脑白质疏松症对急性缺血性卒中患者影响的Meta分析
2018-05-15付敏郡赵亚亚蒋珍秀
付敏郡,胡 郎,赵亚亚,蒋珍秀,刘 宁
卒中是目前世界上第三大死亡原因,好发于中老年人,具有发病率高、病死率高、致残率高等特点。急性缺血性卒中(AIS)是卒中的主要类型,会危及患者的生命安全,影响患者的生活质量。脑白质疏松症(LA)又称脑白质高信号,是指分布于脑室周围、大脑皮质下白质及半卵圆中心的弥漫性病灶或散在病灶[1]。研究表明,LA是缺血性卒中、脑出血及痴呆的独立危险因素[2]。目前,LA对AIS患者影响的研究报道较多,但尚存在较大争议[3]。本研究采用Meta分析方法评估LA对AIS患者的影响,旨在为临床诊疗提供参考。
1 资料与方法
1.1 文献纳入与排除标准
1.1.1 文献纳入标准 (1)研究类型:病例对照研究。(2)研究对象:符合《各类脑血管疾病诊断要点》[4]中的AIS诊断标准,经颅脑CT或MRI检查确诊;发病时间≤1周;性别、年龄不限。(3)暴露因素:经颅脑CT或MRI检查证实存在LA,有明确的LA严重程度分级方法。(4)结局指标:改良Rankin量表(mRS)评分、Barthel指数(BI)评分、颅内出血转化发生率、症状性颅内出血[5]发生率、病死率、卒中复发率及血管再通率。
1.1.2 文献排除标准 (1)重复文献;(2)文献质量较差或存在数据雷同等无法利用的文献;(3)原始数据不完整的文献;(4)综述;(5)基础研究。
1.2 检 索 策 略 计 算 机 检 索 PubMed、EMBase、Web of Science(WOS)、The Cochrane Library、万方数据知识服务平台、中国生物医学文献数据库(CBM)和中国知网(CNKI)等,检索时间为建库至2017-11-30。中文检索词为“脑白质疏松症、脑白质高信号、脑白质损伤、脑小血管病、急性缺血性脑卒中、急性脑梗死”;英文检索词为“leukoaraiosis、white matter hyperintensities、cerebral small vascular diseases、white matter lesions、acute ischemic stroke”。
1.3 数据提取 由2位研究人员根据文献纳入与排除标准独立筛选文献、提取信息并进行方法学质量评价,如遇分歧则讨论解决或交由第三方裁定。依据PICO原则(P:研究对象;I:干预措施;C:对照;O:结局指标)设计信息提取表,提取内容包括文献的基本信息(第一作者、发表年份)、受试人群基本特征(例数、中位年龄)、干预措施、结局指标。
1.4 文献质量评价 采用纽卡斯尔-渥太华量表(NOS)[6]进行文献质量评价,从对象选择、可比性、结局和暴露3方面进行评价,满分9分,NOS评分5~9分为文献质量较高。
1.5 统计学方法 采用RevMan 5.3软件进行Meta分析,计数资料采用OR及其95%CI进行分析,计量资料采用MD及其95%CI进行分析。各文献间统计学异质性分析采用χ2检验,I2>50%且P<0.1表明各文献间有统计学异质性,采用随机效应模型进行Meta分析;I2≤50%且P≥0.1表明各文献间无统计学异质性,采用固定效应模型进行Meta分析。绘制倒漏斗图以分析发表偏倚。以P<0.05为差异有统计学意义。
2 结果
2.1 检索结果及纳入文献质量评价 共检索相关文献988篇,排除重复文献311篇,阅读文题及摘要后排除612篇文献,阅读全文后排除36篇文献,最终纳入29篇文献[7-35],其中英文文献28篇,中文文献1篇,包括15 883例患者,NOS评分均≥6分,文献质量较高,详见表1。文献筛选流程见图1。

表1 纳入文献的基本特征及质量评价Table 1 Basic characteristics and quality evaluation of the involved literatures
2.2 Meta分析结果
2.2.1 mRS 评 分 17 篇 文 献[9-10,13,17,19-23,25-26,28-33]报道了mRS评分,各文献间有统计学异质性(P<0.000 01,I2=81%),采用随机效应模型进行Meta分析;结果显示,有LA组患者mRS评分高于无LA组,差异有统计学意义〔MD=1.71,95%CI(1.29,2.27),P=0.000 2,见图 2〕。
