The relative value of education of emergency physicians in patient outcome: A retrospective analysis at a single center in developing India
2018-04-12ShastriVandanaSinghShubnumKoleTamorish
Shastri Vandana, Singh Shubnum, Kole Tamorish
Department of Emergency Medicine and Max Institute of Medical Excellence, Max Super Specialty Hospital, Saket, Delhi 110017, India
INTRODUCTION
There is a considerable paucity with regards to the research available on the quality and quantity of clinical teaching in the national emergency department (ED)setups.[1]Medical Council of India (MCI) in July 2009 recognized Emergency medicine (EM) as a specialty.With the onset of the age of modern medicine, the outlook towards to the time worn tradition of triage and detailed medical evaluation must be revoked. Skilled physicians in the emergency department are vitalentity of the new healthcare system and their development is of utmost important task of capacity building in EM.[2]
A number of training programs, most affiliated with foreign universities and ranging from 1 to 3 years were approved by the various healthcare institutes all over the country. A majority of the load fell on to private institutions due to lack of an integrated centralized post graduate training program at the time.[2]It was found that of the majority of hospitals, with the help of private healthcare institutions, had a wide variation in terms of size and volume of patients. Despite many hospitals employing doctors and nursing staff with basic medical knowledge, no trained emergency personnel were available. This led to a poor outlook to Emergency departments as compared to the allocated resources and equipment.[3]
Integrating a formal change in the curriculum,especially in the age old training system of medicine in a country like India is anintricate process. The educational approach varies vastly from the point of view of learners and educators, and is highly impacted by teaching methods, material and instructors’ perceptions and acceptability of educational resources among upcoming emergency physicians.[4]
Just being over half a century old specialty, EM is still in its early ages even in the American healthcare system.[5]So the evaluation of educational approaches by these international scenarios that has occurred after the implementation of many programs need to be evaluated in comparison with our own strategy.[5]As expected this is a long and tedious process and requires years of data collection and analysis for any substantial academia to be produced.
Despite the variety of programs being conducted in the country, a comparable entity common to all is patients’ clinical outcomes which can be measured using simple parameters which can be easily acquired compiling hospital registry entries.
This approach will lead to overall assessment of quality improvement and patient care after implementation of a specified curriculum in the training of young emergency physicians. Not only that, problems in the learning process and possible solutions can also be approached simultaneously.[5]
In the face of increasing emergency department(ED) crowding, balancing education and patient care is a trial of physicians. Multiple studies are being conducted to understand the evaluation of these programs by the physicians and students undergoing the training as well as the faculty conducting the training. These studies have till date shown a good progress when collated with previous data.[6]
Hence, lacking adequate evidence of any actual improvement in patient care and to evaluate the relative value of education of the Emergency doctors on clinical outcomes, a study was advocated which identified the factors to be assessed and compared so as to guide further development of the emergency medicine specialty in India.
METHODS
A retrospective observational study was conducted in the Emergency department of Max hospital, Saket,New Delhi. A period of 22 months prior to the start of the program and like-wise 22 months after initiation of the program was collected from the hospital registry.The period was chosen so as this was the maximum possible data collected prior to the program due to inadequacy of complete records and later period was kept similar to give a relative level of confidence in comparing the data.
The Emergency Medicine program in consideration was the Masters in emergency Medicine (MEM) Program affiliated with George Washington University, NY, USA.This was due to the lack of any central or government post graduate program in the country at the time of the study.
Patients of all age groups and gender registering in the Emergency Department and so were all the doctors working in the ED before and after initiation of the program.
Data was extracted from the hospital registers and compiled on a regular basis by hospital staff. Validity of the data was confirmed by visualized of the records personally by the investigators. Total number of patients visiting ED, total admission through ED per month,total no. of discharged through ED per month, average length of stay- admitted/discharge patients, No. of patient complaint, total no. of LAMA, total no. of patient expired per month data was collected.
No specific sample size was defined or allocated to any of the groups as the footfall of patients
Numerous parameters were considered as per mentioned above in the two groups and compared by applying multiple statistical tests. Minimum of 5% level of significance was considered to be adequate difference to register as any significant value.
All data was kept confidential and blinded statistical analysis conducted. Patient consent was wavered off as per ICMR guidelines as data was extrapolated from hospital registry.
RESULTS
The time frames that were considered included the periods before and after integrating a three-year structured program in emergency medicine. Comparative data in terms of number of patients was obtained when reviewing the total number of patients i.e., 36,145 patients with average patients of 1,642.95 (SD±368.29)per month for years 2009-2010 as compared to 36,440 patients with average per month of 1,656.36 (SD±295.2)for 2012-2013. Whilst the patient number stayed almost similar, the patient data suggests more complicated and critical patients in later years than in the earlier time periods, probably due to increased patient awareness and referral capabilities. Table 1, Figure 1.
The number of patients getting admitted through the emergency in 2009-2010 was 15,021 (mean 682.77 SD±145.731) and in 2012-2013 was 18,940 (mean 860.91 SD±140.307). This quite possibly suggests the improved patient disposition towards in-hospital care along with increased financial status of patients visiting the facility. Table 2, Figure 2.
The total number of patients provisionally diagnosed after evaluation and discharged with only Emergency department management was 20,476 (930.73±247.66)in 2009-2010 to 18,991 (863.23±189.054). This data possibly reflects improved patient diagnostics with improved conversion rates for further evaluation and appropriate management than only being discharged on symptomatic care. Table 3, Figure 3.
The average length of stay of patients in the emergency prior to being admitted to the hospital was 2:55:35 (SD 0:22:43) in 2009-2010 as compared to 4:40:08 (SD 0:57:28). The considerable increase in the duration spent in ER corroborates with the increasing number of inpatient occupancy, increased detailed diagnostics and procedures carried out primarily in the ER prior to appropriate disposition, and increased competency of ED personnel at providing more thorough care to critical as well as noncritical patients awaiting inpatient bed. Table 4, Figure 4.
Similarly, the average length of stay of patients in the emergency prior to being discharged from the ED was 2:22:46 (±0:19:14) in 2009-2010 as compared to 3:58:10(±0:29:31). This too can be extrapolated similarly as to the admission times and additionally to the requisition ofpatients for thorough diagnostics in the emergency itself before discharge. Table 4, Figure 4.

