开窗支架治疗慢性主动脉夹层远端破口的现状
2018-07-10孟庆友
孟庆友
(苏州大学附属第一医院 心血管外科/苏州大学心血管病研究所,江苏 苏州 215006)
主动脉夹层是一类灾难性疾病。外科手术创伤巨大,血管介入技术近年快速发展,胸主动脉瘤腔内修复术(TEVAR)现在已经成为急性B型主动脉夹层的一线治疗方式,主要是封堵近端第一破口,假腔内血栓形成,真腔扩大。但约30%远端会发生假腔的瘤样扩张[1-2],IRAD研究甚至发现有高达62.7%的扩张率[3]。远端破口是主要危险因素。因此,如何处理慢性夹层的远端破口成为主动脉夹层治疗的重要课题。开窗支架是处理此问题方案之一,近年在少数大中心开始开展,有较好的临床效果。本文旨在探讨慢性主动脉夹层远端破口处理的相关问题,以及开窗支架应用的思路和实践。
1 慢性主动脉夹层远端破口处理的必要性及适应证
1.1 必要性
主动脉夹层往往具有多破口,在急性期主要针对近端的破口处理,旷置远端破口,多数会闭合。近年在对TEVAR术后的长期随访中发现,远端破口对预后和主动脉的重塑起着重要作用。仅封闭夹层近端裂口不能有效降低假腔内压力、促进假腔内血栓化及真腔的良性重构[4]。并且TEVAR术后患者的远期生存率会因为假腔内血液反流及假腔内血栓化不全而降低[5-6]。Sueyoshi等[7]发现假腔内持续存在血流是真腔是否改变的唯一危险因素。所以只有封闭全部裂口才能达到理想的治疗效果[8-9]。Kim等[10-11]在一系列研究中发现,只有二次干预,真腔才能有效增加。Thrumurthy等[12]综述分析发现TEVAR术后有0~60%者需再次处理远端破口。因此,远端破口的处理对于夹层的整体治疗效果有积极重要意义[13-14]。主动脉夹层腔内治疗指南[15]也明确建议远端破口位于肾动脉以上且破口较大者应与近端破口同期修复。
相较于急性和亚急性主动脉夹层,慢性主动脉夹层全程瘤样病变,而且远端破口较多,流量都很大,夹层内膜片纤维化程度高,甚至钙化,重塑性差,真腔受压明显。因此主张封堵所有远端破口,从而达到假腔完全血栓化、主动脉良性重塑,既可以防止远端夹层动脉瘤破裂,也可以提高远端脏器血供[16-18]。所以对其远端所有破口处理有其必要性。
1.2 适应证
仍存在很大争议,但有以下几点共识:出现相关临床症状,主动脉瘤样扩张(直径>5.5 cm),夹层快速增大(速度>10 mm/年),真腔受压明显,影响脏器灌注。国内常光其等[19]主张对以下情况进行一期或多期腔内封闭所有裂口:⑴ 破口大,假腔血流多且夹层扩张明显;⑵ 多个破口形成多个互不相通的夹层;⑶ 封闭夹层近端破口后即时造影远端破口血流明显增加;⑷ 一期封闭近端破口随访发现远端破口仍扩大,或夹层扩张每年超过5 mm。
2 慢性主动脉夹层远端破口处理的困难[20-21]
2.1 无良好锚定区
慢性主动脉夹层远端破口所形成的夹层动脉瘤多是Stanford A或B型经药物保守治疗,或外科手术,或腔内修复术后形成,开窗支架所需的近、远端锚定区多为不健康锚定区,和真性动脉瘤有较大区别。腹腔干动脉以上主动脉,即近端锚定区多是夹层段动脉,开窗支架往往多需延长到原支架的位置,实现完全封堵。远端锚定区往往需到腹主动脉远段,甚至髂总动脉,髂外动脉[22]。