2.2.2 BI评分 3 篇文献[12,30,33]报道了 BI评分,各文献间无统计学异质性(P=0.47,I2=0%),采用固定效应模型进行Meta分析;结果显示,有LA组患者BI评分低于无LA组,差异有统计学意义〔MD=2.51,95%CI(1.62,3.88),P<0.000 1,见图 3〕。
2.2.3 颅内出血转化发生率 5 篇文献[7,9,15,24,27]报道了颅内出血转化发生率,各文献间无统计学异质性(P=0.19,I2=34%),采用固定效应模型进行Meta分析;结果显示,有LA组患者颅内出血转化发生率高于无LA组,差异有统计学意义〔OR=1.34,95%CI(1.15,1.58),P=0.000 3,见图 4〕。
2.2.4 症状性颅内出血发生率 5 篇文献[16,18,29,34-35]报道了症状性颅内出血发生率,各文献间无统计学异质性(P=0.13,I2=43%),采用固定效应模型进行Meta分析;结果显示,有LA组患者症状性颅内出血发生率高于无LA组,差异有统计学意义〔OR=1.69,95%CI(1.31,2.19),P<0.000 1,见图 5〕。
2.2.5 病死率 4 篇文献[9,11,25,33]报道了病死率,各文献间有统计学异质性(P=0.004,I2=77%),采用随机效应模型进行Meta分析;结果显示,两组患者病死率比较,差异无统计学意义〔OR=1.11,95%CI(0.66,1.85),P=0.69,见图 6〕。
2.2.6 卒中复发率 2 篇文献[8,14]报道了卒中复发率,各文献间无统计学异质性(P=0.41,I2=0%),采用固定效应模型进行Meta分析;结果显示,有LA组患者卒中复发率高于无LA 组,差异有统计学意义〔OR=1.55,95%CI(1.26,1.91),P<0.000 1,见图 7〕。
2.2.7 血管再通率 2 篇文献[9,25]报道了血管再通率,各文献间无统计学异质性(P=0.39,I2=0%),采用固定效应模型进行Meta分析;两组患者血管再通率比较,差异无统计学意义〔OR=1.04,95%CI(0.74,1.45),P=0.83,见图 8〕。
2.3 发表偏倚 绘制倒漏斗图分析报道mRS评分文献的发表偏倚,结果显示,散点分布不对称,多数散点位于中下部,提示报道mRS评分文献的发表偏倚可能较大(见图9)。因报道其他结局指标的文献数量较少,倒漏斗图分析误差较大,故未绘制倒漏斗图。

图1 文献筛选流程Figure 1 Flow chart for literature screening
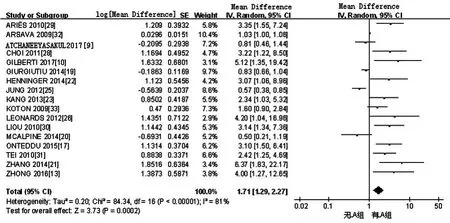
图2 无/有LA组患者mRS评分比较的森林图Figure 2 Forest plot for comparison of mRS score in patients with leukoaraiosis or not
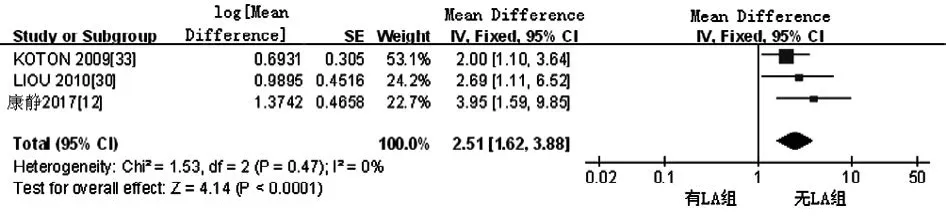
图3 无/有LA组患者BI评分比较的森林图Figure 3 Forest plot for comparison of BI score between without LA group and LA group

图4 无/有LA组患者颅内出血转化发生率比较的森林图Figure 4 Forest plot for comparison of incidence of intracranial hemorrhagic transformation in patients with leukoaraiosis or not

图5 无/有LA组患者症状性颅内出血发生率比较的森林图Figure 5 Forest plot for comparison of incidence of symptomatic intracerebral hemorrhage in patients with leukoaraiosis or not
