Toxoplasma gondii and human immunodeficiency virus co-infection in western Iran: A cross sectional study
2018-05-09NaserNazariArezooBozorgomidAlirezaJanbakhshFarshidBashiri
Naser Nazari, Arezoo Bozorgomid, Alireza Janbakhsh, Farshid Bashiri
1Department of Medical Parasitology and Mycology, Faculty of Medicine, Kermanshah University of Medical Sciences, Shahid Shiroudi blvrd. ,Daneshgah St. Kermanshah, Iran
2Department of Microbiolgy, Asadabad School of Medical Sciences, Asadabad, Iran
3Department of Infection Disease, Faculty of Medicine, Kermanshah University of Medical Sciences, Shahid Shiroudi blvrd. , Daneshgah St.Kermanshah, Iran
1. Introduction
Toxoplasma gondii(T. gondii) as a ubiquitous parasite is one of the most common zoonotic parasitic diseases in almost all warmblooded vertebrates across the world. It is estimated that 1/3 of the human population in the world has been infected by this protozoan parasite[1]. The primary infection withT. gondiican be asymptomatic and self-limiting in immunocompetent individuals[1].However, in pregnant women, immunocompromised patients such as those with acquired immune deficiency syndrome (AIDS) and patients receiving chemotherapy or immunosuppressive drugs,an infection withT. gondiimay be reactivated in various organs especially brain[2].
Cerebral toxoplasmosis is an important health-related complication in patients with AIDS, which is often observed in the advanced stages of the disease and can lead to morbidity and mortality. In the absence of prophylaxis strategies, 30%-40% of HIV-infected patients will develop toxoplasmic encephalitis (TE)[3]. Suitable prophylaxis can effectively reduce the rate of TE. Therefore, a timely diagnosis and treatment ofT. gondiiserious affect the clinical management of patients with HIV. Additionally, with advent of highly active antiretroviral therapy (HAART) and its effect in improving the immunological status of patients with AIDS have reduced the incidence of TE and death associated with it.
In Iran, the first case of the HIV infection was detected in 1986. By 2014, 27 888 Iranians were reported to be infected with HIV among which 12.63% (3 300 individuals) lived in the Kermanshah Province in the west of Iran[4]. Despite our knowledge on the epidemiology of the HIV infection in Iran, little information is available about opportunistic infections in the population of HIV patients. A recent systematic review study of toxoplasmosis in Iranian immunocompromised patients including HIV/AIDS, cancer, and transplantation showed that the rate of seroprevalence was 50.01%[5].Due to a lack of information on the toxoplasmosis serologic status among patients with HIV in Kermanshah, Iran, the risk for damage to the brain and the high morbidity rate of these patients, this study aimed to evaluate the seroepidemiology ofT. gondiiinfection in patients with HIV. Moreover, improving our knowledge about the seroepidemiology of toxoplasmosis among patients with HIV/AIDS can help us design effective strategies for controlling and preventing this disease.
2. Methodology
2.1. Sample collection and epidemiological factors
This cross sectional study was carried out with 385 patients with HIV/AIDS referred to the behavior disease consultation center(BDCC) in Kermanshah in the West of Iran from May 2012 to June 2013. The study participants were diagnosed with HIV and were undergoing the follow up process by the healthcare professionals in the BDCC. The demographic and epidemiologic characteristic of the patients were collected through interviews. In addition, the patients were evaluated with regard to the presence of co-infections, receiving anti-Toxoplasmaprophylaxis and antiretroviral therapy (ART). The CD4+ T-lymphocyte counts for each patient were measured by the flow cytometry procedure and documented in the patient health file.A sample consisting of 5 mL of venous blood was collected from each person. After the separation of serum, it was labeled and stored at 20 °C until the time of use.
2.2. ELISA
The sample was tested for anti-ToxoplasmaIgG and IgM antibodies by using the ELISA technique according to the manufacturers’instructions (ToxoplasmaIgG and IGM kit, PISHTAZ TEB®, Tehran,Iran). The optical density of IgG and IgM antibody titers were read at 450 nm. The sample containing above 11 IU/mL was considered positive. The patient was diagnosed negative when the titer the serum IgG and IgM antibodies were lower than 9 IU/mL. Those patients with the range of antibody titers between 9 and 11 IU/mL were considered doubtful positive.
2.3. Ethical clearance
This study was approved by the Research Ethics Committee affiliated with the Kermanshah University of Medical Sciences,Kermanshah, Iran. All the patients were requested to sign the written informed consent form.