2.2 真腔狭小
慢性主动脉夹层远端多表现真腔狭小,并且多倾斜,开窗支架展开困难,同时在开窗支架释放后在其内实现超选分支动脉困难。
2.3 主动脉夹层远端裂口多累及内脏血管
慢性主动脉夹层远端破口所在位置难以处理[23],并且隐蔽,内脏分支区约占49%~88%。
2.4 内脏分支动脉开口假腔或伴分支动脉夹层
慢性主动脉夹层远端破口累及分支动脉时,可造成分支动脉开口假腔,夹层有时可延至分支动脉远端。
3 慢性主动脉夹层远端破口处理方法
传统外科手术仍是主要治疗手段,随着腔内技术的发展及器材的更新,腔内修复逐渐作为一种治疗的选择。对于破口位于腹腔干动脉上方1 cm,或肾动脉下方1 cm,可采用直管式覆膜支架直接封堵,甚至可牺牲腹腔干动脉。破口位于内脏分支动脉区时,可尝试以下方法:⑴ TEVAR联合裸支架技术。即petticoat(provisional extension to induce complete attachment)技术,在主动脉覆膜支架的远端植入裸支架,扩大真腔,促进主动脉良性重塑,裸支架的网眼可供内脏分支动脉血供[24]。但目前尚不能肯定此技术能够促进主动脉良性重塑[25],而且裸支架本身也不能封堵破口,对于破口较大者不能达到理想的疗效。⑵ 假腔填塞技术。即AFTER(aortic false lumen thrombosis induction by embolotherapy)技术,在假腔内填塞栓塞材料,促进假腔血栓形成。可用的材料有弹簧圈、蛋白胶、封堵器、滤器、可分离球囊、髂动脉封堵器等[26]。此技术有一定疗效,但由于假腔较大,填充不全,而且有异位栓塞风险。而且此法不适用于内脏分支动脉起自假腔的情况。⑶ 假腔填塞联合裸支架技术。为了避免填充材料移位,用裸支架固定 。同时减少填充材料,节省费用,更好地使真腔重塑。⑷ 烟囱技术。该技术多用在主动脉瘤,较少用在多破口的主动脉夹层。⑸多层裸支架。是一种探索的技术,争议仍然较大。⑹ 内脏分支动脉覆膜支架植入(spotstent-graft)。对于远端破口位于分支动脉内或贴近分支动脉者,或分支动脉由假腔供应者,将覆膜支架一端放在主动脉真腔内,一端放在分支动脉内,可以较远。既封堵了破口,又保持了相应分支动脉血流。Bel等[27]首次报道了这一技术,后Kim等[28]和Evangelista等[29]相继报道了该技术,临床效果较好。笔者也应用此技术处理1例破口在肾动脉附近者,国内其他一些学者在会议上有相似报道。但总体此技术应用例数较少,也存在支架脱落、移位风险。⑺ 开窗型覆膜支架植入。在覆膜支架上开槽或开窗,对准分支动脉,以保证分支血管的血供。此技术一出现即显示其先进性。
4 开窗支架处理慢性主动脉夹层远端破口
开窗支架主要用于治疗肾周的真性动脉瘤,对于慢性主动脉夹层来说,需在狭小的真腔内植入支架,并超选内脏分支动脉,这都是技术的难点。但一些学者也开始探索,也取得了较好效果。Anderson等[30]首先应用定制的开窗治疗慢性主动脉夹层远端破口。Oikonomou等[31]报道了一组开窗/分支型覆膜支架治疗慢性主动脉夹层远端破口,17例中技术成功率100%,围手术期病死率2例(11.8%),无截瘫,随访12个月,无动脉瘤相关死亡,再介入3例(17.7%)。