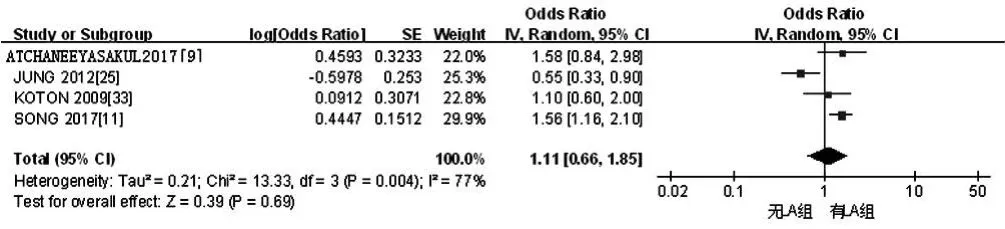
图6 无/有LA组患者病死率比较的森林图Figure 6 Forest plot for comparison of fatality rate in patients with leukoaraiosis or not

图7 无/有LA组患者卒中复发率比较的森林图Figure 7 Forest plot for comparison of recurrent rate of stroke in patients with leukoaraiosis or not
3 讨论
LA是由Hachinski在1987年首次提出的一个影像学诊断术语,用来描述脑皮质下白质CT密度灶,多见于老年人[36]。LA在T2加权像与液体衰减反转恢复(FLAIR)序列表现为白质高信号,病变部位小血管管壁出现增厚、透明样变,导致血管曲折、狭窄,造成管腔内血流量减少,不利于卒中患者侧支循环的建立[2]。LIN等[37]研究结果显示,非痴呆人群LA发生率约为73.0%,40~80岁住院患者LA发生率约为58.3%,>80岁住院患者LA发生率约为82.7%。研究表明,LA与痴呆、残疾、卒中等关系密切[38]。多项研究表明,LA是脑小血管相关性疾病,主要病理表现为不同程度的髓鞘和轴突脱失、小动脉硬化和轻微的神经胶质细胞增生等[39-40]。
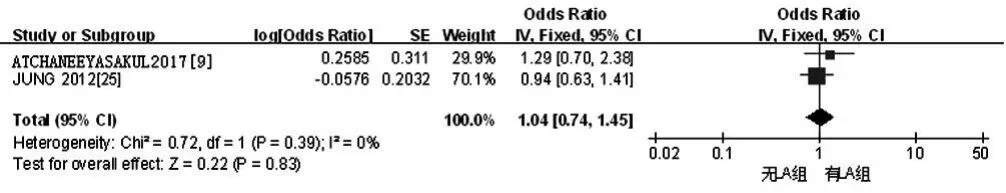
图8 无/有LA组患者血管再通率比较的森林图Figure 8 Forest plot for comparison of vascular recanalization rate in patients with leukoaraiosis or not

图9 报道mRS评分文献发表偏倚的倒漏斗图Figure 9 Inverted funnel plot for publication bias of involved literatures reported mRS score
AIS合并LA患者上皮细胞、星形胶质细胞损伤及氧化应激反应会破坏血管内皮细胞完整性,使血-脑脊液屏障通透性增加,同时LA区域脑微循环长期损伤会诱发缺血组织出血转化[41-42]。研究表明,卒中后梗死灶面积扩大会影响患者预后,而LA是梗死灶面积扩大的独立危险因素[3]。RYU等[43]通过对5 000例卒中患者进行研究发现,卒中合并LA患者神经功能损伤较重,且治疗3个月后患者神经功能改善效果较差。SENDA等[44]研究表明,AIS合并LA患者神经功能损伤较重、认知功能较差,会严重影响患者的生活质量。多项研究表明,有LA的卒中患者溶栓治疗后出血转化发生率高于无LA的卒中患者[45-47]。KUMRAL等[48]研究表明,AIS合并LA患者卒中复发率高于未合并LA者。
本Meta分析结果显示,有LA组患者mRS评分高于无LA组,提示AIS合并LA患者神经功能损伤较重;有LA组患者BI评分低于无LA组,提示AIS合并LA患者日常生活活动能力较差;有LA组患者颅内出血转化发生率、症状性颅内出血发生率、卒中复发率高于无LA组,与既往研究结果一致[8],提示AIS合并LA患者颅内出血转化发生率、症状性颅内出血发生率、卒中复发率较高;两组患者病死率、血管再通率间无差异,与既往研究结果一致[49]。
本Meta分析的局限性:(1)纳入文献均为病例对照研究,且多为单中心研究,可能降低结果的可信性;(2)纳入文献均为已发表文献,未检索相关会议论文等,可能对研究结果产生一定影响。
参考文献
[1]WARDLAW J M,SMITH C,DICHGANS M.Mechanisms of sporadic cerebral small vessel disease: insights from neuroimaging[J].Lancet Neurol,2013,12(5):483-497.DOI:10.1016/S1474-4422(13)70060-7.