2.4. Statistical analysis
Descriptive and inferential statistics via the SPSS software v.16 was used for data analysis. The Chi-squared and Fisher’s exact tests were used to report the associations between variables.P<0.05 was considered statistically significant.
3. Results
In this study, 385 patients consisting of 281 males and 104 females participated. The age range of the patients was 3-68 years and the mean age of the male and female patients was 37.9 years and 34.0 years, respectively. Also, 40.8% (157/358) and 2.6% (10/358)patients were positive for anti-T. gondiiIgG and IgM antibodies,respectively. The prevalence of IgG and IgM antibodies was higher in the age group of 46-60 years, which was statistically significant(P=0.01 andP= 0.01, respectively).
No statistically significant association was reported between the seroprevalence ofToxoplasmainfection (seropositivity to IgM or IgG antibodies) and gender, the level of education, occupation, residence,marital status, prophylaxis status and use of azithromycin (P>0.05)(Table 1).
The majority of the patients had the history of infection with hepatitis C (n=190), hepatitis B (n=17), tuberculosis (n=69) and candidiasis (n=42). About 41.1% (78/190) patients with hepatitis C hadToxoplasmaseropositivity for the anti-ToxoplasmaIgG antibody and 4 patients with hepatitis C had seropositivity for the anti-ToxoplasmaIgM antibody. However, no statistically significance association was reported between seropositivity and the abovementioned infections (P>0.05).

Table 1The sociodemographic characteristics of HIV-infected patients in this study.
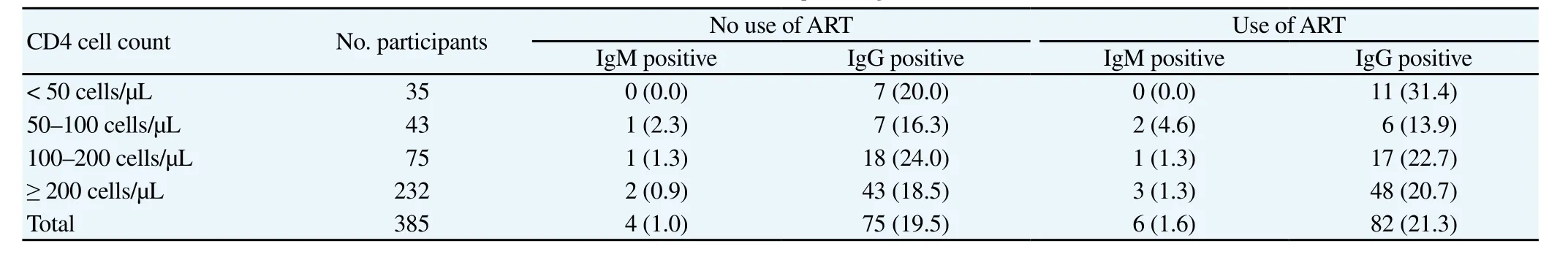
Table 2The frequency of 385 HIV-positive patients seropositive and seronegative for Toxoplasma gondii related to the levels of CD4+ and use of ART[n(%)].
The mean CD4+ lymphocyte count of the patients with HIV was 327 cells/μL. About 35.8% (28/78) of the patients with HIV who had CD4+ count below 100 cells/μL were seropositive to theToxoplasmaIgG antibody. Regarding chemoprophylaxis in HIV, 14 and 7Toxoplasma-seropositive patients with a CD4+ cell count <100 cells/mm3were not receiving ART and prophylaxis, respectively.No statistically significance association was observed between the patient seropositivity and CD4+ T cell count (P>0.05). The frequency of seropositivity and antiretroviral use related to the levels of CD4+ T- lymphocytes are shown in Table 2.
4. Discussion
Opportunistic infections (OIs) are one of the identified causes for enhancing immunodeficiency in patients with HIV. Also,T. gondiias one of the OIs causes cerebral toxoplasmosis that can be a major threat to the health of patients with HIV. Antiretroviral drugs and HAART have suppressed HIV viral replication and increased CD4+T-cell counts. Therefore, the incidence of OIs in these patients has reduced[6].
