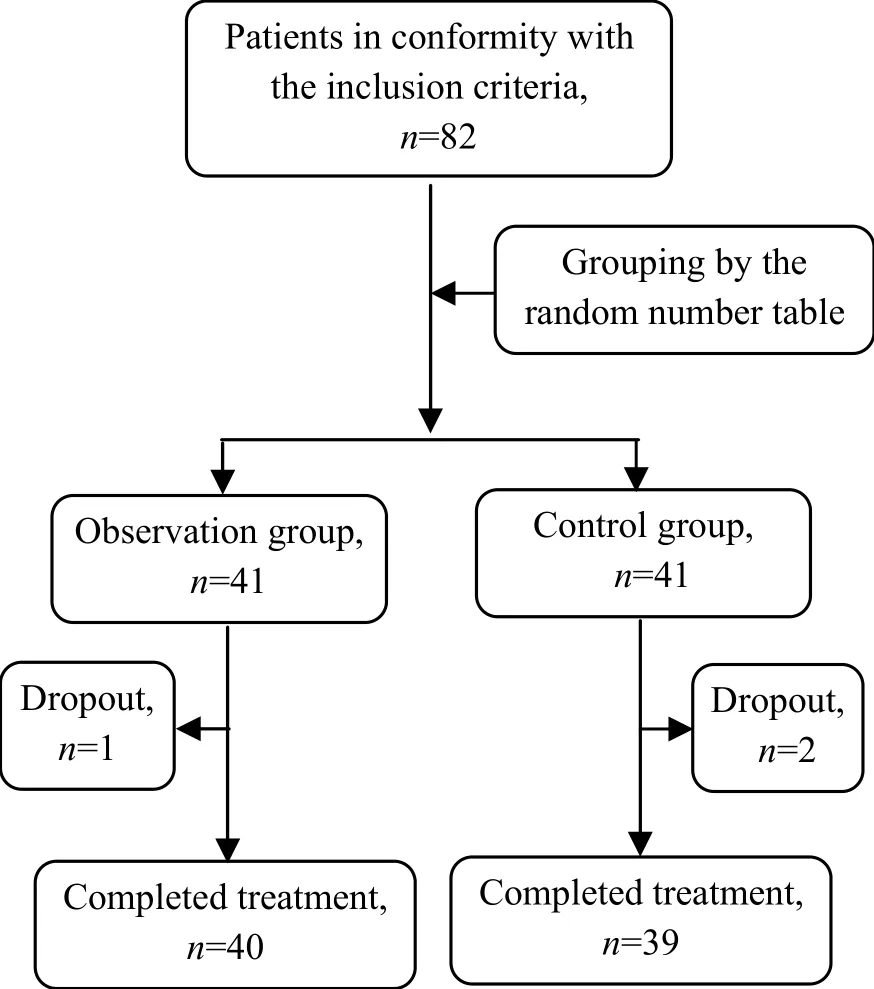
Figure 1. The flow chart
2 Treatment Methods
2. 1 Observation group
2.1.1 Conventional acupuncture
Acupoints: Baihui (GV 20), Sishencong (EX-HN 1),bilateral Shenmen (HT 7), Neiguan (PC 6), Sanyinjiao(SP 6) and Zusanli (ST 36).
Method: After routine sterilization, filiform needles of 0.25 mm in diameter and 25 mm in length were used to puncture Baihui (GV 20), Sishencong (EX-HN 1) and Shenmen (HT 7). Inserted the needle obliquely at a 30°angle to skin and to depth of 10-15 mm; used needles of 0.30 in diameter and 40 mm in length to puncture perpendicularly at Neiguan (PC 6), Sanyinjiao (SP 6) and Zusanli (ST 36). The needles were inserted to 15-20 mm,and even reinforcing-reducing manipulation was applied upon qi arrival.
2.1.2 Abdominal acupuncture
Abdominal acupuncture was used on the basis of the conventional acupuncture.
Acupoints: Yinqiguiyuan [Zhongwan (CV 12), Xiawan(CV 10), Qihai (CV 6) and Guanyuan (CV 4)], Shangqu(KI 17) on the left side, Qipang (Extra, located at 1.5 cun below the umbilicus and 0.5 cun lateral to the front midline) on the left side, and Qixue (KI 13) on the left side.
Method: After routine sterilization, filiform needles of 0.25 mm in diameter and 40 mm in length were punctured perpendicularly at the acupoints. The needles were adjusted to perpendicular to the skin after inserting into 10 mm. The feelings of soreness,numbness, heaviness and distention were not required.