[2]ETHERTON M R,WU O,ROST N S.Recent Advances in Leukoaraiosis: White Matter Structural Integrity and Functional Outcomes after Acute Ischemic Stroke[J].Curr Cardiol Rep,2016,18(12):123.DOI:10.1007/s11886-016-0803-0.
[3]FIERINI F,POGGESI A,PANTONI L.Leukoaraiosis as an outcome predictor in the acute and subacute phases of stroke[J].Expert Rev Neurother,2017,17(10):963-975.DOI:10.1080/14737175.2017.1371013.
[4]各类脑血管疾病诊断要点[J].中华神经科杂志,1996,29(6):60-61.
[5]LARRUE V,VON KUMMER R R,MÜLLER A,et al.Risk factors for severe hemorrhagic transformation in ischemic stroke patients treated with recombinant tissue plasminogen activator: a secondary analysis of the European-Australasian Acute Stroke Study (ECASS II)[J].Stroke,2001,32(2):438-441.
[6]WELLS G A,SHEA B,O'CONNELL D,et al.The Newcastle-Ottawa Scale (NOS) for Assessing the Quality of Non-Randomized Studies in Meta-Analysis[J].The Ottawa Hospital Research Institute,2013,3:1-4.
[7]WEI C C,ZHANG S T,WANG Y H,et al.Association between leukoaraiosis and hemorrhagic transformation after cardioembolic stroke due to atrial fibrillation and/or rheumatic heart disease[J].J Neurol Sci,2017,378:94-99.DOI:10.1016/j.jns.2017.05.001.
[8]NAM K W,KWON H M,LIM J S,et al.Clinical relevance of abnormal neuroimaging findings and long-term risk of stroke recurrence[J].Eur J Neurol,2017,24(11):1348-1354.DOI:10.1111/ene.13391.
[9]ATCHANEEYASAKUL K,LESLIE-MAZWI T,DONAHUE K,et al.White Matter Hyperintensity Volume and Outcome of Mechanical Thrombectomy With Stentriever in Acute Ischemic Stroke[J].Stroke,2017,48(10):2892-2894.DOI:10.1161/STROKEAHA.117.018653.
[10]GILBERTI N,GAMBA M,PREMI E,et al.Leukoaraiosis is a predictor of futile recanalization in acute ischemic stroke[J].J Neurol,2017,264(3):448-452.DOI:10.1007/s00415-016-8366-y.
[11]SONG T J,KIM J,SONG D,et al.Total Cerebral Small-Vessel Disease Score is Associated with Mortality during Follow-Up after Acute Ischemic Stroke[J].J Clin Neurol,2017,13(2):187-195.DOI:10.3988/jcn.2017.13.2.187.
[12]康静,李晨曦,范百亚,等.急性脑梗死患者脑白质疏松程度与静脉溶栓治疗后日常生活能力恢复的关系[J].血栓与止血学,2017,23(4):591-594,598.
[13]ZHONG G,YAN S,ZHANG S,et al.Association between Leukoaraiosis and Poor Outcome is not due to Reperfusion Inefficiency after Intravenous Thrombolysis[J].Transl Stroke Res,2016,7(5):439-445.DOI:10.1007/s12975-016-0473-7.
[14]MOERCH-RASMUSSEN A,NACU A,WAJE-ANDREASSEN U,et al.Recurrent ischemic stroke is associated with the burden of risk factors[J].Acta Neurol Scand,2016,133(4):289-294.DOI:10.1111/ane.12457.
[15]NIGHOGHOSSIAN N,ABBAS F,CHO T H,et al.Impact of leukoaraiosis on parenchymal hemorrhage in elderly patients treated with thrombolysis[J].Neuroradiology,2016,58(10):961-967.DOI:10.1007/s00234-016-1725-7.
[16]CURTZE S,HAAPANIEMI E,MELKAS S,et al.White Matter Lesions Double the Risk of Post-Thrombolytic Intracerebral Hemorrhage[J].Stroke,2015,46(8):2149-2155.DOI:10.1161/STROKEAHA.115.009318.
[17]ONTEDDU S R,GODDEAU R P Jr,MINAEIAN A,et al.Clinical impact of leukoaraiosis burden and chronological age on neurological deficit recovery and 90-day outcome after minor ischemic stroke[J].J Neurol Sci,2015,359(1/2):418-423.DOI:10.1016/j.jns.2015.10.005.