This study aimed to investigate the toxoplasmosis serology in patients with HIV referred to the BDCC in Kermanshah, Iran. In total, 40.8% of the patients were seropositive for the anti-T. gondiiIgG antibody. This seroprevalence did not vary greatly from previous study performed among the general population in the same region(36.3%)[7]. The results of this study revealed that the HIV infection did not increase the risk for toxoplasmosis. A probable reason is that the patients mainly acquired this infection during childhood and adolescence and before the HIV infection. A meta-analysis study among patients with HIV/AIDS in Iran showed that the risk for toxoplasmosis was 50.05%[5]. The lower risk in our study can be attributed to differences in lifestyles, geographic area and weather conditions. Kermanshah province has a moderate and mountainous climate. It is rainy mostly in winters and is moderately warm in summers. Therefore, climate effects influence the survival of oocysts in this environment. However, this infection is widespread in the humid and warm weathers than in other weathers. Furthermore, the consumption of undercooked or raw meat is a risk factor for the infection with toxoplasmosis. A study reported that 18.2% of the sheep cattle and goats in Kermanshah province had the serological evidence for theT. gondiiinfection[8]. Therefore, patients with HIV are at the risk for acquiring the toxoplasmosis infection in this area.In this study, the prevalence of the anti-T. gondiiIgM antibody was 2.6% (10/385) including eight men and two women. Nevertheless,no statistically significant difference was observed (P>0.05).Regarding previous studies, a study from Ethiopia showed that anti-T. gondiiIgM antibodies seroprevalence in HIV seropositive individuals, was 10.7%[9]. However, Rahimiet al. reported that no person had the IgM anti-T. gondiiantibodies in Mazandaran Province, North of Iran[10]. Shenet al. found three patients (1.2%)with the anti-ToxoplasmaIgM antibody[11].
Among all patients with HIV, 112 men (112/281, 39.9%) and 45 women (45/104, 43.3%) were positive for the anti-T. gondiiIgG antibody. Although few studies have reported vertical transmission ofT. gondiithrough reactivation of toxoplasmosis, it is relatively rare[12,13]. No statistically significant difference was detected in the seroprevalence of the anti-ToxoplasmaIgG antibody between males and females (P>0.05).
The overall seroprevalence was highest in the 46-60 year age group (51.8%, 28/53) in his study. The study of Zhanget al. has shown the highest prevalence of disease in 3rd and 4th decades of life[14]. Nonetheless, Walleet al. reported the highest prevalence rate in 21-30 year age group[9]. This can probably be explained by the prolonged exposure time with the increase of patient age.
Many studies showed that more Iranian patients with HIV were illicit drug abusers[15,16]. The illicit drug users are at the high risk for the toxoplasmosis infection, particularly due to inferior socioeconomical, occupational and nutritional situations[17,18]. In this study, approximately 1/3 of the patients were unemployed. However,no statistically significant difference was observed between occupation, the educational level, marital status and residence areas and seroreactivity to the anti-T. gondiiantibodies.
Azithromycin is used for the treatment or as the prophylaxis forMycobacterium avium, subspecies paratuberculosis, but it can also provokes Crohn's disease. Since azithromycin can be an alternative treatment for the toxoplasmosis[19], its correlation with seroepidemiology of the infection was assessed. However, no statistically significant difference was reported between theT. gondiiseropositivity and azithromycin.
The mean CD4+ lymphocyte count of the patients with HIV was 327 cells/μL while theT. gondiiseropositive had the mean CD4+lymphocyte count of 346 cells/μL. A total of 20.2% (78/385) of the study participants had CD4+ T lymphocyte count less than 100 cells/μL. It could be concluded that the patients with HIV in the Kermanshah region should be considered at the high risk for developing the toxoplasmosis disease, especially when CD4+ T-cells count was below 100 cells/μL.
The ART and cotrimoxazole prophylaxis were not used by 47.3%(182/385) and 55.6% (214/385) of the patients in this study,respectively. Also, HIV-infected patients who did not receive ART and cotrimoxazole prophylaxis had 40% (72/182) and 39% (84/214)anti-ToxoplasmaIgG antibodies, respectively, indicating a high risk of the reactivation of dormant cysts. It is noteworthy that 30%-40%of toxoplasmosis patients with AIDS finally developed TE[3]. One HIV-infected patient (3.3%) in this study had the history of TE and two patients had the history of clinical toxoplasmosis. All of them were seropositive to theToxoplasmainfection.
A systematic review and meta-analysis study reported the incidence of OIs and the impact of antiretroviral therapy among 491 608 patients with HIV between 1990 and 2013. Overall,a major reduction in the risk of infection during the first year of treatment using the ART and with the largest effect on oral candidiasis,Pneumocystispneumonia and toxoplasmosis (range from 57%-91%) [20]. Based on our findings, no statistically significant differences between theT. gondiiseropositivity with the antiretroviral treatment and cotrimoxazole prophylaxis were reported.
