Video versus direct laryngoscopy on successful firstpass endotracheal intubation in ICU patients
2018-04-12YongxiaGaoYanboSongZejuanGuJinsongZhangXufengChenHaoSunZhenLu
Yong-xia Gao, Yan-bo Song, Ze-juan Gu, Jin-song Zhang, Xu-feng Chen, Hao Sun, Zhen Lu
Department of Emergency Medicine, the First affiliated Hospital of Nanjing Medical University, Nanjing, China
INTRODUCTION
Airway management in intensive care unit (ICU)patients is challenging.[1]Hypoxemia is common in patients in the ICU requiring intubation, which must be performed rapidly to avoid aspiration because the patient is usually not in a fasted state.[2]Studies have assessed interventions such as routine neuromuscular blockade to improve intubation success rates.[3]Nevertheless,intubation in the ICU still carries higher morbidity and mortality rates compared with intubation in the operating room.[4]
For the past several decades, endotracheal intubation has been performed using the Macintosh laryngoscope for direct laryngoscopy (DL).[5]The video laryngoscope is a recently developed device that contains a miniaturized camera towards the tip of the blades to indirectly visualize the glottis.[6]The video laryngoscopy(VL) is designed to improve the success rate of the physical act of endotracheal intubation, and it has been demonstrated to have utility in anesthesiology practice.By improving glottis visualization, the VL could help to decrease difficult intubation and reduce complications related to intubation in the ICU.[7,8]However, its use in the ICU is more frequent than in operative rooms and its effectiveness in increasing first-pass success and reducing difficult endotracheal intubation or complications related to intubation remain controversial.[9]The aim of this study was to compare the rate of successful first-pass intubation in the ICU by using the DL and that by using the VL in Chinese population.
METHODS
Study design
The present study performed a preliminary,randomized, non-blinded trial comparing first-pass success rate of endotracheal intubation between VL(Med. Adult type Video Laryngoscope VL300M,Zhejiang UE Medical Corp., China) and conventional DL. Patients were recruited in the period from August 2014 to August 2016 at the First Affiliated Hospital of Nanjing Medical University (Nanjing, China).
Inclusion criteria were ICU admission and need for endotracheal intubation to allow mechanical ventilation.Exclusion criteria were: (1) contraindications to endotracheal intubation (e.g., unstable spinal lesion);(2) age younger than 18 years; (3) currently pregnant or breast feeding. The study protocol was reviewed and approved by the Institutional Review Boards for Human Studies of Nanjing Medical University.
Interventions
Laryngoscopy was performed using the device allocated at random (i.e., either a VL which had a requirement to obtain indirect glottis visualization via the camera for the first-pass and had a curved blade similar to the direct laryngoscope, or the DL), the intubation technique with VL is similar to that with DL.Endotracheal tube position was confirmed by analyzing the normal-appearing waveform of the partial pressure of end-tidal exhaled carbon dioxide curve over 4 or more breathing cycles.[10]After tube insertion, the cuff was inflated and the tube was connected to the ventilator.Each introduction of the laryngoscope into the oral cavity was considered a separate laryngoscopy attempt. Firstpass success was defined as the successful placement of an endotracheal tube on the first intubation attempt. If the first-pass intubation attempt failed, repeat laryngoscopy was performed.
Study outcomes
The primary outcome measure was the first-pass success. Other outcomes included: (1) the overall intubation success (the proportion of patients with successful intubation within 3 attempts); (2) total time to successful intubation (time from anesthesia induction initiation to confirmation of good tube position based on partial pressure of end-tidal exhaled carbon dioxide);(3) glottis view as measured by Cormack-Lehane grade[score range from 1 (good) to 4 (no glottis visualization)]and percentage of glottic opening scale score[11][score range from 100% (good) to 0% (no glottis visualization)];(4) difficult intubation (intubation requiring 3 or more attempts, or a total intubation duration longer than 10 minutes, or both);[12](5) complications [death, cardiac arrest, severe cardiovascular collapse (systolic blood pressure <90 mmHg)], hypoxemia [oxygen saturation by pulse oximeter (SpO2) <90%] or severe hypoxemia (SpO2<80%), esophageal intubation, aspiration, arrhythmia(ventricular tachycardia, ventricular fibrillation,ventricular premature beats), and dental injury.