[18]IST-3 collaborative group.Association between brain imaging signs,early and late outcomes,and response to intravenous alteplase after acute ischaemic stroke in the third International Stroke Trial (IST-3): secondary analysis of a randomised controlled trial[J].Lancet Neurol,2015,14(5):485-496.DOI:10.1016/S1474-4422(15)00012-5.
[19]GIURGIUTIU D V,YOO A J,FITZPATRICK K,et al.Severity of leukoaraiosis,leptomeningeal collaterals,and clinical outcomes after intra-arterial therapy in patients with acute ischemic stroke[J].J Neurointerv Surg,2015,7(5):326-330.DOI:10.1136/neurintsurg-2013-011083.
[20]MCALPINE H,CHURILOV L,MITCHELL P,et al.Leukoaraiosis and early neurological recovery after intravenous thrombolysis[J].J Stroke Cerebrovasc Dis,2014,23(9):2431-2436.DOI:10.1016/j.jstrokecerebrovasdis.2014.05.012.
[21]ZHANG J,PURI A S,KHAN M A,et al.Leukoaraiosis predicts a poor 90-day outcome after endovascular stroke therapy[J].AJNR Am J Neuroradiol,2014,35(11):2070-2075.DOI:10.3174/ajnr.A4029.
[22]HENNINGER N,KHAN M A,ZHANG J,et al.Leukoaraiosis predicts cortical infarct volume after distal middle cerebral artery occlusion[J].Stroke,2014,45(3):689-695.DOI:10.1161/STROKEAHA.113.002855.
[23]KANG H J,STEWART R,PARK M S,et al.White matter hyperintensities and functional outcomes at 2 weeks and 1 year after stroke[J].Cerebrovasc Dis,2013,35(2):138-145.DOI:10.1159/000346604.
[24]KUFNER A,GALINOVIC I,BRUNECKER P,et al.Early infarct FLAIR hyperintensity is associated with increased hemorrhagic transformation after thrombolysis[J].Eur J Neurol,2013,20(2):281-285.DOI:10.1111/j.1468-1331.2012.03841.x.
[25]JUNG S,MONO M L,FINDLING O,et al.White matter lesions and intra-arterial thrombolysis[J].J Neurol,2012,259(7):1331-1336.DOI:10.1007/s00415-011-6352-y.
[26]LEONARDS C O,IPSEN N,MALZAHN U,et al.White matter lesion severity in mild acute ischemic stroke patients and functional outcome after 1 year[J].Stroke,2012,43(11):3046-3051.DOI:10.1161/STROKEAHA.111.646554.
[27]SHI Z S,LOH Y,LIEBESKIND D S,et al.Leukoaraiosis predicts parenchymal hematoma after mechanical thrombectomy in acute ischemic stroke[J].Stroke,2012,43(7):1806-1811.DOI:10.1161/STROKEAHA.111.649152.
[28]CHOI J H,BAE H J,CHA J K.Leukoaraiosis on magnetic resonance imaging is related to long-term poor functional outcome after thrombolysis in acute ischemic stroke[J].J Korean Neurosurg Soc,2011,50(2):75-80.DOI:10.3340/jkns.2011.50.2.75.
[29]ARIËS M J,UYTTENBOOGAART M,VROOMEN P C,et al.tPA treatment for acute ischaemic stroke in patients with leukoaraiosis[J].Eur J Neurol,2010,17(6):866-870.DOI:10.1111/j.1468-1331.2010.02963.x.
[30]LIOU L M,CHEN C F,GUO Y C,et al.Cerebral white matter hyperintensities predict functional stroke outcome[J].Cerebrovasc Dis,2010,29(1):22-27.DOI:10.1159/000255970.
[31]TEI H,UCHIYAMA S,USUI T,et al.Posterior circulation ASPECTS on diffusion-weighted MRI can be a powerful marker for predicting functional outcome[J].J Neurol,2010,257(5):767-773.DOI:10.1007/s00415-009-5406-x.
[32]ARSAVA E M,RAHMAN R,ROSAND J,et al.Severity of leukoaraiosis correlates with clinical outcome after ischemic stroke[J].Neurology,2009,72(16):1403-1410.DOI:10.1212/WNL.0b013e3181a18823.
[33]KOTON S,SCHWAMMENTHAL Y,MERZELIAK O,et al.Cerebral leukoaraiosis in patients with stroke or TIA: clinical correlates and 1-year outcome[J].Eur J Neurol,2009,16(2):218-225.DOI:10.1111/j.1468-1331.2008.02389.x.