Kitagawa等[32]报道了30例,无死亡,无截瘫。Spear等[33]多次报道,最近的报道了24例慢性主动脉夹层远端破口采用开窗/分支支架治疗,技术成功率100%,截瘫1例,无动脉瘤相关死亡。3D打印技术飞速发展,也为定制支架广泛应用于临床提供了更大的可能性[34]。但由于解剖的特殊性,我们要客观看待此技术在这一类疾病中的应用。各种新的图像软件的开发、3D融合技术都为此项技术的开展提供便利[21]。
5 思路及实践
笔者应用改建开窗支架治疗慢性主动脉夹层远端破口26例,根据经验并结合文献总结开窗支架应用在慢性主动脉夹层远端破口的治疗,为克服以上困难,总结出以四字“开”、“凿”、“疏“、“扩”概括的思路,并相应实践。
5.1 开
包括“小开”和“大开”。“小开”就是在主动脉原有破口的基础上,用球囊扩大破口,使得真假腔的压力相对平衡,使得狭小的真腔扩大,假腔减小。应用此方法处理3例,均取得良好的效果。“大开”就是真假腔融合技术,应用cheese wire技术撕开内膜片,使得真假腔融合,从而形成动脉瘤。再在融合的腔内植入开窗支架,既解决了真腔狭小的问题,也摆脱了支架由于内膜片的存在,不能完全贴壁的困境。此种技术Kos等[35]首次应用到4例急性夹层灌注不良的病例。但1例由于内膜片遮挡致髂动脉闭塞,1例由于肠道缺血死亡。 Ullery等[36]应用此方法治疗1例慢性夹层,撕开内膜后,使得夹层动脉瘤变成动脉瘤,再行标准的分体式支架植入。笔者应用cheese wire技术此方法处理5例,肾上1例,肾下4例。均取得良好效果。
5.2 凿
有些病例原内膜破口不能利用,需在内膜片上别的位置利用器具凿出新的破口(neofenestration)。从而可以把分支动脉的支架远端放置在分支动脉内,中间放置在假腔内,近端放置在真腔内,形成桥接通道。克服真狭小的困难,同时解决了分支动脉开口假腔的问题。凿的方法可以在导引导管的支撑下用导丝的硬头破膜,或TIPS(transjugular portosystemic shunt)针穿刺,然后再球囊扩张[21,37],或房间隔穿刺针[38],或用返回真腔装置[39]。笔者应用此方法处理1例肾动脉开口假腔,从而形成主支架窗口-新破口-假腔-肾动脉通路,再放置覆膜支架重建肾动脉。此时开窗支架需加强窗口的接触面积,如“袖口状”窗口、“分支型”窗口(branchedfenestration)等。
5.3 疏
利用假腔,真-假-真(true-false-true,TFT)腔方案,就是覆膜支架两端位于真腔内,而使支架主体部分位于假腔内,利用假腔空间。Kölbel等[40]首先把此方法应用到段胸主动脉,当真腔狭小或闭塞时,覆膜支架很难在其内展开,覆膜支架从腹腔干动脉的上方真腔进入大的假腔,然后在左锁骨下动脉远端破口进入弓部真腔,覆膜支架的通路就形成真腔 -假腔-真腔。Simring等[41]在胸腹主动脉段将1个分支支架放置在假腔内,近端放在真腔内,将各个分支桥接各腹部各分支动脉,远端接标准的分体式支架到髂动脉(真腔),实现了真-假-真腔血流灌注。笔者把此种方案应用到腹主动脉段,开窗分体式支架从髂动脉的真腔入路,进入假腔,再从肾下段的破口回到真腔,形成这一通路,分体式的支架近段开窗,开窗支架的开窗段在真腔内,然后从各窗口超选各内脏各分支动脉,实现各分支动脉重建。