Conventional and abdominal acupuncture both lasted 30 min each time, and the treatment was done every other day, with 6 treatments as a course. The therapeutic evaluation was done after 2 courses.
2.2 Control group
Patients in the control group received the same conventional acupuncture treatment as that in the observation group, with the same acupoints,manipulation, retaining time and courses.
Patients in the two groups did not use hypnotics before and during the treatment period.
3 Observation of Therapeutic Efficacy
3.1 Observation items and methods
3.1.1 Clinical symptoms
The measuring scale of traditional Chinese medicine(TCM) syndrome for subhealth state (MSSSHS) was used for evaluation of clinical symptoms[7]. Items mainly include confidential data, clinical symptoms, general data and signs, tongue and pulse. A total of 90 items are included in this scale, each item is scored according to the symptom severity from 1-5 points which indicate totally not, occasional, sometimes, frequent and always,respectively.
3.1.2 PSQI[8]
The PSQI includes 18 counting items with 7 subscales,including subjective sleep quality, sleep latency, sleep duration, habitual sleep efficiency, use of sleep medication, sleep disturbance and daytime dysfunction.Each item is scored 0 to 3 points. Score of the whole scale ranges from 0 to 21 points, and a higher score indicates a poorer sleep quality.
3.2 Therapeutic efficacy evaluation
Conforming to the therapeutic evaluation criteria of insomnia in the Criteria of Diagnosis and Therapeutic Effects of Diseases and Syndromes in Traditional Chinese Medicine[9].
Cured: Recovery of sleep duration or the total sleep duration above 6 h, with disappeared clinical symptoms.
Effective: Sleep duration increased by more than 2 h when compared with that before treatment, with improved clinical symptoms.
Invalid: No improvements in sleep and clinical symptoms.
3.3 Results
3.3.1 Comparison of clinical efficacy
The total effective rate was 87.5% in the observation group versus 71.8% in the control group, and the difference in the total effective rate showed statistical significance (P<0.01), (Table 2).
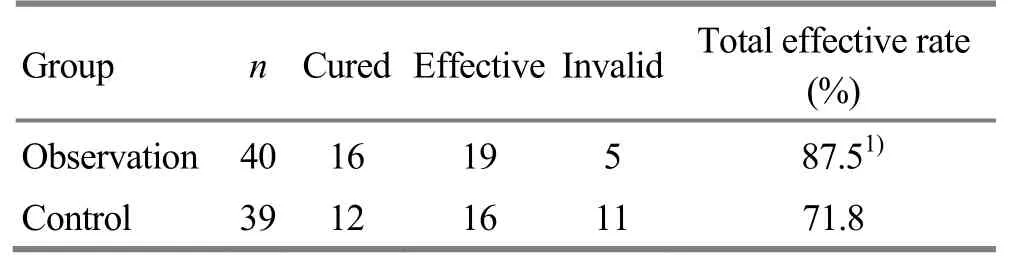
Table 2. Comparison of clinical efficacy (case)
3.3.2 Comparison of MSSSHS score
Before the treatment, the difference in MSSSHS score between the two groups showed no statistical significance (P>0.05). After the treatment, MSSSHS scores in the two groups dropped significantly (both P<0.01); the MSSSHS score in the observation group was lower than that in the control group, and the between-group comparison showed a significant difference (P<0.01), (Table 3).
Table 3. Comparison of MSSSHS score (±s, point)
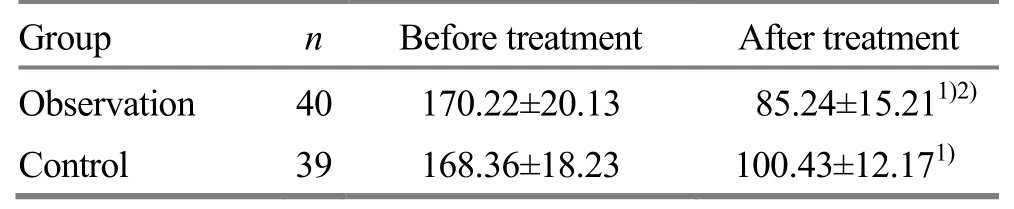
Table 3. Comparison of MSSSHS score (±s, point)
Note:Ⅰntra-group comparison,1)P<0.01; inter-group comparison, 2) P<0.01
?