[34]PALUMBO V,BOULANGER J M,HILL M D,et al.Leukoaraiosis and intracerebral hemorrhage after thrombolysis in acute stroke[J].Neurology,2007,68(13):1020-1024.DOI:10.1212/01.wnl.0000257817.29883.48.
[35]NEUMANN-HAEFELIN T,HOELIG S,BERKEFELD J,et al.Leukoaraiosis is a risk factor for symptomatic intracerebral hemorrhage after thrombolysis for acute stroke[J].Stroke,2006,37(10):2463-2466.DOI:10.1161/01.STR.0000239321.53203.ea.
[36]HACHINSKI V C,POTTER P,MERSKEY H.Leuko-araiosis[J].Arch Neurol,1987,44(1):21-23.
[37]LIN Q,HUANG W Q,MA Q L,et al.Incidence and risk factors of leukoaraiosis from 4683 hospitalized patients: A cross-sectional study[J].Medicine (Baltimore),2017,96(39):e7682.DOI:10.1097/MD.0000000000007682.
[38]SIBOLT G,CURTZE S,MELKAS S,et al.White matter lesions are associated with hospital admissions because of hip-fractures and trauma after ischemic stroke[J].Stroke,2014,45(10):2948-2951.DOI:10.1161/STROKEAHA.114.006116.
[39]PANTONI L.Cerebral small vessel disease: from pathogenesis and clinical characteristics to therapeutic challenges[J].Lancet Neurol,2010,9(7):689-701.DOI:10.1016/S1474-4422(10)70104-6.
[40]PRINS N D,SCHELTENS P.White matter hyperintensities,cognitive impairment and dementia: an update[J].Nat Rev Neurol,2015,11(3):157-165.DOI:10.1038/nrneurol.2015.10.
[41]DE SILVA T M,MILLER A A.Cerebral Small Vessel Disease:Targeting Oxidative Stress as a Novel Therapeutic Strategy?[J].Front Pharmacol,2016,7:61.DOI:10.3389/fphar.2016.00061.eCollection 2016.
[42]LLOMBART V,DOMINGUEZ C,BUSTAMANTE A,et al.Fluorescent molecular peroxidation products: a prognostic biomarker of early neurologic deterioration after thrombolysis[J].Stroke,2014,45(2):432-437.DOI:10.1161/STROKEAHA.113.003431.
[43]RYU W S,WOO S H,SCHELLINGERHOUT D,et al.Stroke outcomes are worse with larger leukoaraiosis volumes[J].Brain,2017,140(1):158-170.DOI:10.1093/brain/aww259.
[44]SENDA J,ITO K,KOTAKE T,et al.Association of Leukoaraiosis With Convalescent Rehabilitation Outcome in Patients With Ischemic Stroke[J].Stroke,2016,47(1):160-166.DOI:10.1161/STROKEAHA.115.010682.
[45]LIN Q,LI Z,WEI R,et al.Increased Risk of Post-Thrombolysis Intracranial Hemorrhage in Acute Ischemic Stroke Patients with Leukoaraiosis: A Meta-Analysis[J].PLoS One,2016,11(4):e0153486.DOI:10.1371/journal.pone.0153486.
[46]CHARIDIMOU A,PASI M,FIORELLI M,et al.Leukoaraiosis,Cerebral Hemorrhage,and Outcome After Intravenous Thrombolysis for Acute Ischemic Stroke: A Meta-Analysis (v1)[J].Stroke,2016,47(9):2364-2372.DOI:10.1161/STROKEAHA.116.014096.
[47]KONGBUNKIAT K,WILSON D,KASEMSAP N,et al.Leukoaraiosis,intracerebral hemorrhage,and functional outcome after acute stroke thrombolysis[J].Neurology,2017,88(7):638-645.DOI:10.1212/WNL.0000000000003605.
[48]KUMRAL E,GÜLLÜO L U H,ALAKBAROVA N,et al.Association of leukoaraiosis with stroke recurrence within 5 years after initial stroke[J].J Stroke Cerebrovasc Dis,2015,24(3):573-582.DOI:10.1016/j.jstrokecerebrovasdis.2014.10.002.
[49]INZITARI D,PRACUCCI G,POGGESI A,et al.Changes in white matter as determinant of global functional decline in older independent outpatients: three year follow-up of LADIS(leukoaraiosis and disability) study cohort[J].BMJ,2009,339:b2477.DOI:10.1136/bmj.b2477.