分体式支架一侧髂支在真腔内,一侧髂支在假腔内,远端接各髂支。在疏的方案内还包括将桥接的分支动 脉支架放在假腔内,这些支架可以正向,也 可以逆向(图1)。此种技术在腹主动脉夹层腔内修复中有以下优点:⑴借用假腔空间,利于腹主动脉支架分腿的释放,并增加手术的操作空间,提高手术成功率。⑵利于分支动脉开口于假腔的重建,可以结合烟囱技术、潜望镜技术、开窗技术和分支技术等。

图1 真腔-假腔-真腔方案 A:术前血管造影真腔受压,狭小,假腔较大,腹主动脉动脉段有较大破口(红色箭头所示);B:3D打印模具;C:改建开窗支架;D:腹腔干动脉假腔供血(红色箭头所示);E:改建开窗支架长髂支在假腔内(红色箭头所示),短髂支在破口上方的真腔内(蓝色箭头所示);F:肠系膜上动脉和双肾动脉开窗支架重建,腹腔干动脉在假腔内逆向分支支架重建;G:手术示意图Figure 1 True-false-true technique A: Preoperative angiography showing the compression and constriction of the true lumen,and enlargement of the false lumen, with a large tear in the segment of the abdominal aortic artery; B: 3D printing model;C: Reconstruction of the fenestrated stent-graft; D: Perfusion of the false lumen in the celiac trunk (shown by red arrow); E: The long iliac branch of the reconstructed fenestrated stent-graft in the false lumen (shown by red arrow), with its short branch in the true lumen(shown by blue arrow); F: Reconstruction of the superior mesenteric artery and bilateral renal arteries with the fenestrated stent-graft,and reconstruction of the celiac trunk by placement of a reverse branched stent-graft in the false lumen; G: Schematic picture of the operation
5.4 扩
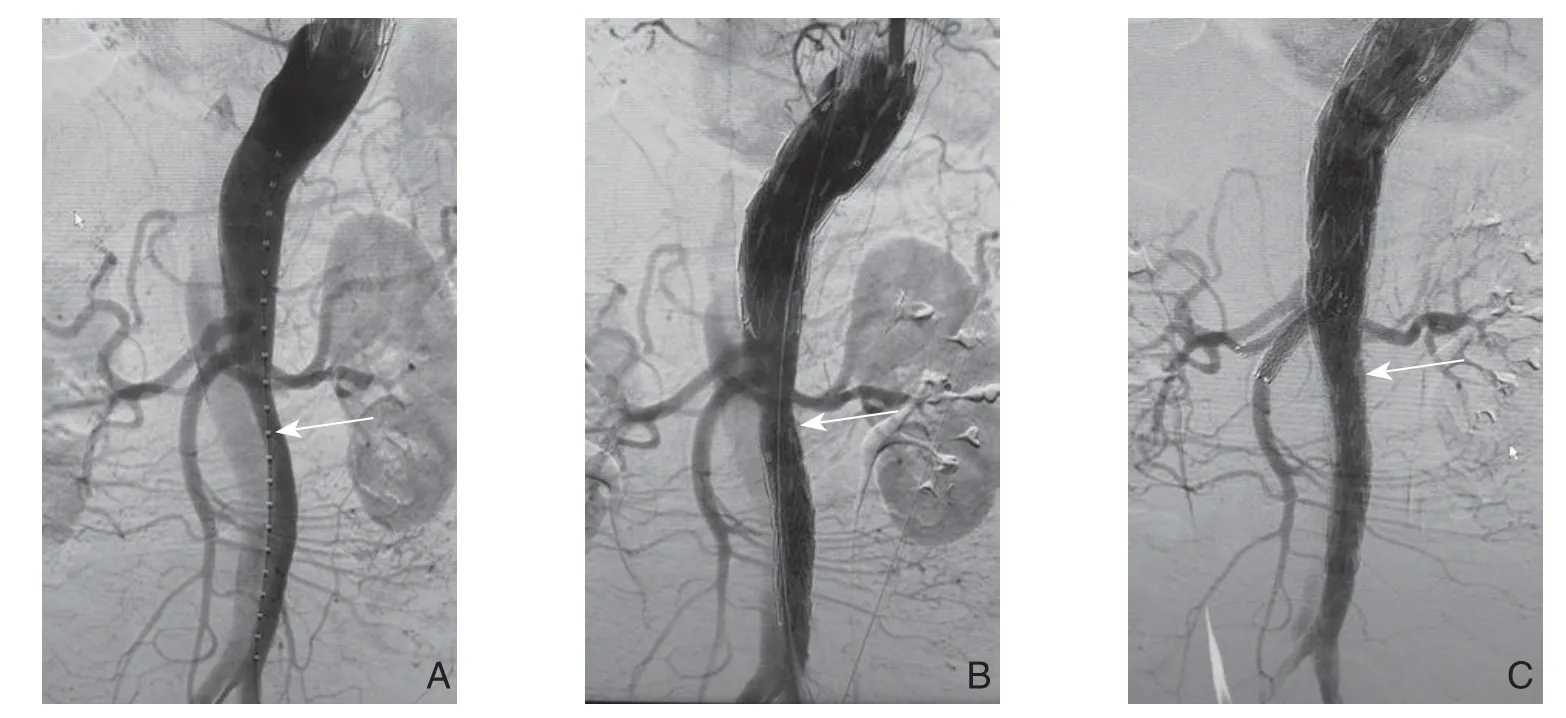