3.3.3 Comparison of PSQI score
Before the treatment, the difference in PSQI score between the two groups showed no statistical significance (P>0.05). After the treatment, the total and component PSQI scores in the two groups dropped significantly (both P<0.01); the total and component PSQI scores in the observation group were lower than those in the control group, and the between-group comparisons showed significant differences (all P<0.05),(Table 4).
Table 4. Comparison of PSQI score (±s, point)
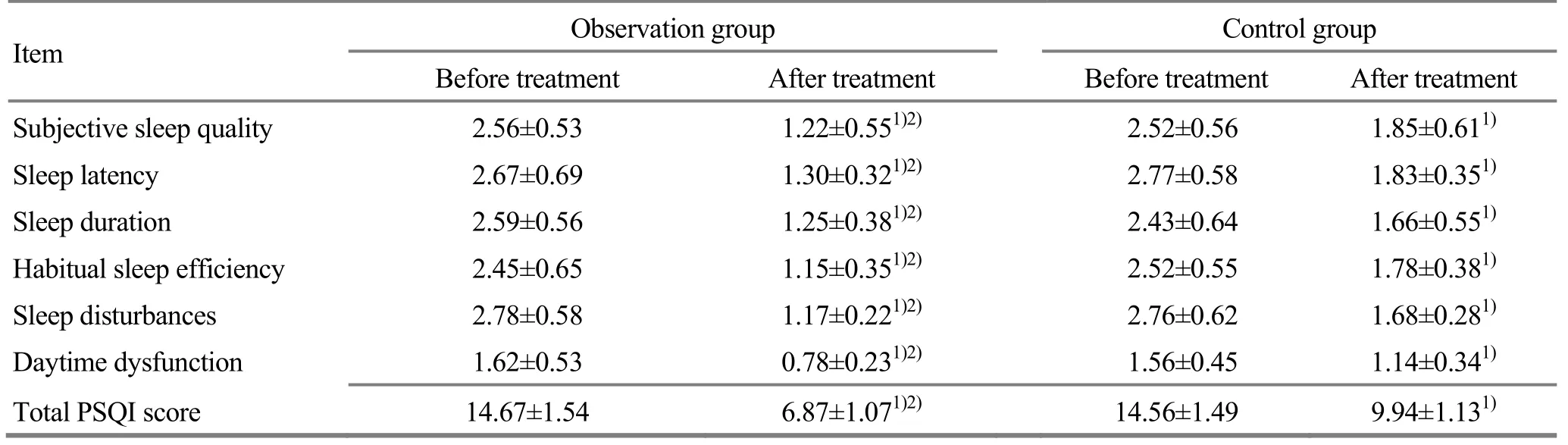
Table 4. Comparison of PSQI score (±s, point)
Note: Ⅰntra-group comparison, 1) P<0.05; inter-group comparison, 2) P<0.05
?
4 Discussion
Subhealth refers to a state between health and illness[5]. Clinical symptoms of subhealth include physical subhealth, mental subhealth, and social adaptable subhealth, in which sleep disorder pertains to physical subhealth. Subhealth insomnia refers to the presence of insomnia in subhealth state, while its severity and course have not reached the diagnostic criteria for non-organic insomnia[10]. It frequently manifests as difficulty falling asleep or difficulty returning to sleep after awakening (sleep latency>30 min), shallow sleeping, dreaminess, early awakening, discomfort after awakening, fatigue and daytime drowsiness[11]. Therefore, symptoms of subhealth may include insomnia, and long-term insomnia may in turn aggravate subhealth, creating a vicious circle.
Subhealth state pertains to pre-disease in TCM. TCM theory holds that the occurring of diseases is related to certain pathogenic factors which cause imbalance between yin and yang. While subhealth state is on the verge of the imbalance between yin and yang[5]. Waxing and waning of yin-yang is closely linked with sleep.According to TCM, imbalance of yin-yang is the root cause of subhealth insomnia.
Modern research holds that insomnia is caused by nervous and mental tension, and the subsequent influence on functional activities of the cortex. The pathogenic location is mainly the heart and brain[12].Through acupuncture treatment, immune functions can be recovered and boosted. Acupuncture also shows advantages in correcting mind-body imbalance and intervening subhealth state[13-15]. Guo D, et al[2]analyzed 84 modern literatures of acupuncture intervening subhealth insomnia, and the result showed that Baihui(GV 20), Sishencong (EX-HN 1), Shenmen (HT 7) on bilateral sides, Neiguan (PC 6), Sanyinjiao (SP 6) and Zusanli (ST 36) were mainly slected, possibly in combination with Back-Shu and Front-Mu points[16],with the purpose to regulate heart and mind, and harmonize spleen and stomach[2].