Table 1. Total number of patient visiting ED

Table 2. Total admission through ED per month

Table 3. Total discharge ED month

Table 4. The average length of stay of patients in ED

Table 5. Return to emergency within 24 hours

Figure 1. Total number of patient visiting ED.

Figure 2. Total admission through ED per month.
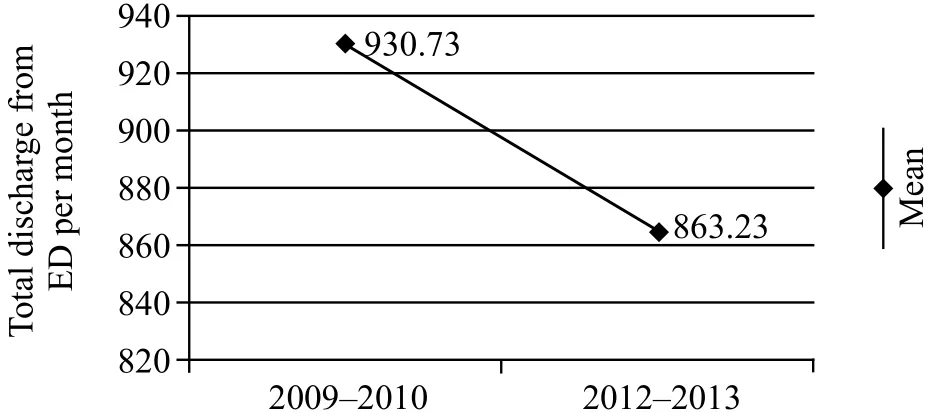
Figure 3. Total discharge from ED per month.
The number of patients returning to the emergency department within 24 hours of discharge or leaving against medical advice from the ED totaled at 72(mean of 3.27, SD 3.807) in 2009-2010 whilst in the time period of 2012 to 2013 the total number was 31(mean 1.41, SD 1.68). This data suggests the improved management of patients with appropriate discharge or referral advice. Table 5, Figure 5.
The number of patient complaints was 56 (mean 2.55, SD 1.565±0.334) in the period 2009-2010 and 35 (mean 1.59, SD 1.709±0.364) in the period 2012-2013. This represents the data reflecting better-quality of patient care as well patient outcomes and overall satisfaction of all the people visiting the emergency department. Table 6, Figure 6.
Patients who left against medical advice from the emergency department surmounted to 2,248 (mean of 102.18, SD 19.331±4.121) from 2009-2010 and 2,246(mean of 102.09, SD 31.213±6.655) from 2012-2013.There seems to be no apparent change in the number of patients going LAMA. However, the reasons for the two periods vary and may include the availability of empaneled coverage and socio-economic reasons. Table 7, Figure 7.
The number of patient deaths in the Emergency department for the time period 2009-2010 was 18 (mean of 0.82, SD 0.907±0.193) and for 2012-2013 was 45(mean of 2.045, SD 3.645±0.777).
Considering the figures of the total and the averages,it can be said that the number of deaths more than doubled in the second time frame of consideration. However, a look at the graphs of the two data when compared gives an idea that there are only last 3 months in the second time period which account for the 31 deaths of the total 45 in this period and only 14 in the rest of the months. This evidently can be correlated with the dengue and H1N1 influenza epidemics in the country at the time and may represent the increased number of very critical patients’ presentation to the ED, either directly but more so on a referral basis from multiple small clinics and private setups located in the nearby surrounding areas. Table 8, Figure 8.
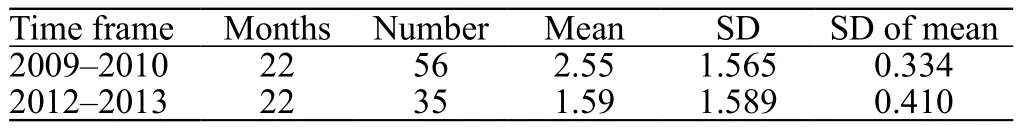
Table 6. The number of patient complaints

