Comparison of sedative effectiveness of thiopental versus midazolam in reduction of shoulder dislocation
2018-04-12ElnazVahidiRezvanHematiMehdiMomeniAmirhosseinJahanshirMortezaSaeedi
Elnaz Vahidi, Rezvan Hemati, Mehdi Momeni, Amirhossein Jahanshir, Morteza Saeedi
Emergency Medicine Research Center, Shariati Hospital, Emergency Medicine Department, Tehran University of Medical Sciences, Tehran, Iran
INTRODUCTION
The emergency department (ED) is a unique environment where a variety of procedures with emergent and urgent indications are managed. Many of these procedures result in significant pain and are associated with varying degrees of anxiety and agitation.Accordingly, the management of sedation and analgesia is an important component of comprehensive emergency medical care for patients of all ages. Controlling anxiety may improve quality of care and patient satisfaction by facilitating interventional procedures and minimizing patient suffering.
Among different procedures done in emergency room, replacing joint dislocations occur frequently.Anterior shoulder dislocation is the most commonly dislocated joint that necessitates emergency referral and reduction. Most (90%-97%) shoulder dislocations are anterior.[1]It consists of up to 50% of all joint dislocations. In 70% of cases it is seen in people under 30 years old.[2]Patients must have their shoulder muscles relaxed before any reduction can be easily effected so analgesic and muscle-relaxing medications are required. Procedural sedation and analgesia(PSA) refers to the use of analgesic, dissociative, and sedative agents to relieve pain and anxiety associated with diagnostic and therapeutic procedures performed in various settings. PSA is an integral element of emergency medicine. Various drugs have been tried to alleviate pain and anxiety in patients suffering shoulder dislocation for example midazolam+ fentanyl or midazolam+ ketamine are among most popular combinations in PSA.[3]In recent years etomidate has favorably been chosen as an induction agent in contrast to other drugs because of the low risk of apnea and hypotension.[4-6]While doing PSA, patients should be monitored closely with capnography.[3,7]
Midazolam is a benzodiazepine and its clinical effects are sedation, motion control and anxiolytic. Its initial IV sedative dose is 0.05-0.1 mg/kg or 1 mg and then titrated to max dose of 5 mg. As IV form, it has an onset of action near 2-3 minutes and duration of sedation is 45-60 minutes.[8]
Thiopental has been used in different short surgeries.Its clinical action is sedation, motion control and anxiolytic. It has a very short onset of action near 10-15 seconds and half-life is almost 5-10 minutes. Initial IV sedative dose is 3-4 mg/kg or 50-100 mg first then repeated every 10 minutes[8,9]
Falk et al[6]in 2004 did a systematic review to compare the efficacy and safety of etomidate for PSA in ED. They found that etomidate’s onset of action and time to recovery was rapid and comparable to that of thiopental but significantly faster than that of midazolam.
Burton et al[5]in 2002 conducted a randomized controlled trial to compare etomidate and midazolam for reduction of anterior shoulder dislocation. They concluded that etomidate provided effective PSA and when compared with midazolam it conferred a significantly shorter period of PSA.
The only study compared midazolam and thiopental’s sedation, was by Barry A. R. Bland in 1987 that evaluated the two drugs for rapid sequence anesthetic induction for elective cesarean section. They showed that maintenance of anesthesia and hemodynamic responses were identical in both groups but they concluded that midazolam was less suitable than thiopental for anesthetic induction.[10]
Since there are not enough studies about sedative effect of thiopental in procedures, we conducted an RCT to compare thiopental with midazolam in reduction of shoulder dislocation. Our primary outcomes were number of times other methods except tractioncounteraction were used and the degree of muscle relaxation was induced by thiopental.