Statistical analysis
Continuous variables were expressed as the mean±standard deviation (SD) or median with interquartile ranges (IQR), as appropriate. Comparisons of continuous variables between independent groups were performed using the two samplettest or Mann-WhitneyUtest, as appropriate. Categorical variables were given as frequencies and percentages. Comparisons of categorical variables were performed by the chi-square test or Fisher’s exact test, as indicated. All the statistical tests were performed in SPSS version 16.0 (SPSS Inc.,Chicago, IL, USA). A two-tailedPvalue of less than 0.05 was considered statistically significant.
RESULTS
Patient baseline data were shown in Table 1. A total of 163 ICU patients underwent endotracheal intubation during the study period. According to the different laryngoscopy devices, 81 patients were assigned to the VL group and 82 patients to the DL group (Figure 1). The average age of the included patients was 69.29±16.22 years. The majority of patients was male, and estimated to be less than 100 kg. The most common indication for intubation was acute respiratory failure. Baseline features were evenly balanced between the two groups.
Endotracheal intubation characteristics of theincluded patients were shown in Table 2. The rate of successful first-pass intubation was not significantly different between the VL group and the DL group(67.9% vs. 69.5%,P=0.824). Moreover, the overall intubation success and total number of attempts to achieve intubation success did not differ between the two groups. In patients with successful first-pass intubation,the median duration of the intubation procedure did not significantly differ between the VL group (3.5 minutes)and the DL group (3 minutes) (P=0.923). The Cormack-Lehane grades of 1 or 2 (better glottis visualization) and the percentage of glottic opening score were similar, and no significant differences were found between the two groups. There were no statistical differences between the VL group and the DL group in intubation complications such as death, cardiac arrest, hypotension, hypoxemia,esophageal intubation, aspiration, arrhythmia, and dental injury.

Table 1. Patient baseline data

Table 2. Intubation characteristics
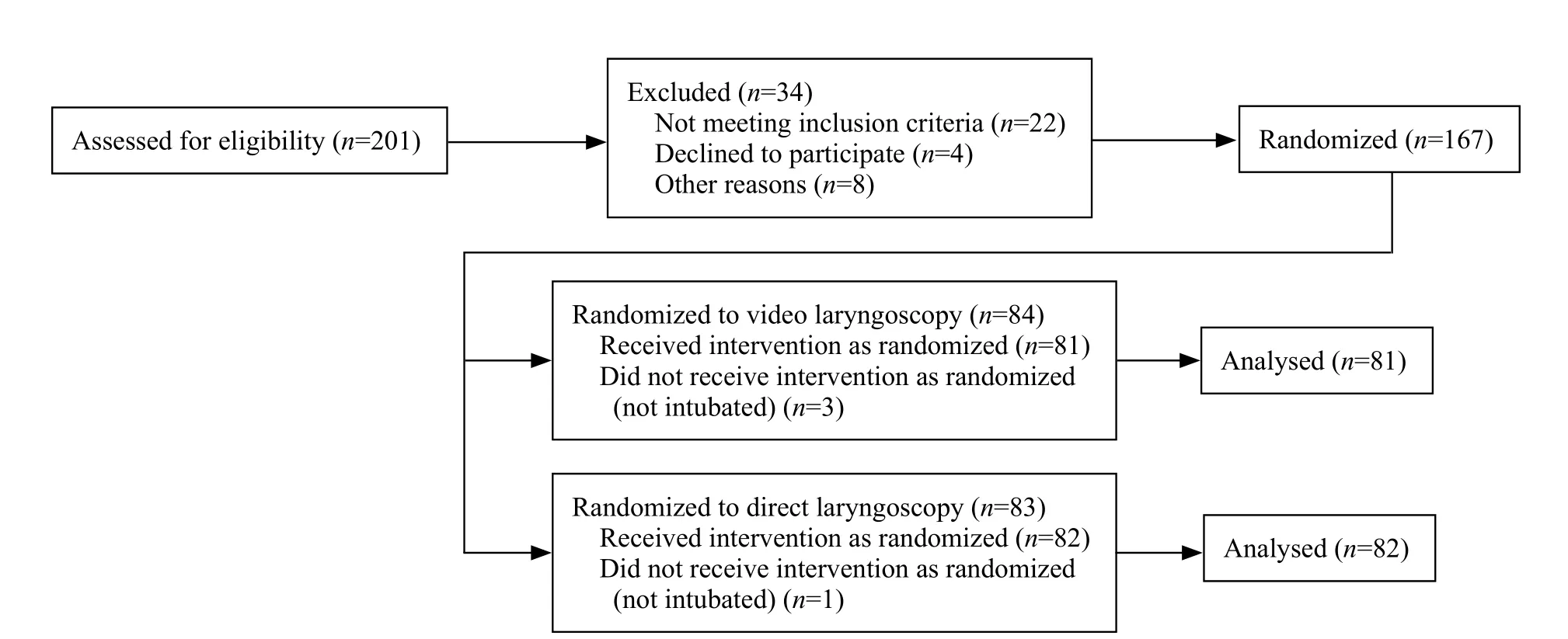
Figure 1. Flow of patients through the video laryngoscopy versus direct laryngoscopy for endotracheal intubation in ICU patients.
