Therapeutic efficacy observation on acupuncture for persistent allergic rhinitis
2018-09-12LiuPeng刘鹏ZhangBimeng张必萌ZongLei宗蕾HuZhihai胡智海ShouYin寿崟LiBingrong李冰融YuanLong袁龙XuSiwei徐斯伟YangYang杨洋ZhangKaiyong张开勇JiangHuiru蒋会茹
Liu Peng (刘鹏), Zhang Bi-meng (张必萌), Zong Lei (宗蕾), Hu Zhi-hai (胡智海), Shou Yin (寿崟), Li Bing-rong (李冰融),Yuan Long (袁龙), Xu Si-wei (徐斯伟), Yang Yang (杨洋), Zhang Kai-yong (张开勇), Jiang Hui-ru (蒋会茹)
Abstract Objective: To observe the clinical effect of acupuncture for persistent allergic rhinitis (PAR).Methods: A total of 154 PAR patients were randomized into a treatment group and a control group, 78 cases in the treatment group received acupuncture at meridian points, while 76 cases in the control group received acupuncture at non-meridian points. The treatment was done every other day, 3 times a week for a total 4 weeks. The total nasal symptom score (TNSS), the total non-nasal symptom score (TNNSS) and the rhinoconjunctivitis quality of life questionnaire (RQLQ)were measured before the treatment and after 2 weeks and 4 weeks of treatment, as well as 1 month and 3 months after the treatment to compare the clinical effect between the two groups.Results: After 4 weeks of treatment, the total effective rate in the treatment group was 92.3%, versus 76.3% in the control group, showing a statistically significant difference (P<0.05). Intra-group comparisons of TNSS, TNNSS and RQLQ scores after 4 weeks of treatment showed statistically significant differences (all P<0.05). Between-group comparisons of TNSS, TNNSS and RQLQ score after 4 weeks of treatment and in follow-up visits showed statistically significant differences (all P<0.05).Conclusion: Acupuncture is effective for PAR, and acupuncture at meridian points can produce a better effect than acupuncture at non-meridian points.
Keywords: Acupuncture Therapy; Rhinitis, Allergic; Acupuncture Points; Specificity of Acupoints; Quality of Life; Surveys and Questionnaires
Allergic rhinitis (AR) is an immunoglobulin E(IgE)-mediated atopic disorder that affects nasal mucosa,and is mainly manifested by rhinorrhea, sneezing, and nasal obstruction. AR can be sorted into intermittent AR(IAR) and persistent AR (PAR) according to Allergic Rhinitis and Its Impact on Asthma (ARIA)[1]. PAR is also called perennial AR that occurs throughout the year,and is common in teenagers. Clinical symptoms of PAR include paroxysmal nasal itching, succession of sneezing,rhinorrhea and nasal congestion and hyposmia, and such symptoms usually last for a long time with high relapse rate[2]. Otorhinolaryngology Head and Neck Surgery Groups in 11 domestic hospitals conduct a survey in 11 cities, during which the prevalence rate of AR was averaged at 11.1% but varied from 8.0% to 21.4%. The prevalence rate in the 11 cities in this survey appeared lower than that in American and European countries[3]. This study observed the effect of acupuncture on PAR, and the results are showed as follows.
1 Clinical Materials
1.1 Diagnostic criteria
It was based on the Diagnosis and Treatment Principle and Recommended Scheme for Allergic Rhinitis(2004, Lanzhou, China)[4].
History: By detailed inquiry of medical history, the attack time and inducing factor of symptoms, presence of asthma and severity of symptoms were evaluated.With the presence of at least 3 symptoms including itching, sneezing, rhinorrhea and congestion, and daily attack time accumulating to at least 0.5 h.
Examination: Nasal mucus appears pale, congested or swelling. Conjunctival congestion or edema or eyelid swelling in severe cases with hay fever. Positive eosinophilic granulocyte test in nasal secretion smear or conjunctiva blade. Positive allergen skin test, (++) or above for at least one allergen. IgE concentration in serum or nasal secretion was identified.
1.2 Inclusion criteria
Met the above diagnostic criteria and 2008 ARIA diagnostic criteria of PAR[1], moderate-severe degree;symptom lasted ≥4 d in a week and in succession of ≥4 weeks; aged between 18-60 years old; didn’t receive Western or Chinese medicine treatment related to allergic rhinitis in the recent 2 weeks; signed informed consent.