METHODS
Participants
We conducted a randomized double blind parallel group study (with block randomization) in patients with shoulder dislocation recruited from the EDs of Shariati and Imam Khomeini Hospitals, two tertiary referral center, from August to December 2014. We got the approval from the ethics committee of Tehran University of Medical Sciences. Eligible patients were aged >18 years old who were diagnosed with anterior shoulder dislocation based on their clinical findings and X rays. We excluded patients with other types of shoulder dislocation, severe neurovascular injury,dislocation longer than 24 hours, fracture dislocation,multiple trauma mechanism, no consent to participate in the study, decreased level of consciousness, systolic hypotension<90 mmHg, drugs hypersensitivity, illicit drug use, age<18 years, pregnancy or hepatorenal disorders (Figure 1). The treating emergency physician confirmed the diagnosis and contacts the chief investigator. The subjects were randomly divided into two groups of 35 each: a midazolam group (A) and a thiopental group (B). One of our triage nurses used a random number table to block randomize subjects, she was the only person aware of this randomization. Each patient had a code in block randomization, and only the chief investigator and the triage nurse were aware of the assignment and patient’s group. The specified drug and dose were provided by the triage nurse based on the code (all syringes covered) and injected to the patient by the emergency physician who was blinded to the study.All dislocations were anterior and initially reduced by traction-countertraction and if it was unsuccessful, other methods would be tried and recorded. All study outcomes were evaluated and recorded by the emergency physician doing the procedure, who was blinded to the patient group.
Drug administration
All patients were interviewed and the method of drug administration, visual analogue pain score (VAS; where 10 represented the worst imaginable pain and 0 was pain-free) and possible complications were explained to them and informed written consent was obtained.Demographic data including age, sex, number of times other methods except traction-countertraction were used, patients and physician’s satisfaction, difficulty of procedure, degree of muscle relaxation, time of sedation and complete recovery, number of patients had apnea episode, O2saturation, patient’s pain score before drug infusion and after procedure completion and adverse events were all recorded by the emergency physician responsible for the patients. In group A 0.1 mg/kg IV midazolam+ 2 µg/kg IV fentanyl and in group B 2 mg/kg IV thiopental+ 2 µg/kg IV fentanyl were administered.Both drug syringes were covered in order to not recognize them based on their color.
Statistical analysis and sample size calculation
For sample size calculation we used the variable“number of times the procedure was repeated by other methods except traction-counteraction” as the main primary outcome. Based on the reference number 12,in order to produce statistically significant difference between the two groups, with Power of 90%,CIof 95%,a sample size of 15 per treatment group was calculated by means of the following formula:
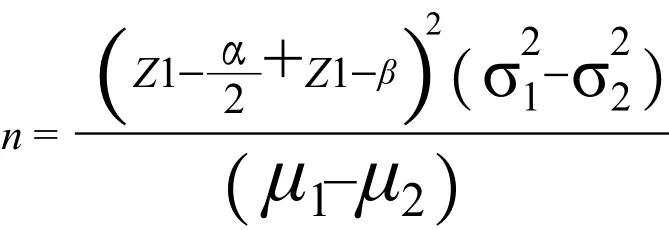
Because one of our drugs, thiopental was not studied with this purpose in PSA, we supposed the error 100%and estimated a sample size 30 patients in each group.All data were analyzed using SPSS V.22 software. In order to evaluate the normal distribution of quantitative data such as VAS score, we conducted a Kolmogorov-Smirnov (KS) test. We analyzed normally distributed continuous data by independentttest and median of ordinal, non-continuous and non-normal data by analysis of Mann-WhitneyUtest. We analyzed normally distributed qualitative data by Chi square test.
RESULTS
During the study period 80 patients were diagnosed with shoulder dislocation and 10 patients were excluded:2 patients had posterior shoulder dislocation, 2 didn’t consent to participate in the study, three had fracture dislocation, 1 patient were <18 y/o and 2 patients had neurovascular impairment. The remaining 70 patients were randomly divided into two groups of 35 each(Figure 1).
The mean ages of group A and B were similar(25.77±3.69 and 27.94±5.56 years, respectively)(P-value=0.60). Incidentally all patients were men (Table 1). Side effects including apnea episode are shown in Table 2. Apnea episodes had no significant difference between the two groups (P-value=0.39).

Table 1. Demographic feature of study groups (% of all patients in each group)

Figure 1. CONSORT fl ow diagram.
Table 3 describes study end points. Before drug infusion the mean±SD VAS scores were 8.37±2.21 in the midazolam group (A) and 8.94±1.78 in the thiopental group (B); mean difference 0.57, 95%CI= -0.38 to 1.52(P-value=0.238). After completion of the procedure, the mean ±SD VAS scores in groups A and B were 3.20±1.30 vs. 3.65±1.30; mean difference -0.45, 95%CI=-1.07 to 0.16 (P-value=0.147).