DISCUSSION
The VL is a recently developed device that provides indirect visualization of the glottis via a camera, which has either a curved blade similar to the Macintosh laryngoscope or a tube channe.[13]VL has been extensively studied for intubation in the operating room and may facilitate endotracheal intubation compared with DL.[14]In the ICU, previous observational studies supported the use of VL for endotracheal intubation,[15]regardless of the predicted difficulty of intubation. Some of these studies also recorded adverse effects such as longer duration of the intubation procedure and higher mortality.[16,17]A recent systematic review found that VL may help to decrease intubation failure but did not improve the first attempt success.[18]Therefore, whether use of VL in ICUs is of greater benefit to patients deserves investigation. This study was designed to test the hypothesis that routine use of the VL for endotracheal intubation of patients in the ICU increased the rate of successful first-pass intubation compared with use of the DL. Meanwhile, this study added an objective primary outcome measure (capnography) to ensure a low risk of bias and high external validity.
Some previous studies had indicated that VL could improve the first-pass endotracheal intubation success rate compared with DL.[19,20]However, other studies failed to show improvements in VL compared with DL.[21,22]In a recent randomized clinical trial of 371 adults, the author found VL failed to improve first-pass endotracheal intubation rates and was associated with higher rates of severe life-threatening complications.[23]The present study suggested that VL did not improve the rate of successful intubation on the first attempt compared with DL.
Several factors may explain the discrepancy in results of early studies vs. recent RCTs, one of which was a high success rate in the DL group, related in particular to adherence to a standardized protocol,including routine sedation agents.[23]In addition,improved glottis visualization with VL was not translated into a higher success rate of first-pass intubation because tracheal catheterization under indirect vision was more difficult.[24]Conceivably, a VL with an intubation channel might improve the success rate, although preliminary data obtained in the operating room were inconclusive,[23]which requires further studies to assess the comparative effectiveness.
The present study found the frequency of intubation complications was similar between the VL and the DL group, which was incomplete consistent with the results reported previously. The better visualization of the glottis with VL might lead to a false impression of safety when intubation is performed. In addition, poorer alignment of the pharyngeal axis, laryngeal axis, and mouth opening despite good glottis visualization by VL could lead to mechanical upper airway obstruction and faster progression to hypoxemia.[24]
Endotracheal intubation performed by the anesthesiologist in the operating room has a low complication rate, because the patients are prescreened for difficult airway problems and have stable physiology,and the practitioner who experiences unanticipated difficulties often has the back out and wake-up option.[2]Furthermore, anesthesiologists have excellent manual skills in intubation, and have the advantage of extensive procedure practice. Endotracheal intubation in the ICU patients presents a different set of challenges. The patient may have an unrecognized difficult airway, minimal physiological reserve due to cardiopulmonary failure,and there is no back out or wake-up option. The rate of difficult intubation did not differ between the two groups in this study.[18]The difficult airway characteristics included bleeding, emesis, obstruction, restricted mouth opening, and obesity, etc.[25]The main reason for patients to experience first-pass intubation failure was because the glottis was not visualized during DL. For patients in the VL group, first-pass intubation failure was due to failure of tracheal catheterization. Therefore, the clinical application should take the concrete patients’ conditions and environment into consideration.