Table 7. Total number of LAMA
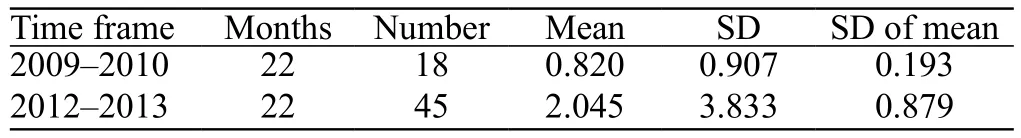
Table 8. Patients expired ED month
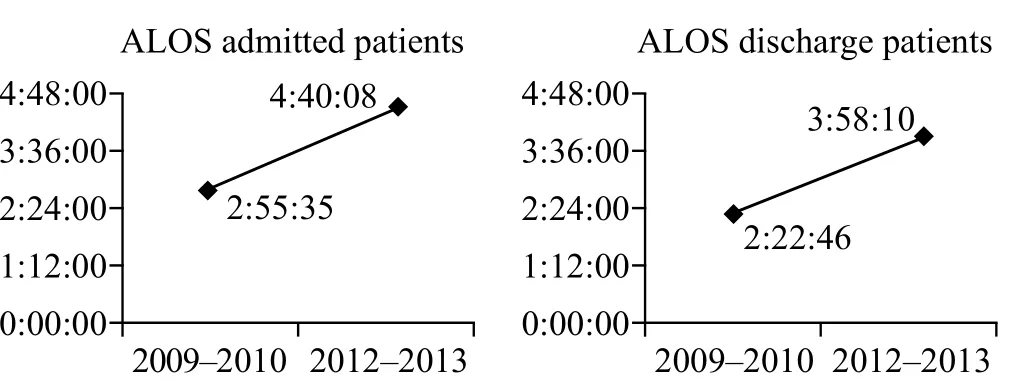
Figure 4. The average length of stay of patients in ED.

Figure 5. Return to emergency within 24 hours.

Figure 6. The number of patient complaints.

Figure 7. Total number of LAMA.