This study took acupuncture as an intervention method. For the control group, acupoints were selected based on literatures. For the observation group,abdominal acupuncture method was added on the basis of the conventional acupuncture. Abdominal acupuncture is a micro-needle system taking Shenque(CV 8) distributing qi hypothesis as the core theory.Through stimulating acupoints on abdominal region, it can regulate imbalance of Zang-fu organs to treat diseases[17]. Conventional meridian system is a feedback system. By stimulating acupoints on meridian, it can transmit stimulation to brain and facilitate the secretion of neurotransmitters. After a series of reactions, target organs can be activated and thus take effect. Modern research revealed the existence of the second brain, i.e.the gut brain[18]. Developed on the basis of conventional acupuncture system, abdominal acupuncture has created a Shenque (CV 8) regulating system which is comprised of two subsystems. One system is located on the superficial layer of abdominal wall and can regulate the whole body, and is called peripheral system.Another system is located deep in the abdominal wall and can regulate visceral organs, and is called visceral system[19]. The coordination of the two systems can regulate physical functions effectively. The possible mechanism of abdominal acupuncture may relate to the direct stimulation of gut-brain system and the effect of neurotransmitters on the target organs. Therefore,abdominal acupuncture has the merit of reducing intermediate links, and shortening the distance of regulating Zang-fu function and maximizing the adjustment effect. In the traditional meridian theory,the disease location is the heart but also linked with the liver, spleen and kidney. The liver stores blood, spleen governs blood and spleen and stomach are the origin of qi-blood generation. The kidney stores essence from the five Zang organs and connects with the heart;heart-qi descends to associate kidney. Normal functions of the five Zang organs can guarantee a calmed mind and spirit. In this study, Yinqiguiyuan [Zhongwan (CV 12),Xiawan (CV 10), Qihai (CV 6) and Guanyuan (CV 4)] in abdominal acupuncture were selected to control heart and lung, regulate spleen and stomach, tonify liver and kidney, and induce qi to its origin. These points can nourish the innate essence by supplementing the acquired essence[20]. Shangqu (KI 17), Qipang (Extra,located at 1.5 cun below the umbilicus and 0.5 cun lateral to the front midline) and Qixue (KI 13) on the left side are all located on the Kidney Meridian and have the function of connecting heart and kidney and regulating Zang-fu organs. Abdominal acupoints in this research started from the regulation of Zang-fu organs and also addressed local meridians, and such selection principle had the characteristic of regulating from the inside to the outside. It aimed to balance Zang-fu organs,qi-blood and yin-yang, to treat the root causes of the disease and improve sleep quality when alleviating fatigue.
Results in this study showed that after the treatment,the scores of MSSSHS and PSQI both dropped significantly, intra-group differences showed statistical significance (all P<0.05), and the scores of MSSSHS and PSQI in the observation group were lower than those in the control group (P<0.01, P<0.05). The total effective rate was higher in the observation group than that in the control group (P<0.05). These results showed that abdominal acupuncture should be effective for subhealth insomnia, and it can enhance the efficacy of conventional acupuncture.
Conflict of Interest
The authors declared that there was no potential conflict of interest in this article.
Acknowledgments
This work was supported by Project of Wuxi Municipal Commission of Health and Family Planning (无锡市卫生和计划生育委员会项目, No. CXTDJS006).
Statement of Informed Consent
Ⅰnformed consent was obtained from all individual participants included in this study.
Received: 15 October 2017/Accepted: 19 November 2017
猜你喜欢
杂志排行
Journal of Acupuncture and Tuina Science的其它文章
- Modern quantum theories and experimental achievements motivate new exploration of acupuncture in traditional Chinese medicine
- Application and exploration of suspended magnetic moxibustion cup for obesity
- Therapeutic efficacy observation on acupuncture for persistent allergic rhinitis
- Correlation analysis on clinical effects of acupuncture for elderly patients with sensorineural deafness and ear distending sensation
- Effect of Governor Vessel-unblocking and mindrefreshing acupuncture plus functional training on neural development in infants with brain damage
- Effects of acupuncture on ovarian blood supply and pregnancy outcomes in patients receiving assisted reproduction