VL has been shown to improve the physicians’view of the glottic opening, while this study failed to detect differences between the VL and the DL group.The present study examined both the Cormack-Lehane and percentage of glottic opening scores as both have previously been studied. Although these scores are commonly used, there are other tools that may help to better discriminate the challenges physicians encounter during intubation such as the intubation difficulty scale,[26]which incorporates multiple aspects including the number of attempts, number of operators, alternative devices if used, Cormack-Lehane grade, amount of force required, position of the vocal cords, and external laryngeal pressure if applied.
This study also presents several limitations. First,this was a randomized study, but not a multicenter trial,and with a limited amount and quality of data. Second,physician intubation expertise requires theoretical skills,manikin practice, and supervised hands-on training,which cannot be precisely defined individually. Third,it assessed a single type of video laryngoscope in the present study, which has a curved blade similar to the direct laryngoscope. Other video laryngoscopes with a hyperangulated blade or specific intubation channel might produce different results.
CONCLUSIONS
Among patients in the ICU requiring intubation,VL, compared with DL, did not improve the rate of successful first-pass endotracheal intubation. Further studies in multicenter, larger patient populations are desirable to assess the comparative effectiveness of these two strategies in different clinical settings and among operators with diverse skill levels.
Funding:None.
Ethical approval:The study was approved by the Institutional Review Boards for Human Studies of Nanjing Medical University.
conflicts of interest:There is no conflict of interest related to this study.
Contributors:YXG and YBS contributed equally to this work.YXG proposed the study, analyzed the data and wrote the first drafts. All authors contributed to the design and interpretation of the study and to further drafts.
1 De Jong A, Molinari N, Conseil M, Coisel Y, Pouzeratte Y,Bela fi a F, et al. Video laryngoscopy versus direct laryngoscopy for endotracheal intubation in the intensive care unit: a systematic review and meta-analysis. Intensive Care Med.2014;40(5):629-39.
2 Jaber S, Amraoui J, Lefrant JY, Arich C, Cohendy R, Landreau L, et al. Clinical practice and risk factors for immediate complications of endotracheal intubation in the intensive care unit: a prospective, multiple-center study. Crit Care Med.2006;34(9):2355-61.
3 Mosier JM, Sakles JC, Stolz U, Hypes CD, Chopra H, Malo J,et al. Neuromuscular blockade improves first-attempt success for intubation in the intensive care unit. A propensity matched analysis. Ann Am Thorac Soc. 2015;12(5):734-41.
4 Griesdale DE, Bosma TL, Kurth T, Isac G, Chittock DR.Complications of endotracheal intubation in the critically ill.Intensive Care Med. 2008;34(10):1835-42.
5 Campbell SG, Magee KD, Zed PJ, Froese P, Etsell G, LaPierre A, et al. End-tidal capnometry during emergency department procedural sedation and analgesia: a randomized, controlled study. World J Emerg Med. 2016;7(1):13-8.
6 Griesdale DE, Liu D, McKinney J, Choi PT. Glidescope®video-laryngoscopy versus direct laryngoscopy for endotracheal intubation: a systematic review and meta-analysis. Can J Anaesth. 2012;59(1):41-52.
7 De Jong A, Clavieras N, Conseil M, Coisel Y, Moury PH, Pouzeratte Y, et al. Implementation of a combo videolaryngoscope for intubation in critically ill patients:a before-after comparative study. Intensive Care Med.2013;39(12):2144-52.
8 Kory P, Guevarra K, Mathew JP, Hegde A, Mayo PH. The impact of video laryngoscopy use during urgent endotracheal intubation in the critically ill. Anesth Analg. 2013; 117(1):144-9.
9 Larsson A, Dhonneur G. Videolaryngoscopy: towards a new standard method for tracheal intubation in the ICU? Intensive Care Med. 2013;39(12):2220-2.
10 Silvestri S, Ladde JG, Brown JF, Roa JV, Hunter C, Ralls GA, et al. Endotracheal tube placement con fi rmation: 100% sensitivity and specificity with sustained four-phase capnographic waveforms in a cadaveric experimental model. Resuscitation.2017;115:192-8.
11 Levitan RM, Ochroch EA, Kush S, Shofer FS, Hollander JE. Assessment of airway visualization: validation of the percentage of glottic opening (POGO) scale. Acad Emerg Med.1998;5(9):919-23.