图2 三段式覆膜支架扩大真腔 A:术前血管造影真腔受压,狭小(箭头所示);B:在内脏动脉区两端放置覆膜支架后,内脏动脉区真腔扩大(箭头所示);C:内脏区分支动脉开窗支架分别重建(箭头所示)Figure 2 Expansion of the true lumen with three-segment stents A: Preoperative angiography showing the compression and constriction of the true lumen (shown by arrow); B: Enlargement of the true lumen in the visceral artery region after placement of covered stents at both sides of the visceral artery region (shown by arrow); C: Reconstruction of the visceral branches with fenestrated stent-grafts (shown by arrow)
分段式,是解决真腔狭小的方法之一,就是在腹腔干动脉以上和/或肾动脉以下主动脉放置直管式支架,使得内脏区主动脉的真腔相对扩大,以此为开窗支架获得相对大的空间,利于开窗支架多窗口精确对位。根据真腔节段的直径,可选择腹腔干动脉以上直管式支架结合开窗支架,或肾动脉以下主动脉直管式支架结合开窗支架的两段式,也可以腹腔干动脉以上和肾动脉以下主动脉直管式支架结合中间内脏区开窗支架的三段式。近端支架选择以大于模拟真腔2 mm为准[20]。Verhoeven等[42]应用两段式处理4例,笔者应用两段式处理4例,应用三段式处理4例,都取得良好的效果(图2)。这是一期处理,有些学者[32]主张主动脉先放置直管式支架,2个月后再开窗支架置入也是选择方案。这些方式的实施不仅扩大内脏分支动脉区真腔的扩大,而且使得我们对内脏分支动脉在“钟表盘”上的方向有更准确的预判。内脏分支动脉在受压真腔上的方向往往是不准确的,真腔预先张开后,这些内脏分支动脉的真实方向会更清楚。我们根据3D打印模具或CT工作站预估的开窗支架的窗口会更加准确。
以上几种方案可以结合使用,如可以用疏的方案开窗支架放置在假腔内,然后用凿的方案在内膜片上凿出新的破口,然后球囊扩张,从开窗支架的窗口桥接各分支动脉开口于真腔的血管[39,41]等。
6 并发症
截瘫和内漏是开窗支架应用主动脉夹层远端破口的两个主要严重并发症。其他如脏器的丢失、出血、支架的移位等并发症都需要进一步关注。
7 总 结
综上所述,开窗支架治疗慢性主动脉夹层远端破口总体效果是良好的,但由于解剖的复杂性和技术难度较高,仅能在一些大的中心开展,未能广泛开展。由于开展的时间较短,中长期效果如何,需更多循证医学的验证。
[1] Marui A, Mochizuki T, Koyama T, et al. Degree of fusiform dilatation of the proximal descending aorta in type B acute aortic dissection can predict late aortic events[J]. J Thorac Cardiovasc Surg, 2007, 134(5):1163–1170. doi: 10.1016/j.jtcvs.2007.07.037.