There was no remarkable difference between theT. gondiiseropositivity with the CD4+ lymphocyte count, which is consistent with the reports of studies from Ethiopia and Morocco[21,22]. Another study in Jahrom, Iran found a correlation between the CD4+ count,100 cells/μL and theToxoplasmaseropositivity[23]. Although CD4+T cells play a major role in protection against intracellular protozoan parasites such asT. gondiias the producers of IFN- γ, CD8+ T cell and NK cell also are important effector cells in the control of parasite reactivation during HIV infection[24].
As a limitation of this study, the patients were referred to one BDCC that could not reflect the real prevalence of toxoplasmosis among patients with HIV. Therefore, the investigation of associations between the risk factors needs the inclusion of more healthy and infected patients in future studies. Also, approximately 70% of the patients were male and did not allow a perfect gender-specific data analysis. Additionally, monitoring of the antiretroviral treatment and adherence to it and the possibility of adverse reactions were not studied. A study of patients with HIV/AIDS in Brazil showed that the antiretroviral treatment was not used regularly by 32% of patients[25].
The results of this study highlighted the high risk for clinical toxoplasmosis in individuals with HIV, because of the possibility of reactivation of the infection in the seropositive patients who do not adhere to the ART and infection in seronegative patients without primary prophylaxis. TE should be suspected in all people with advanced HIV infection. Undiagnosed patients with HIV may present their initial symptoms of their disease with TE.
Further studies are needed to determine the prevalence of TE in patients with HIV. Moreover, there is a need to investigateT. gondiistrains in patients for evaluating the population genetic structure ofT. gondiiand the association between the parasite genotype and the disease patterns in patients with HIV.
Conflict of interest statement
We have no conflict of interest related to this work.
Acknowledgment
The authors would like to thank the Behavior Disease Consultation Center (BDCC) in Kermanshah, Iran for their kind assistance during this research project.
[1] Halonen SK, Weiss LM. Toxoplasmosis.Handb Clin Neurol2013; 114:125-145.
[2] Montoya J, Liesenfeld O. Toxoplasmosis.Lancet2004; 363: 1965-1976.
[3] Luma HN, Tchaleu BC, Mapoure YN, Temfack E, Doualla MS, Halle MP, et al.Toxoplasmaencephalitis in HIV/AIDS patients admitted to the Douala general hospital between 2004 and 2009: A cross sectional study.BMC Res Notes2013; 6: 146.
[4] Khademi N, Reshadat S, Zangeneh A, Saeidi S, Ghasemi SR, Rajabi-Gilan N, et al. A comparative study of the spatial distribution of HIV prevalence in the metropolis of Kermanshah, Iran, in 1996 2014 using geographical information systems.HIV Med2016; 18(3): 220-224.
[5] Ahmadpour E, Daryani A, Sharif M, Sarvi S, Aarabi M, Mizani A, et al.Toxoplasmosis in immunocompromised patients in Iran: A systematic review and meta-analysis.J Infect Dev Ctries2014; 8(12): 1503-1510.
[6] Granich R, Gupta S, Suthar AB, Smyth C, Hoos D, Vitoria M, et al.Antiretroviral therapy in prevention of HIV and TB: Update on current research efforts.Curr HIV Res2011; 9(6): 446-469.
[7] Mansouri F, Hatami H, Mahdavian B, Hashemian AH. Epidemiology of toxoplasmosis in Kermanshah province.J Kermanshah Univ Med Sci2003; 7(2): 12-19.
[8] Hamzavi Y, Mostafaie A, Nomanpour B. Serological prevalence of toxoplasmosis in meat producing animals.Parasit Vectors2007; 2(1):7-11.
[9] Walle F, Kebede N, Tsegaye A, Kassa T. Seroprevalence and risk factors for Toxoplasmosis in HIV infected and non-infected individuals in Bahir Dar, Northwest Ethiopia.Parasit Vectors2013; 6(1): 1.
[10] Rahimi MT, Mahdavi SA, Javadian B, Rezaei R, Moosazadeh M,Khademlou M, et al. High seroprevalence ofToxoplasma gondiiantibody in HIV/AIDS individuals from North of Iran.Parasit Vectors2015; 10(4):584.
[11] Shen G, Wang X, Sun H, Gao Y. Seroprevalence ofToxoplasma gondiiinfection among HIV/AIDS patients in Eastern China.Korean J Parasitol2016; 54(1): 93.