12 Lascarrou JB, Boisrame-Helms J, Bailly A, Le Thuaut A, Kamel T,Mercier E, et al. Video Laryngoscopy vs Direct Laryngoscopy on Successful First-Pass Orotracheal Intubation Among ICU Patients:A Randomized Clinical Trial. JAMA. 2017;317(5):483-93.
13 Silverberg MJ, Kory P. Survey of video laryngoscopy use by U.S.critical care fellowship training programs. Ann Am Thorac Soc.2014;11(8):1225-9.
14 Wadman MC, Dierks TW, Branecki CE, Barthold CL, Hoffman LH, Lander L, et al. Comparison of Airtraq optical laryngoscope and Storz video laryngoscope in a cadaver model. World J Emerg Med. 2011;2(3):175-8.
15 Silverberg MJ, Li N, Acquah SO, Kory PD. Comparison of video laryngoscopy versus direct laryngoscopy during urgent endotracheal intubation: a randomized controlled trial. Crit Care Med. 2015;43(3):636-41.
16 Platts-Mills TF, Campagne D, Chinnock B, Snowden B,Glickman LT, Hendey GW. A comparison of GlideScope video laryngoscopy versus direct laryngoscopy intubation in the emergency department. Acad Emerg Med. 2009;16(9):866-71.
17 Takenaka I, Aoyama K. Prevention of aspiration of gastric contents during attempt in tracheal intubation in the semi-lateral and lateral positions. World J Emerg Med. 2016;7(4):285-289.
18 Lewis SR, Butler AR, Parker J, Cook TM, Smith AF.Videolaryngoscopy versus direct laryngoscopy for adult patients requiring tracheal intubation. Cochrane Database Syst Rev.2016;11:CD011136.
19 Lakticova V, Koenig SJ, Narasimhan M, Mayo PH. Video laryngoscopy is associated with increased first pass success and decreased rate of esophageal intubations during urgent endotracheal intubation in a medical intensive care unit when compared to direct laryngoscopy. J Intensive Care Med.2015;30(1):44-8.
20 Mosier JM, Whitmore SP, Bloom JW, Snyder LS, Graham LA, Carr GE, et al. Video laryngoscopy improves intubation success and reduces esophageal intubations compared to direct laryngoscopy in the medical intensive care unit. Crit Care.2013;17(5):R237.
21 Ducharme S, Kramer B, Gelbart D, Colleran C, Risavi B,Carlson JN. A pilot, prospective, randomized trial of video versus direct laryngoscopy for paramedic endotracheal intubation.Resuscitation. 2017;114:121-6.
22 Michailidou M, O’Keeffe T, Mosier JM, Friese RS, Joseph B,Rhee P, et al. A comparison of video laryngoscopy to direct laryngoscopy for the emergency intubation of trauma patients.World J Surg. 2015;39(3):782-8.
23 Corso RM, Zampone S, Baccanelli M, Sorbello M, Gambale G.Prehospital difficult airway management: old things still work.World J Emerg Med. 2014;5(1):75-6.
24 Hirabayashi Y, Fujita A, Seo N, Sugimoto H. Distortion of anterior airway anatomy during laryngoscopy with the GlideScope videolaryngoscope. J Anesth. 2010;24(3):366-72.
25 Takenaka I, Aoyama K. Prevention of aspiration of gastric contents during attempt in tracheal intubation in the semi-lateral and lateral positions. World J Emerg Med. 2016;7(4):285-9.
26 Adnet F, Borron SW, Racine SX, Clemessy JL, Fournier JL,Plaisance P, et al. The intubation difficulty scale (IDS): proposal and evaluation of a new score characterizing the complexity of endotracheal intubation. Anesthesiology. 1997; 87(6):1290-7.
杂志排行
World journal of emergency medicine的其它文章
- Effect of angioembolisation versus surgical packing on mortality in traumatic pelvic haemorrhage: A systematic review and meta-analysis
- The Emergency Department Crash Cart: A systematic review and suggested contents
- Predisposing factors, clinical assessment, management and outcomes of agitation in the trauma intensive care unit
- Outcomes of severe sepsis and septic shock patients after stratification by initial lactate value
- Ventilator management for acute respiratory distress syndrome associated with avian in fl uenza A (H7N9)virus infection: A case series
- Comparison of sedative effectiveness of thiopental versus midazolam in reduction of shoulder dislocation