[2] Song JM, Kim SD, Kim JH, et al. Long-term predictors of descending aorta aneurysmal change in patients with aortic dissection[J]. J Am Coll Cardiol, 2007, 50(8):799–804. doi:10.1016/j.jacc.2007.03.064.
[3] Tsai TT, Evangelista A, Nienaber CA, et al. Long-term survival in patients presenting with type A acute aortic dissection: insights from the International Registry of Acute Aortic Dissection(IRAD)[J]. Circulation, 2006, 114(1 Suppl):I350–356. doi:10.1161/CIRCULATIONAHA.105.000497.
[4] Xu SD, Huang FJ, Yang JF, et al. Early and midterm results of thoracic endovascular aortic repair of chronic type B aortic dissection[J]. J Thorac Cardiovasc Surg, 2010, 139(6):1548–1553.doi: 10.1016/j.jtcvs.2009.08.051.
[5] Tsai TT, Evangelista A, Nienaber CA, et al. Partial thrombosis of the false lumen in patients with acute type B aortic dissection[J]. N Engl J Med, 2007, 357(4):349–359. doi: 10.1056/NEJMoa063232.
[6] Qin YL, Deng G, Li TX, et al. Risk factors of incomplete thrombosis in the false lumen after endovascular treatment of extensive acute type B aortic dissection[J]. J Vasc Surg, 2012,56(5):1232–1238. doi: 10.1016/j.jvs.2012.04.019.
[7] Sueyoshi E, Sakamoto I, Hayashi K, et al. Growth rate of aortic diameter in patients with type B aortic dissection during the chronic phase[J]. Circulation, 2004, 110(11 Suppl 1):II256–261. doi:10.1161/01.CIR.0000138386.48852.b6.
[8] Chen D, Müller-Eschner M, Kotelis D, et al. A longitudinal study of Type-B aortic dissection and endovascular repair scenarios:computational analyses[J]. Med Eng Phys, 2013, 35(9):1321–1330.doi: 10.1016/j.medengphy.2013.02.006.
[9] Tsai TT, Schlicht MS, Khanafer K, et al. Tear size and location impacts false lumen pressure in an ex vivo model of chronic type B aortic dissection[J]. J Vasc Surg, 2008, 47(4):844–851. doi: 10.1016/j.jvs.2007.11.059.
[10] Kim KM, Donayre CE, Reynolds TS, et al. Aortic remodeling,volumetric analysis, and clinical outcomes of endoluminal exclusion of acute complicated type B thoracic aortic dissections[J]. J Vasc Surg, 2011, 54(2):316–324. doi: 10.1016/j.jvs.2010.11.134.
[11] Kim U, Hong SJ, Kim J, et al. Intermediate to long-term outcomes of endoluminal stent-graft repair in patients with chronic type B aortic dissection[J]. J Endovasc Ther, 2009, 16(1):42–47. doi:10.1583/08–2563.1.
[12] Thrumurthy SG, Karthikesalingam A, Patterson BO, et al. A systematic review of mid-term outcomes of thoracic endovascular repair (TEVAR) of chronic type B aortic dissection[J]. Eur J Vasc Endovasc Surg, 2011, 42(5):632–647. doi: 10.1016/j.ejvs.2011.08.009.
[13] Idrees J, Roselli EE, Shafii S, et al. Outcomes after false lumen embolization with covered stent devices in chronic dissection[J]. J Vasc Surg, 2014, 60(6):1507–1513. doi: 10.1016/j.jvs.2014.08.094.
[14] Kim TH, Ko YG, Kwon SW, et al. Large false lumen area is a predictor of failed false lumen volume reduction after stentgraft repair in type B aortic dissection[J]. J Endovasc Ther, 2014,21(5):697–706. doi: 10.1583/14–4671MR.1.
