Echocardiography in centenarians: characteristics, utility and follow-up
2018-08-09JorgeBrenesSalazarJaimedelaFuentePunnaiahMarellaHariChalikiChristopherScottHeidiConnollyRogerClick
Jorge A Brenes-Salazar, Jaime de la Fuente, Punnaiah Marella, Hari Chaliki, Christopher Scott,Heidi M Connolly, Roger L Click
1Department of Cardiovascular Diseases, Mayo Clinic, Rochester, USA
2Department of Internal Medicine, Mayo Clinic, Rochester, USA
3Department of Cardiovascular Diseases, Mayo Clinic, Arizona, USA
4Division of Biostatistics, Mayo Clinic, Rochester, USA
Abstract Background Echocardiography has been shown to be a valuable resource in the diagnosis of many cardiac conditions, and can be used in all age groups, from the fetus to the oldest old. In the context of an increasingly aging population, the impact and utility of echocardiography in centenarians is largely unknown. This study is to determine whether echocardiography in centenarians aids in making clinical patient management decisions. Methods A retrospective review of echocardiograms from 1986 to 2014, at two affiliated tertiary centers, in individuals who were 100 years or older at the time of the examination. Patient and echocardiogram characteristics, management decisions based on echocardiography, and mortality were documented. Results 114 centenarians had echocardiograms, with ages ranging from 100 to 107 years (101 ± 1.4 years). In 82 of the centenarians evaluated (72%), no changes in management occurred as a consequence of the echocardiogram. From all management changes directly related to the echocardiogram, 81% (n = 26) of these corresponded to medication adjustments; interventional or surgical procedures followed the echocardiogram only in 4% (n = 5) of the total number of centenarians.Echocardiogram-based changes in management were only significant in patients that were referred for congestive heart failure (P = 0.02).After the echocardiogram was performed, 1-month and 1-year mortality were 15% and 47%, respectively. The median survival after the echocardiogram was obtained was 13 months (range 0.03 to 145 months), with no difference if there was a change or no change in management (P = 0.21). Conclusions Among centenarians undergoing echocardiography, despite additional diagnostic information, echocardiograms in centenarians influence management in a minority of cases, most commonly in the form of medication changes for treatment of heart failure. A significant proportion of centenarians are deceased within a year of undergoing echocardiographic assessment. These findings may question the overall utility of echocardiography in these late survivors.
Keywords: Centenarian; Echocardiography; Geriatric
1 Introduction
In the context of an increasingly aging population, cardiovascular diseases continue to be the number one cause of death in adults over 65 years of age in the United States.[1–3]Advancing age is per se one of the most important nonmodifiable cardiovascular risk factors. Within the elderly population, the centenarian sub-group (≥ 100 years old) has experienced a 66% relative increase between 1980 and 2010.[4]Thus, it is now much more common to see these centenarian patients in clinical practice.[5]Based on population studies, centenarians demonstrate different clinical characteristics, compared to “younger” elderly cohorts, with decreased prevalence of diabetes mellitus and a more favorable metabolic cardiovascular risk profile.[6–9]This has prompted interest to better understand such late survivors.[10–13]
The study of cardiac structure and function in centenarians using echocardiography has been limited.[10,11]Furthermore, no previous studies have evaluated the role of echocardiography on patient management decisions. This is of particular importance due to increasing health-care costs,emphasis on cost-effectiveness, and achieving high value care.[14–16]
The primary aim of this study was to provide insights into the clinical value of echocardiography in centenarians in terms of management and decision-making.
2 Methods
The study was approved by the Mayo Clinic Institutional Review Board. We performed a retrospective review on all patients evaluated at the Mayo Clinic Rochester, Minnesota and Mayo Clinic Scottsdale, Arizona between October 31,1986, and October 1, 2014, who underwent echocardiograms, with an age of 100 years or more at the time of examination. If more than one echocardiogram was performed,only the first one was included. At the time of retrospective extraction, patient demographic variables at time of echocardiogram were collected including: age, gender, and residence. Concurrent past medical history of the following diseases: coronary artery disease, heart failure, atrial fibrillation, severe valvular disease, stroke and dementia were also recorded. Patient location (inpatient versus outpatient)at the time of the echocardiogram was included as well.