[12] Gontijo da Silva M, Clare Vinaud M, de Castro AM. Prevalence of toxoplasmosis in pregnant women and vertical transmission ofToxoplasma gondiiin patients from basic units of health from Gurupi,Tocantins, Brazil, from 2012 to 2014.PLoS One2015; 10: e0141700.
[13] Campos FA, Andrade GM, Lanna Ade P, Lage BF, Assumpção MV, Pinto JA. Incidence of congenital toxoplasmosis among infants born to HIV-coinfected mothers: Case series and literature review.Braz J Infect Dis2014; 18(6): 609-617.
[14] Zhang YB, Cong W, Li ZT, Bi XG, Xian Y, Wang YH, et al.Seroprevalence ofToxoplasma gondiiinfection in patients of intensive care unit in China: A hospital based study.Biomed Res Int2015; 2015:908217.
[15] Seyed Alinaghi S, Farhoudi B, Mohraz M, Golsoorat Pahlaviani F,Hosseini M, Farnia M, et al. Prevalence and associated factors of HIV Infection among male prisoners in Tehran, Iran.Arch Iran Med2017;20(6): 356-360.
[16] Sharifi H, Mirzazadeh A, Noroozi A, Marshall BD, Farhoudian A, Higgs P, et al. Patterns of HIV risks and related factors among people who inject drugs in Kermanshah, Iran: A latent class analysis.J Psychoactive Drugs2017; 49(1): 69-73.
[17] Razzaghi EM, Movaghar AR, Green TC, Khoshnood K. Profiles of risk:A qualitative study of injecting drug users in Tehran, Iran.Harm Reduct J2006; 3(1): 1.
[18] Vazirian M, Nassirimanesh B, Zamani S, Ono-Kihara M, Kihara M,Ravari SM, et al. Needle and syringe sharing practices of injecting drug users participating in an outreach HIV prevention program in Tehran,Iran: A cross-sectional study.Harm Reduct J2005; 2(1): 1.
[19] Lashay A, Mirshahi A, Parandin N, Riazi Esfahani H, Mazloumi M,Reza Lashay M, et al. A prospective randomized trial of azithromycin versus trimethoprim/sulfamethoxazole in treatment of toxoplasmic retinochoroiditis.J Curr Ophthalmol2016; 29(2): 120-125.
[20] Low A, Gavriilidis G, Larke N, B-Lajoie MR, Drouin O, Stover J, et al. Incidence of opportunistic infections and the impact of antiretroviral therapy among HIV-infected adults in low-and middle-income countries:A systematic review and meta-analysis.Clin Infect Dis2016; 62(12):1595-1603.
[21] Ngobeni R, Samie A. Prevalence ofToxoplasma gondiiIgG and IgM and associated risk factors among HIV-positive and HIV-negative patients in Vhembe district of South Africa.Afr J Infect Dis2017; 11(2): 1-9.
[22] Yohanes T, Debalke S, Zemene E. LatentToxoplasma gondiiinfection and associated risk factors among HIV-infected individuals at Arba Minch hospital, South Ethiopia.AIDS Res Treat2014; 2014: 652941.
[23] Rezanezhad H, Sayadi F, Shadmand E, Nasab SD, Yazdi HR, Solhjoo K, et al. Seroprevalence ofToxoplasma gondiiamong HIV patients in Jahrom, Southern Iran.Korean J Parasitol2017; 55(1): 99-103.
[24] Kodym P, Malý M, Beran O, Jilich D, Rozsypal H, Machala L, et al.Incidence, immunological and clinical characteristics of reactivation of latentToxoplasma gondiiinfection in HIV-infected patients.Epidemiol Infect2015; 143(3): 600-7.
[25] Xavier GA, Cademartori BG, Cunha Filho NAd, Farias NAdR.Evaluation of seroepidemiological toxoplasmosis in HIV/AIDS patients in the south of Brazil.Rev Inst Med Trop Sao Paulo2013; 55(1): 25-30.
杂志排行
Asian Pacific Journal of Tropical Medicine的其它文章
- An updated systematic review of Zika virus-linked complications
- Biological, chemical and pharmacological aspects of Madhuca longifolia
- Scenario of dengue infection & its control in Pakistan: An up-date and way forward
- Cytotoxic, kinetics of inhibition of carbohydrate-hydrolysing enzymes and oxidative stress mitigation by flavonoids roots extract of Dicoma anomala (Sond.)
- Evaluation of antiparasitic, anticancer, antimicrobial and hypoglycemic properties of organic extracts from Panamanian mangrove plants
- Neuroprotection by misoprostol against rotenone-induced neurotoxicity in rat brain