1.3 Exclusion criteria
Non-PAR patients; suffering from influenza in the previous 2 weeks or usage of antibiotics after acute nasosinusitis; acute onset of chronic nasosinusitis;history of asthma and usage of anti-allergic medication in the recent 2 weeks; received Western or Chinese medicine treatment related to allergic rhinitis in the recent 4 weeks; women during pregnancy or lactation;those with serious tuberculosis, hepatitis, nephrotic syndrome or cardiovascular diseases; bad compliance.
1.4 Dropout criteria
Withdrawn from treatment upon self-decision;unblinding caused by improper reason; loss of contact during follow-up visit.
1.5 Rejecting criteria
Cases didn’t meet the inclusion criteria or met exclusion criteria; against treatment protocol or using medication during the experiment.
1.6 Statistical method
All data were processed by SPSS 19.0 version software. Measurement data of normal distribution were described by mean ± standard deviation (±s)and analyzed by t-test. The enumeration data were analyzed by using Chi-square test. A P-value less than 0.05 indicated a statistical significance.
1.7 General data
Ethical approval for this study was granted by the Institutional Review Board of Shanghai First People’s Hospital, Shanghai Jiao Tong University School of Medicine. The ethic code is No. 25 (2014).
Cases conforming to the diagnostic and inclusion criteria in this study were enrolled from Acupuncture Outpatients of Shanghai First People’s Hospital,Shanghai Jiao Tong University School of Medicine,Yueyang Hospital of Integrated Traditional Chinese and Western Medicine, Shanghai University of Traditional Chinese Medicine and Shanghai TCM-integrated Hospital, Shanghai University of Traditional Chinese Medicine from August of 2014 to December of 2016. A total of 160 cases were included. By simple randomization method, the patients were divided into a treatment group and a control group, 80 in each group.Two cases in the treatment group and 4 cases in the control group dropped out due to job transfer or visiting relatives, so the actual cases were 154. In comparison of the gender, age and duration, the differences showed no statistical significances (all P>0.05), indicating the comparability (Table 1).
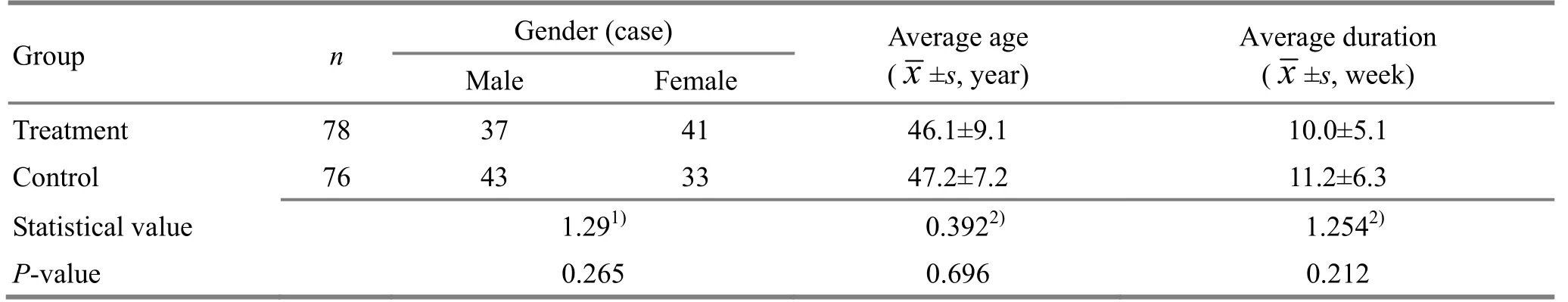
Table 1. Comparison of general data
2 Therapeutic Methods
2.1 Treatment group
Acupoints: Yintang (GV 29), Shangxing (GV 23),bilateral Yingxiang (LI 20), Hegu (LI 4), Sibai (ST 2),Zusanli (ST 36) and Taixi (KI 3).
Methods: After routine sterilization, disposable needle of 0.20 mm in diameter and 40 mm in length was used to insert upward at Yingxiang (LI 20) along nasolabial fold for 0.5 cun, perpendicularly at Zusanli(ST 36) for 1.2 cun, obliquely at Hegu (LI 4) towards carpus for 1.2 cun, at Sibai (ST 2) towards pupil under skin for 0.5 cun, perpendicularly at Taixi (KI 3) for 0.8 cun, and at Shangxing (GV 23) towards forehead for 0.5 cun. Even reinforcing-reducing lifting and thrusting manipulation was used upon qi arrival. Retained the needle for 30 min each time, and the treatment was done every other day, 3 times in a week for a total of 4 weeks.