Figure 8. Patients expired ED month.
DISCUSSION
The total data in review had the time periods that took into consideration the periods before and after integration of a three-year structured Academic Program in Emergency Medicine.
The comparative data in terms of number of patients,the total of whom visited the Emergency department,was sizably almost similar even though this data gives a deceptive picture of no change in patient presentation to the emergency department of our study center. However,detailed patient records show that more complicated and critical patients were managed in the ED in later years than in the earlier time periods, probably due to increased patient awareness and referral capabilities.
The number of patients getting admitted through the emergency increased in general and quite possibly suggests the improved patient disposition towards inhospital care along with increased financial status of patients visiting the facility.
The total number of patients provisionally diagnosed after evaluation and discharged with only Emergency department management was lowered. These figures in this study group re fl ect enhanced patient diagnostics with value-added conversion rates for further evaluation and appropriate management than only being discharged on symptomatic care.
The average length of stay of patients in the emergency prior to being admitted to the hospital was 2:55:35 (SD 0:22:43) in 2009-2010 as compared to 4:40:08 (SD 0:57:28) in 2012-2013. The considerable increase in the duration spent in ED corroborates with the increasing number of inpatient occupancy, increased detailed diagnostics and procedures carried out primarily in the ED prior to appropriate disposition, and increased competency of ED personnel at providing more thorough care to critical as well as non-critical patients awaiting inpatient bed.
Similarly, the average length of stay of patients in the emergency prior to being discharged from the ED was 2:22:46 (±0:19:14) in 2009-2010 as compared to 3:58:10(±0:29:31). This too can be extrapolated similarly as to the admission times and additionally to the requisition of patients for thorough diagnostics in the emergency itself before discharge.
The number of patients returning to the emergency department within 24 hours of discharge or leaving against medical advice from the ED totaled at 72(mean of 3.27, SD 3.807) in 2009-2010 whilst in the time period of 2012 to 2013 the total number was 31(mean 1.41, SD 1.68). This data suggests the improved management of patients with appropriate discharge or referral advice.
The number of patient complaints was 56 (mean 2.55, SD 1.565±0.334) in the period 2009-2010 and 35 (mean 1.59, SD 1.709±0.364) in 2012-2013. This represents the data reflecting better-quality of patient care as well patient outcomes and overall satisfaction of all the people visiting the emergency department.
Patients who left against medical advice from the emergency department surmounted to 2,248 (mean of 102.18, SD 19.331±4.121) from 2009-2010 and 2,246(mean of 102.09, SD 31.213±6.655) from 2012-2013.There seems to be no apparent change in the number of patients going LAMA. However, the reasons for the two periods vary and may include the availability of empaneled coverage and socio-economic reasons.
Considering the figures of the total and the averages,it can be said that the number of deaths more than doubled in the second time frame of consideration.However, a look at the graphs of the two data when compared gives an idea that there are only last 3 months in the second time period which account for the 31 deaths of the total 45 in this period and only 14 in the rest of the months. This evidently can be correlated with the dengue and H1N1 in fl uenza epidemics in the country at the time and may represent the increased number of very critical patients’ presentation to the ED, either directly but more so on a referral basis from multiple small clinics and private setups located in the nearby surrounding areas.
CONCLUSION
From the above discussion we can make a coherent conclusion that there is an improvement in the outcome of the entire patient related aspects in the Emergency Department considering the all two time frames included in the study. The difference can be very well attributed to the integration of the structural Academic Program in the development of the Emergency Physicians. This leads us to make a conclusive analysis regarding a positive impact of the Relative Value of Education of Emergency Physicians not only in patient outcome but also in physicians and administrative outlook towards an overall better emergency care.
We are grateful to Dr.Sangram Shinde, Kalden Sherab and Sushant Chhabra for their contribution to part of the study.
Funding:This work was supported by Department of Emergency Medicine and Max Institute of Medical Excellence, Max Super Specialty Hospital, Saket, Delhi 110017, India.
Ethical approval:Not needed.
Conflicts of interest:The authors hav e no competing interests relevant to the present study.
Contributors:All authors read and approved the final version of the manuscript.
1 Hexom B, Seth Trueger N, Levene R, Ioannides KL, Cherkas D.The educational value of emergency department teaching: it is about time. Intern Emerg Med. 2016 Apr 8.
2 Pothiawala S, Anantharaman V. Academic emergency medicine in India. Emerg Med Australas. 2013;25(4):359-64.
3 Khadpe J, Thangalvadi T, Rajavelu P, Sinert R. Survey of the current state of emergency care in Chennai, India. World J Emerg Med. 2011;2(3):169-74.
4 Muller JH, Jain S, Loeser H, Irby DM. Lessons learned about integrating a medical school curriculum: perceptions of students,faculty and curriculum leaders. Med Educ. 2008;42(8):778-85.
5 Hollander H, Loeser H, Irby D. An anticipatory quality improvement process for curricular reform. Acad Med.2002;77(9):930.
6 Ahn J, Golden A, Bryant A, Babcock C. Impact of a dedicated emergency medicine teaching resident rotation at a large urban academic center. West J Emerg Med. 2016;17(2):143-8.
杂志排行
World journal of emergency medicine的其它文章
- Effect of angioembolisation versus surgical packing on mortality in traumatic pelvic haemorrhage: A systematic review and meta-analysis
- The Emergency Department Crash Cart: A systematic review and suggested contents
- Video versus direct laryngoscopy on successful firstpass endotracheal intubation in ICU patients
- Predisposing factors, clinical assessment, management and outcomes of agitation in the trauma intensive care unit
- Outcomes of severe sepsis and septic shock patients after stratification by initial lactate value
- Ventilator management for acute respiratory distress syndrome associated with avian in fl uenza A (H7N9)virus infection: A case series