Referring ICD-9 codes were documented. Follow up after the echocardiogram included echocardiogram related complications, date of death, and any management changes based on the imaging study. Management changes were defined as medication adjustment, changes in monitoring,interventional procedures, or surgery. When applicable, the time from the echocardiogram to death was recorded.
2.1 Echocardiography
Patients underwent 2D and Doppler transthoracic (TTE)or transesophageal echocardiography (TEE) according to standard American Society of Echocardiography guidelines.[17,18]Left and right ventricles were assessed, along with function, with multiple orthogonal views. The systolic function was calculated from end diastolic and end-systolic ventricular diameters. Right ventricular systolic pressure(RVSP) was determined by the modified Bernoulli equation(4v2+ estimated right atrial pressure, where v = tricuspid regurgitation velocity). Right atrial and ventricular sizes as well as right ventricular function were measured on an ordinal qualitative scale when available by experienced cardiologists. Stenosis of the aortic or mitral valve was calculated via visualization of valve area and measuring high-velocity flow across the valve by Doppler. Regurgitation in all four heart valves was assessed by color flow Doppler. Diastolic function was also assessed using end-diastolic Doppler signals in concordance with established guidelines.[19]
2.2 Statistical analysis
Statistical analyses were performed using SAS version 9.4 (SAS Institute Inc., Cary, North Carolina). Continuous variables were presented as mean ± standard deviation. The association of changes in management based on the echocardiogram with demographic variables, location and referral of echocardiogram, hemodynamic data from echocardiography, and comorbidities was assessed using the Pearson chi-square test. Trends across time were tested using the Cochran-Armitage trend test. Kaplan-Meier survival curves were constructed to illustrate the survival in this cohort and to compare those centenarians that had a management change versus no management change during the follow-up period. The log-rank test was used to compare survival among these two groups. All tests were two-sided and P-values < 0.05 were considered statistically significant.
3 Results
3.1 Patient characteristics
From 10/31/1986 to 10/01/2014 a total of 140 echocardiograms were performed in 114 patients ≥ 100 years of age.Of the first echocardiograms performed each patient, 111(97%) of the echocardiograms were TTEs while the remaining 3 (3%) were TEEs. Eighty-two patients were female (72%) and 32 patients were male (28%), with ages ranging from 100 to 107 years (mean 101 ± 1.4 years). Most common reasons for echocardiographic referral included:heart failure (28%), dyspnea (17%), aortic stenosis (7%),acute coronary syndromes (7%) and atrial fibrillation (6%).The most common chronic comorbidities included hypertension (67%), heart failure (60%), and coronary disease(46%). Less than half of the sample population (39%) resided in assisted-living facilities at the time of the echocardiogram, while the remaining patients (61%) lived independently. Patient demographics are summarized in Table 1.During the three decades analyzed, the only significant trends noted in patient characteristics were a progressiveincrease in hypertension (P ≤ 0.001) and a progressive decreasing trend (P = 0.03) in heart failure.