2.2 Control group
Non-acupoint stimulating locations: 0.8 cun dorsalateral and 0.5 cun below Yingxiang (LI 20), 0.5 cun above Hegu (LI 4) close to the first metacarpal bone, 0.5 cun lateral to Sibai (ST 2), 0.5 cun on the upper left of Yintang (GV 29), 0.5 cun lateral left of Shangxing (GV 23),1.5 cun lateral to Zusanli (ST 36) and 1 cun above Taixi(KI 3).
Method: After routine sterilization, disposable filiform needle of 0.20 mm in diameter and 40 mm in length was inserted by 1-3 mm into skin with the help of tube, no manipulation, retained for 30 min. The treatment was done every other day, 3 times in a week for a total of 4 weeks.
3 Therapeutic Efficacy Evaluation
3.1 Observation items
3.1.1 Total nasal symptom score (TNSS)[4]
Four symptoms including congestion, sneezing,itching and rhinorrhea are measured. The score of each question is divided into five levels. 0 point: no symptom;1 point: mild symptom; 2 point: moderate symptom; 3 points: severe symptom; 4 points: very severe symptom.The total score of these four sections is considered as the TNSS score. The maximum TNSS score is 16 points,and a higher score indicates a more serious condition.Visit times: before treatment, after 2 weeks and 4 weeks of treatment, and 1 month and 3 months after the treatment.
3.1.2 Total non-nasal symptom score (TNNSS)[5]
Postnasal drip, nasal or ocular itching, nasal or maxillary pain, headache and tears are measured: 0 point: no symptom; 1 point: presence of symptom. The total score of all sections is TNNSS, at a maximum of 5 points.
3.1.3 Rhinoconjunctivitis quality of life questionnaire(RQLQ)[6]
The RQLQ has 28 questions in 7 domains: activity limitation, sleep problems, nose symptoms, eye symptoms, non-nose/eye symptoms, practical problems and emotional function. Patients recall how bothered they have been by their rhinoconjunctivitis and to respond to each question on a 7-point scale:0=not impaired at all; 1=almost no impaired; 2=mildly impaired; 3=moderately impaired; 4=quite impaired;5=very impaired; and 6=severely impaired. The overall RQLQ score is the sum of all 28 responses. The maximum score is 168.
3.2 Standard for therapeutic effect
The improvement rate was calculated according to TNSS score before and after 4 weeks of treatment.Improvement rate = (TNSS score before treatment –TNSS score after treatment) ÷ TNSS score before treatment × 100%. The improvement rate was used for therapeutic effect evaluation.
Marked effective: Improvement rate ≥66%.
Effective: Improvement rate ≥26%, while <66%.
Invalid: Improvement rate <26%.
3.3 Results
3.3.1 Comparison of clinical effect
After 4 weeks of treatment, the total effective rate was 92.3% in the treatment group, versus 76.3% in the control group, and between-group comparison showed a statistical significance (P<0.05), indicating a higher effective rate in the treatment group (Table 2).
3.3.2 Comparison of TNSS, TNNSS and RQLQ score
The scores of TNSS, TNNSS and RQLQ after 2 weeks and 4 weeks of treatment and at the 1-month and 3-month follow-up visits all showed statistical significances when compared with those before treatment (all P<0.01), indicating the treatment methods in both groups are effective. Before the treatment, the between-group comparisons of TNSS,TNNSS and RQLQ scores showed no statistical significances (all P>0.05), indicating the comparability.The between-group comparisons showed lower TNSS,TNNSS and RQLQ scores after 2 weeks and 4 weeks of treatment and at the 1-month and 3-month follow-up visits in the treatment group (all P<0.01), indicating a better therapeutic effect in the treatment group(Table 3).