[15] 中华医学会外科学分会血管外科学组. 主动脉夹层腔内治疗指南[J]. 中国实用外科杂志, 2008, 28(11):909–912.Vascular Surgery Group, Surgery Branch of Chinese Medical Association. Guidelines for endovascular treatment of aortic dissection[J]. Chinese Journal of Practical Surgery, 2008,28(11):909–912.
[16] Funaki B. Chronic complicated aortic dissection[J]. J Vasc Interv Radiol, 2013, 24(10):1460–1461. doi: 10.1016/j.jvir.2013.06.016.
[17] Patterson BO, Cobb RJ, Karthikesalingam A, et al. A systematic review of aortic remodeling after endovascular repair of type B aortic dissection: methods and outcomes[J]. Ann Thorac Surg, 2014,97(2):588–595. doi: 10.1016/j.athoracsur.2013.07.128.
[18] Sayer D, Bratby M, Brooks M, et al. Aortic morphology following endovascular repair of acute and chronic type B aortic dissection:implications for management[J]. Eur J Vasc Endovasc Surg, 2008,36(5):522–529. doi: 10.1016/j.ejvs.2008.06.023.
[19] 常光其, 王深明, 李晓曦, 等. 多撕裂口主动脉夹层的一期或分期血管腔内治疗[J]. 中华外科杂志, 2005, 43(13):866–869.doi:10.3760/j:issn:0529–5815.2005.13.010.Chang GQ, Wang SM, Li XX, et al. Single or staged endovascular stent-graft repair for aortic dissection with multi-tears[J].Chinese Journal of Surgery, 2005, 43(13):866–869. doi:10.3760/j:issn:0529–5815.2005.13.010.
[20] Sobocinski J, Spear R, Tyrrell MR, et al. Chronic dissection -indications for treatment with branched and fenestrated stentgrafts[J]. J Cardiovasc Surg (Torino), 2014, 55(4):505–517.
[21] Sobocinski J, Hertault A, Tyrrell M,et al. Chronic type B dissections: are fenestrated and branched endografts an option?[J]. J Cardiovasc Surg (Torino), 2013, 54(1 Suppl 1):97–107.
[22] Verhoeven EL, Muhs BE, Zeebregts CJ,et al. Fenestrated and branched stent-grafting after previous surgery provides a good alternative to open redo surgery[J]. Eur J Vasc Endovasc Surg,2007, 33(1):84–90. doi: 10.1016/j.ejvs.2006.06.016.
[23] Mirakhur A, Appoo JJ, Kent W, et al. Delayed intimal blowout after endovascular repair of aortic dissection[J]. J Vasc Interv Radiol,2013, 24(10):1471–1475. doi: 10.1016/j.jvir.2013.05.066.
[24] Mossop PJ, McLachlan CS, Amukotuwa SA, et al. Staged endovascular treatment for complicated type B aortic dissection[J].Nat Clin Pract Cardiovasc Med, 2005, 2(6):316–321. doi: 10.1038/ncpcardio0224.
[25] Melissano G, Bertoglio L, Rinaldi E, et al. Volume changes in aortic true and false lumen after the "PETTICOAT" procedure for type B aortic dissection[J]. J Vasc Surg, 2012, 55(3):641–651. doi:10.1016/j.jvs.2011.10.025.
[26] Kölbel T, Lohrenz C, Kieback A, et al. Distal false lumen occlusion in aortic dissection with a homemade extra-large vascular plug: the candy-plug technique[J]. J Endovasc Ther, 2013, 20(4):484–489.doi: 10.1583/13–4318.1.
[27] Bel A, Alsac JM, Baïssas V, et al. Spot stenting of the tear in type B aortic dissection[J]. Ann Vasc Surg, 2013, 27(5):671. doi: 10.1016/j.avsg.2012.06.019.
[28] Kim DJ, Lee KH, Lim SH, et al. Aorta Remodeling after Endovascular Treatment of a Chronic DeBakey IIIb Aneurysm and Simultaneous Palliation of a Renal Cell Carcinoma[J]. Korean J Thorac Cardiovasc Surg, 2015, 48(2):142–145. doi: 10.5090/kjtcs.2015.48.2.142.