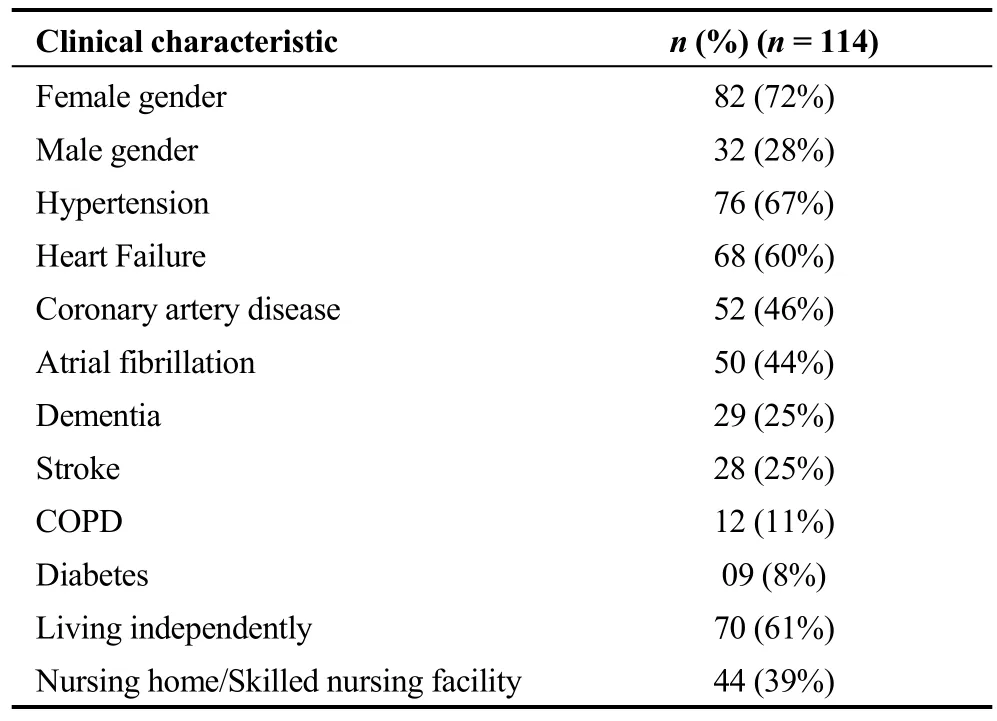
Table 1. Clinical characteristics of patients ≥ 100 years of age who underwent echocardiographic evaluation.
3.2 Echocardiographic characteristics
Eighty-three (73%) of the echocardiograms analyzed were performed in the inpatient setting. Echocardiographic findings included normal left ventricular ejection fraction(EF), greater or equal to 55%, in 82 patients (72%), moderate reduction, EF between 54% and 30% in 16 patients(14%) and severe reduction, EF less than or equal to 30%,in 16 individuals (14%). Of the 76 centenarians in whom diastolic function was assessed, 10 (13%) were found to have severe diastolic dysfunction. Ninety-two centenarians(81%) had varying degrees of pulmonary hypertension(mean RVSP 54 mmHg, range 34 to 108 mmHg) defined by RVSP over 30 mmHg; moderate to severe right systolic dysfunction was present in 8 patients (8%). The most common types of severe valvular disease were aortic stenosis in 18 patients (16%) and tricuspid regurgitation in 14 patients(12%). Echocardiographic characteristics are summarized in Table 2. No complications were attributed to any of the echocardiograms performed.
3.3 Changes in management
Eighty-two (72%) of the centenarians evaluated had no changes in management in relation to the echocardiogram.Of the remaining 32 (28%) patients, the vast majority of changes corresponded to medication adjustments in 26 individuals (81%); in 5 patients (16%) changes involved interventional or surgical procedures; while changes in level of care or monitoring were seen only in 1 centenarian (3%),see Figure 1.EF: ejection fraction; RVSP: right ventricular systolic pressure; RV:right ventricle.*Totaln= 76, due to indeterminate or missing diastolic function calculation.

Table 2. Echocardiogram characteristics of the centenarians.