Muscle tone in group B decreased more (P-value=0.014).Performing the procedure in group B was easier than in group A (P-value=0.043). There were no significant difference in time of sedation and complete recovery,patient and doctor satisfaction, or O2saturation between the study groups. Within each group O2saturation was reduced significantly during dislocation replacement(P-value=0.000). There was no need to conduct other maneuvers for reduction, except traction-countertraction,in either group.
DISCUSSION
This study demonstrated that muscle tone was decreased and relaxed more with thiopental sedation than midazolam and PSA with thiopental was easier than midazolam in reduction of shoulder dislocation. Patient and doctor’s satisfaction, O2saturation, risk of apnea,number of other reduction methods used except tractioncountertraction and patients’ pain score had no significant difference between the study groups. Three patients in group B and none in group A had nausea and vomiting.
Midazolam has been used as sedative in different procedures with a relatively short-acting time, few hemodynamic effects and significant anterograde amnesic properties. As IV form, it has an onset of action near 2-3 minutes and duration of sedation is 45-60 minutes.[8]
Thiopental clinical action is sedation, motion control and anxiolysis. It has a very short onset of action near 10-15 seconds and half-life is almost 5-10 minutes.Initial IV sedative dose is 3-4 mg/kg or 50-100 mg first then repeated every 10 minutes[8,9]
Etomidate has been recently evaluated with midazolam and thiopental in different setups. In 2005 Hunt GB et al compared etomidate with midazolam and concluded that etomidate could provide a significant reduction in recovery time while providing equal sedation quality.[4]In 2002 Burton et al[5]tried etomidate and midazolam for reduction of anterior shoulder dislocation and they found that etomidate provided a significantly shorter period of PSA. Falk et al[6]in 2004 showed that etomidate onset of action and time to recovery were rapid and comparable to that of propofol and thiopental but significantly faster than that of midazolam.
One study that compared midazolam and thiopental sedation, by Wakamoto et al[10]in 1987, evaluated the two drugs for rapid sequence anesthetic induction for elective cesarean section. They showed that maintenance of anesthesia and hemodynamic responses were identical in both groups but midazolam was less suitable than thiopental for anesthetic induction.
Bland et al[11-13]evaluated sedative effect of propofolfentanyl vs. thiopental-sevoflurane in diagnostic bronchoscopy and they added that the first group performed better anesthesia than the second because of its superior maintenance of cardiovascular stability.
In conclusion, from the sedative viewpoint, thiopental proved an effective intravenous anxiolytic agent for shoulder dislocation reduction, comparable in most respects to midazolam. Thiopental had some theoretical advantages like more relaxation and reduction in muscle tone and shorter sedative and complete recovery time.
Limitations of the study
One limitation of our study was that we were notable to determine the onset of action of both drugs. Our sample size was not sufficient to detect the exact drugs’effects and adverse events. Further clinical trials with larger sample sizes and longer follow-up should therefore be performed to identify adverse events.
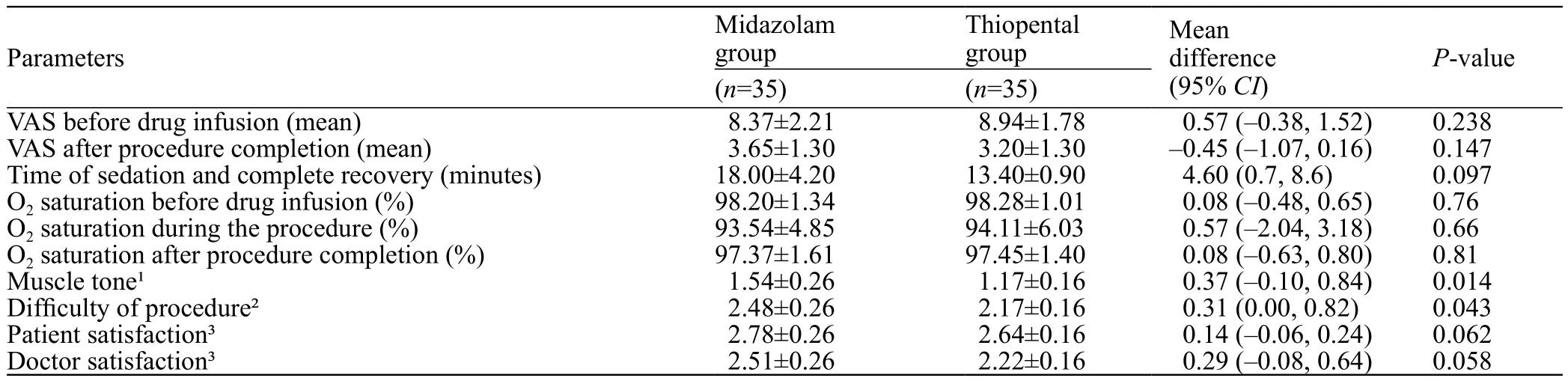
Table 3. Comparison of primary outcomes of study groups
CONCLUSION
This study shows that thiopental sedation might be as effective as midazolam in replacement of shoulder dislocation with more reduction in muscle tone.