[29] Evangelista A, Galuppo V, Gruosso D, et al. Role of entry tear size in type B aortic dissection[J]. Ann Cardiothorac Surg, 2014,3(4):403–405. doi: 10.3978/j.issn.2225–319X.2014.07.03.
[30] Anderson JL, Adam DJ, Berce M, et al. Repair of thoracoabdominal aortic aneurysms with fenestrated and branched endovascular stent grafts[J]. J Vasc Surg, 2005, 42(4):600–607. doi: 10.1016/j.jvs.2005.05.063.
[31] Oikonomou K, Katsargyris A, Ritter W, et al. Endovascular management of chronic post-dissection aneurysms[J]. Ann Cardiothorac Surg, 2014, 3(3):307–313. doi: 10.3978/j.issn.2225–319X.2014.04.02.
[32] Kitagawa A, Greenberg RK, Eagleton MJ,et al. Fenestrated and branched endovascular aortic repair for chronic type B aortic dissection with thoracoabdominal aneurysms[J]. J Vasc Surg, 2013,58(3):625–634. doi: 10.1016/j.jvs.2013.01.049.
[33] Spear R, Hertault A, Van Calster K,et al. Complex endovascular repair of postdissection arch and thoracoabdominal aneurysms[J]. J Vasc Surg, 2018, 67(3):685–693. doi: 10.1016/j.jvs.2017.09.010.
[34] Tam MD, Latham T, Brown JR, et al. Use of a 3D printed hollow aortic model to assist EVAR planning in a case with complex neck anatomy: potential of 3D printing to improve patient outcome[J]. J Endovasc Ther, 2014, 21(5):760–762. doi: 10.1583/14–4810L.1.
[35] Kos S, Gürke L, Jacob AL. A novel fenestration technique for abdominal aortic dissection membranes using a combination of a needle re-entry catheter and the "cheese-wire" technique[J].Cardiovasc Intervent Radiol, 2011, 34(6):1296–1302. doi: 10.1007/s00270–011–0110–5.
[36] Ullery BW, Chandra V, Dake M, et al. Cheese wire fenestration of a chronic juxtarenal dissection fl ap to facilitate proximal neck fi xation during EVAR[J]. Ann Vasc Surg, 2015, 29(1):124. doi: 10.1016/j.avsg.2014.07.025.
[37] Oikonomou K, Kopp R, Katsargyris A, et al. Outcomes of fenestrated/branched endografting in post-dissection thoracoabdominal aortic aneurysms[J]. Eur J Vasc Endovasc Surg,2014, 48(6):641–648. doi: 10.1016/j.ejvs.2014.07.005.
[38] Kölbel T, Diener H, Larena-Avellaneda A, et al. Advanced endovascular techniques for thoracic and abdominal aortic dissections[J]. J Cardiovasc Surg (Torino), 2013, 54(1 Suppl 1):81–90.
[39] Bertoglio L, Loschi D, Cambiaghi T, et al. Preliminary Outcomes of the LifeStream Balloon-Expandable Covered Stent in Fenestrated and Branched Thoracoabdominal Endovascular Repairs[J]. J Endovasc Ther, 2018, 25(2):230–236. doi:10.1177/1526602817752449.
[40] Kölbel T, Tsilimparis N, Wipper S, et al. TEVAR for chronic aortic dissection - is covering the primary entry tear enough?[J]. J Cardiovasc Surg (Torino), 2014, 55(4):519–527.
[41] Simring D, Raja J, Morgan-Rowe L, et al. Placement of a branched stent graft into the false lumen of a chronic type B aortic dissection[J]. J Vasc Surg, 2011, 54(6):1784–1787. doi: 10.1016/j.jvs.2011.05.053.
[42] Verhoeven EL, Tielliu IF, Ferreira M,et al. Thoraco-abdominal aortic aneurysm branched repair[J]. J Cardiovasc Surg (Torino),2010, 51(2):149–155.