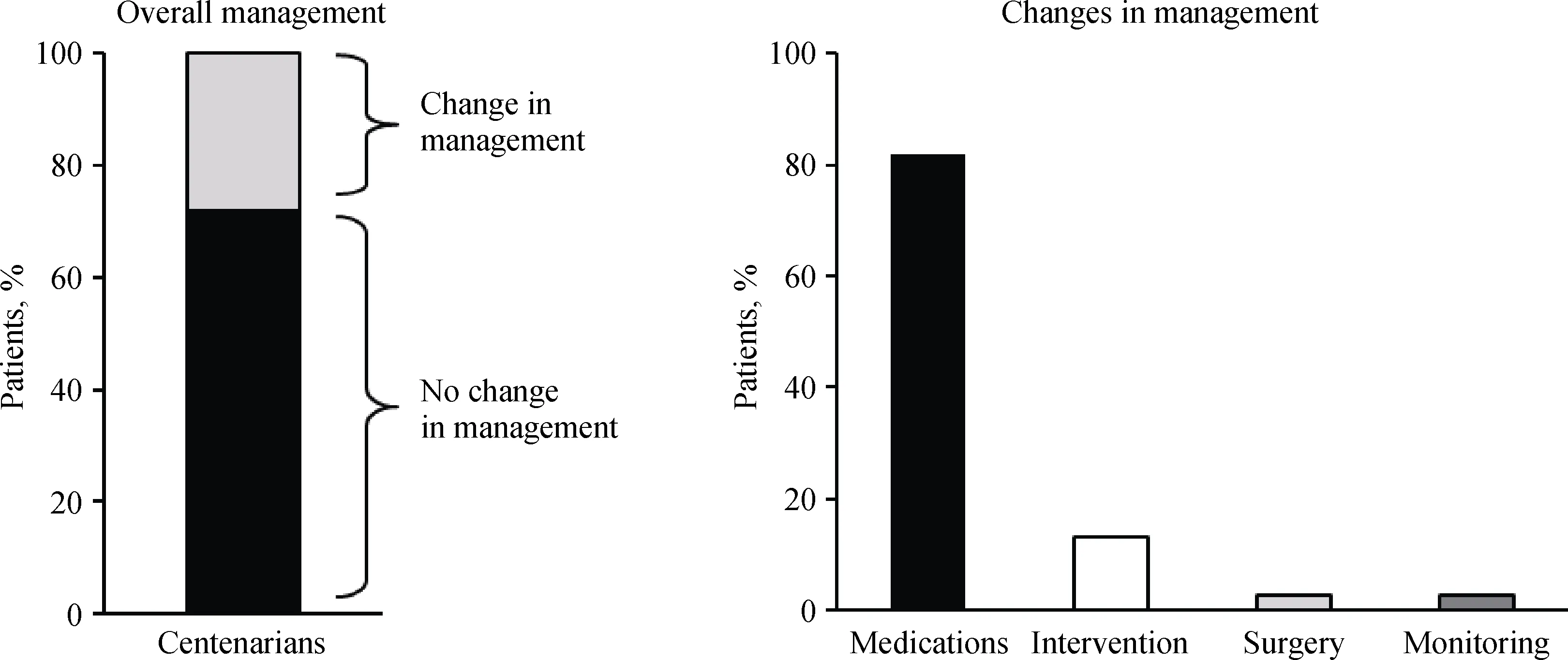
Figure 1. Analysis of the changes in management after echocardiogram. No change in management in 82 (72%) centenarians. Majority of the changes involved medication.
Echocardiogram-based changes in management showed no significant differences in relationship to gender (P =0.16), type of echocardiogram (TTE vs. TEE, P = 0.84),inpatient or outpatient setting (P = 0.21) or decade of performance (P = 0.12). Echocardiogram changes did not differ based on referral diagnosis including: aortic stenosis (P =0.68), atrial fibrillation (P = 0.19), dyspnea (P = 0.85),myocardial infarction/non ST-elevation myocardial infarction (P = 0.84), and syncope (P = 0.32). The only referral diagnosis that demonstrated a significant association with management changes (P = 0.02) was congestive heart failure (CHF), with the majority being medication changes (P =0.04).
3.4 Survival after echocardiogram
Of the 114 patients that had an echocardiogram per-formed, 96 (84%) were known to be deceased at the completion of the study. One-month and 1-year mortality after the echocardiogram were 15% and 47%, respectively. The overall survival after the echocardiogram is depicted in Figure 2A. Median life expectancy was found to be 13 months(range 0.03 to 145 months). Figure 2B depicts no difference in patient’s mortality whether there was a change or not in management, P = 0.21.

Figure 2. Survival after echocardiogram. (A): overall survival after echocardiogram, one-month and 1-year mortality after the echocardiogram were 15% and 47%, respectively; (B): survival after echocardiogram by presence or absence in change in management, No significant change in mortality.