Funding:This study was not funded.
Ethical approval:The study was approved by ethics committee of Tehran University of Medical Sciences.
Conflicts of interest:The authors state they have no competing interests.
Contributors:MS: study design and supervision; RH: data gathering and analysis; EV: data analysis and drafting; MM: data gathering and drafting; MS: critical revision.
1 Schubert H. Emergency case: reducing anterior shoulder dislocation. Clinical challenge, DEFI clinique. 2002; 48:469-72
2 Riebel GD, McCabe JB. Anterior shoulder dislocation: A review of reduction techniques. Am Emerg Med J. 1991;9(2):180.
3 Reichman EF, Simon RR. Emergency Medicine Procedures.New York: McGraw-Hill, 2004;9.
4 Hunt GS, Spencer MT, Hays DP. Etomidate and midazolam for procedural sedation: Prospective, randomized trial. Am Emerg Med J. 2005;23(3):299.
5 Burton JH, Bock AJ, Strout TD, Marcolini EG. Etomidate and midazolam for reduction of anterior shoulder dislocation. Ann Emerg Med J. 2002;40(5):496-504.
6 Falk J, Zed PJ. Etomidate for procedural sedation in emergency department. Ann of Pharma. 2004;38(8):1272-7.
7 Butler M, Froese P, Zed P, Kovacs G, MacKinley R, Magee K,et al. Emergency department procedural sedation for primary electrical cardioversion - a comparison with procedural sedations for other reasons.World J Emerg Med. 2017;8(3):165-9.
8 Roberts JR. Hedges and Roberts’ Clinical procedures in emergency medicine. 2014; 33:598-9.
9 Wakamoto H, Nakamura Y, Ebihara T, Tokuda K, Ohmori H. Reversible coma associated with prolonged high-dose phenobarbital therapy in bilateral Sturge-Weber syndrome. J Child Neurol. 2009;24(12):1547-51. Epub 2009 Aug 11.
10 Uchida T, Takayanagi M, Kitamura T, Nishio T, Numata Y, Endo W, et al. High-dose phenobarbital with intermittent short-acting barbiturates for acute encephalitis with refractory, repetitive partial seizures. Pediatr Int. 2016;58(8):750-3.
11 Bland BA, Lawes EG, Duncan PW, Warnell I, Downing JW.Comparison of midazolam and thiopental for rapid sequence anesthetic induction for elective cesarean section. Anesth Analg.1987;66(11):1165-8.
12 Yamaguchi S, Koguchi T, Midorikawa Y, Okuda Y, Kitajima T. Comparative evaluation of TIVA with propofol-fentanyl and thiopental-sevoflurane anesthesia using laryngeal mask airway for diagnostic bronchoscopy. J Anesth. 1998;12(2):53-6.
13 Taylor DM, O’Brien D, Ritchie P, Pasco J, Cameron PA.Propofol versus midazolam/ fentanyl for reduction of anterior shoulder dislocation. Acad Emerg Med. 2005; 12(1): 13-9.
杂志排行
World journal of emergency medicine的其它文章
- Effect of angioembolisation versus surgical packing on mortality in traumatic pelvic haemorrhage: A systematic review and meta-analysis
- The Emergency Department Crash Cart: A systematic review and suggested contents
- Video versus direct laryngoscopy on successful firstpass endotracheal intubation in ICU patients
- Predisposing factors, clinical assessment, management and outcomes of agitation in the trauma intensive care unit
- Outcomes of severe sepsis and septic shock patients after stratification by initial lactate value
- Ventilator management for acute respiratory distress syndrome associated with avian in fl uenza A (H7N9)virus infection: A case series