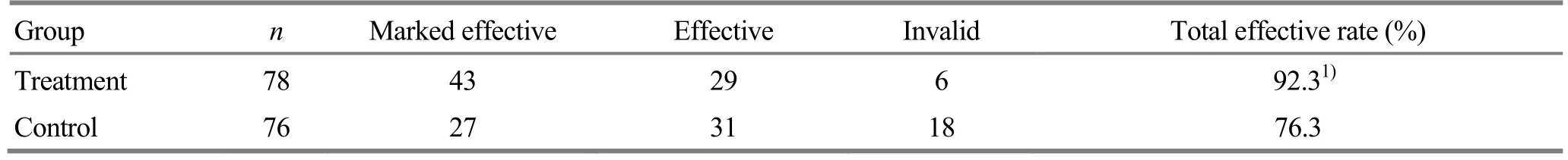
Table 2. Comparison of clinical effect between the two groups (case)
Table 3. Comparison of TNSS, TNNSS and RQLQ scores before and after the treatment (±s, point)

Table 3. Comparison of TNSS, TNNSS and RQLQ scores before and after the treatment (±s, point)
Note: Compared with the same group before the treatment, 1) P<0.01; compared with the control group at same time point, 2) P<0.01
?
4 Discussion
PAR pertains to Bi Qiu (rhinallergosis) in traditional Chinese medicine. Ancient medical practitioners thought that such disease was related to the impairment of the lung, spleen and kidney. In modern view[7-9], PAR is differentiated as deficiency in root and excess in manifestations. The weakness of lung, spleen and kidney is the root cause, while external contraction of evil is the external cause. In modern medicine, the pathogenesis of AR is linked with gene and environment,and the scholars have discovered multiple genetic locus related to AR[10]. Some also raised the hygiene hypothesis[11]. Treatments of AR include environment control, medication, immune therapy and health education[12]. Immune therapy is the most common treatment nowadays with good safety performance[13].Common medication includes glucocorticoid,anti-histamine, anti-leukotriene and intranasal anticholinergic[14]. Nevertheless, 40% patients are reported not satisfied with the current medical treatment[15].
Acupuncture is safe and effective for PAR. Common treatment method includes acupuncture, moxibustion,cupping, acupoint plaster, acupoint injection, acupoint embedding and combination of acupuncture and medication[16]. Frequently chosen acupoints include Yingxiang (LI 20), Yintang (GV 29), Sibai (ST 2), Hegu(LI 4), Fengchi (GB 20), Fengfu (GB 16) and Zusanli(ST 36)[17-18]. Our study took meridian-point acupuncture as the treatment approach. Yingxiang(LI 20), Sibai (ST 2), Shangxing (GV 23) and Yintang(GV 20) locate on face and have the function of dispersing head wind and clear orifices. Zusanli (ST 36)is used for supplementing ‘earth’ to generate ‘metal’.Hegu (LI 4) is used to treat facial problems and can be used to open nasal cavity and facilitate lung qi. The long duration will cause kidney deficiency, and Taixi (KI 3) is the Yuan-Primary point of the Kidney Meridian. It can consolidate the root and propel the evil. Patients in the control group received non-meridian-point shallow-penetrating treatment.
The results have shown acupuncture had a good therapeutic effect for PAR, while non-meridian-point shallow-penetration also had certain effect, but less effective than the former treatment. Some research showed non-meridian-point stimulation also had some effects[19-21]. We suspect such effect might relate to the theory of cutaneous regions, while its mechanism requires further investigation.
Conflict of Interest
The authors declared that there was no potential conflict of interest in this article.
Acknowledgments
This work was supported by Project of Shanghai Municipal Commission of Health and Family Planning (上海市卫生和计划生育委员会项目, No. CC-3-3051);Guidance Project of Traditional Chinese Medicine of Shanghai Science and Technology Committee (上海市科学技术委员会科研计划中医引导类项目, No.17401932200); Projects of Shanghai Science and Technology Committee (上海市科学技术委员会项目,No.14401933100, No.16401934000).
Statement of Informed Consent
Ⅰnformed consent was obtained from all individual participants or their relatives in this study.
Received: 15 September 2017/Accepted: 13 October 2017
猜你喜欢
杂志排行
Journal of Acupuncture and Tuina Science的其它文章
- Modern quantum theories and experimental achievements motivate new exploration of acupuncture in traditional Chinese medicine
- Application and exploration of suspended magnetic moxibustion cup for obesity
- Correlation analysis on clinical effects of acupuncture for elderly patients with sensorineural deafness and ear distending sensation
- Effect of Governor Vessel-unblocking and mindrefreshing acupuncture plus functional training on neural development in infants with brain damage
- Effects of acupuncture on ovarian blood supply and pregnancy outcomes in patients receiving assisted reproduction
- Observation of therapeutic effects of point application at Shenque (CV 8) plus moxa-salt hot compress for prevention of gastrointestinal adverse reactions after chemotherapy for non-Hodgkin lymphoma