4 Discussion
The most important finding of our study is that in centenarians and beyond, echocardiography influences medical-decision making and management only in a minority of cases. It is important to underscore that even in such discrete occasions, the only significant changes occurred in those seniors who presented for care due to CHF (P = 0.02). Despite a recent abstract reporting appropriate use of the echocardiography in most nonagenarians,[20]the value of this test could be limited, based on the lack of impact on overall care in such patients. In a health care system where the safest,non-invasive tests are preferred, increasing access and availability of echocardiography can evidently generate additional financial burdens.[14–16,21]
The intermediate and long-term value of echocardiography in this aged cohort is also questionable, as our Kaplan-Meier curves showed no difference in mortality whether there was a change or not in management, even in heart failure, where medications for systolic dysfunction have shown to improve survival. Nevertheless, this could possibly be explained by expected demographic survival already compromised by a host of extra-cardiac co-morbidities,including frailty and debility.
In terms of patient demographics (Table 1), we noted a significant increase in the prevalence of hypertension (P ≤0.001) across the three decades of the study, perhaps related to stricter definitions and lower cut-offs, particularly after the landmark HYVET trial in the early 2000 s.[22]This rising awareness and treatment of hypertension over time could also potentially explain the decreasing prevalence of heart failure seen within our cohort.
To date, this is the largest group of centenarians with an accurate echocardiographic description, with only two other similar studies found in the literature.[10,11]Most centenarians had a normal ejection fraction (72%), left (88%) and right (69%) atrial enlargement, some degree of pulmonary hypertension (81%) and valve abnormalities. The normal EF emphasizes the notion of preservation of contractile function with aging, in contraposition to diastolic dysfunction being one of the earliest hallmarks of myocardial aging,via ventricular-vascular stiffening and myocyte loss as well as replacement with fibroblasts, seen in the elderly.[23–28]
Our investigation confirmed aortic stenosis to be the most common severe valvular lesion in this age group, with 16% of centenarians affected. This was higher than the series from Sadiq, et al. 11% of hospitalized centenarians, and Martínez-Sellés, et al. outpatient centenarians of 5%. Nevertheless, the number of patients with severe aortic (2%) and mitral regurgitation (7%) were similar to those described previously.[11]Perhaps somewhat surprising was to find tricuspid regurgitation as the second most common type of severe valvular disease, seen in 12% of centenarians, a prevalence that was previously unreported in the literature;this typically poorly defined valvular disease has been associated with excess mortality and morbidity in other age groups.[29]
Pulmonary hypertension was identified in a significant number of centenarians (81%), presumably due to the vascular changes of an ageing population and its effect on the pulmonary vasculature, as well as contributions from increased ventricular filling pressures in the setting of diastolic impairment and tricuspid regurgitation.[28,30,31]This was comparably higher than in previous studies, which reported some degree of pulmonary hypertension in about 55% of their cohorts.[10,11]A fundamental limitation is that most of these patients never had invasive hemodynamic assessments, such as right heart catheterizations, to confirm and provide insight on the etiology of the elevated pulmonary artery systolic pressures by echocardiography.
We would like to highlight several limitations in our study, with the main one being its retrospective nature. Accurate assessment of diastolic function has only been reported in a methodological and consistent way over the last two decades as well, and therefore our results may not provide accurate representation of the whole cohort, particularly the earlier echocardiograms. Very few TEEs were performed (n = 3), perhaps with a referral bias given the need for conscious sedation. In addition, the sample of patients of this study, though representative of the centenarians in the United States today,[4]cannot be extrapolated to represent all centenarians due the data being collected from only two tertiary referral centers. In addition, we did not have a comprehensive, geriatric assessment of function of these patients.
Our data demonstrates that despite providing additional information, echocardiograms in centenarians rarely influence clinical management. A significant proportion of centenarians die within a year of undergoing imaging, which adds to the limited impact of echocardiography in these late survivors.
杂志排行
Journal of Geriatric Cardiology的其它文章
- Heterogeneous genetic architecture by gender for precision medicine of cardiovascular disease
- Sphingosine 1 phosphate receptor-1 (S1PR1) signaling protects cardiac function by inhibiting cardiomyocyte autophagy
- Association between baseline platelet count and severe adverse outcomes following percutaneous coronary intervention
- Optimal timing of staged percutaneous coronary intervention in ST-segment elevation myocardial infarction patients with multivessel disease
- Predictors of long-term outcome in patients with biopsy proven inflammatory cardiomyopathy
- Persistent ductus arteriosus in old patient with atrial fibrillation
