全身弥散加权成像与PET-CT及颅脑MRI在肺癌分期诊断中的对照研究
2017-12-23谈炎欢李俊晨
谈炎欢,李俊晨
南京中医药大学附属常熟医院 放射科,江苏 常熟 215500
全身弥散加权成像与PET-CT及颅脑MRI在肺癌分期诊断中的对照研究
谈炎欢,李俊晨
南京中医药大学附属常熟医院 放射科,江苏 常熟 215500
目的确定全身磁共振弥散加权成像(Whole Body Diffusion Weighted Imaging, WB-DWI)肺癌分期的诊断性能是否优于PET-CT联合颅脑MRI。方法用于肺癌分期与术前PET-CT联合颅脑MRI和WB-DWI检查的肺癌患者30例。其中鳞癌22例,腺癌6例,小细胞癌2例。对肺癌分期的准确性采用McNemar检验和卡方检验进行统计分析。结果PET-CT正确识别病理N分期23例(76.67%),2例被高估(6.67%)和5例被低估(16.67%),分期准确性为0.767。WB-DWI正确识别病理N分期26例(86.67%),1例被高估(3.33%)和3例被低估(10%),分期准确性为0.867,准确性差异无统计学差异。PETCT联合颅脑MRI正确分期20例(66.67%),3例被高估(10%)和7例被低估(23.33%),分期准确性为0.667。WB-DWI正确分期21例(70%),2例被高估(6.67%)和7例被低估(23.33%),分期准确性为0.7,准确性差异无统计学差异。结论WB-DWI对肺癌的分期诊断性能优于PET-CT联合颅脑MRI。
磁共振成像;正电子发射断层扫描成像;全身弥散加权成像;肺癌;分期
引言
男性肺癌发病率和死亡率均占所有恶性肿瘤的第一位,转移是恶性肿瘤发生和演变过程中最危险的阶段[1]。故肺癌准确地术前分期至关重要,不同的分期治疗方法也不尽相同。目前肺癌的术前分期主要依靠PET-CT和颅脑MRI。虽然PET-CT可作为金标准,但程序复杂,基层医院装备少。而作为类PET的全身磁共振弥散加权成像(Whole Body Diffusion Weighted Imaging, WB-DWI)简便易操作,且无辐射,较PET-CT便宜,已应用于肺癌的临床分期[2-3]。本研究通过WB-DWI与PET-CT及颅脑MRI的比较,评估WB-DWI在肺癌术前分期中的价值。
1 资料与方法
1.1 一般资料
收集本院2015年3月~2017年3月肺癌手术患者30例,30例患者均于两周内分别行颅脑MRI与WB-DWI检查,且均有上级医院PET-CT检查资料。30例患者通过告知检查事项并签署知情同意书。男23例,女7例,平均年龄62.27±2.29岁(38~82岁),其中鳞癌22例,腺癌6例,小细胞癌2例。25例患者行肺叶切除和周围淋巴结清扫,5例行肺楔形切除或肺段切除。TNM分期根据2009年第7版UICC标准[4]。
1.2 MRI扫描参数
磁共振成像采用1.5 T扫描仪(Magnetom Avanto,Siemens)。WB-MRI采用短T1反转恢复平面回波(Short T1 Inversion Recovery Echo Planner Imaging,STIR-EPI) 序列;患者空腹取仰平卧位,头先进,平静呼吸,扫描范围自头颅至股骨上段,包括双侧腹股沟区,分8个部位进行扫描,激光标志线定位于下颌骨颏突水平,扫描完成后对8段原始图像进行无缝重组,然后利用3D-MIP重建及黑白反转技术进行三维重建。WB-DWI参数:TR=13800 ms,TE=76 ms,b值 为 50和 1000 s/mm2,FOV=450 mm,层厚5.0 mm,Matrix为340×340,扫描时间为808 s。
颅脑MRI扫描:仰卧位,头颅线圈放置,定位眶耳线,进行轴位平扫及增强扫描,造影剂为钆喷酸葡 胺(0.2 mmol/kg)。T2WI:TR=5000 ms,TE=96 ms,FOV=230 mm, 层 厚 5.0 mm,Matrix为 60×40;T1WI:TR=550 ms,TE=8.7 ms,FOV=230 mm, 层 厚 5.0 mm,Matrix为60×40,扫描时间为20 min。
1.3 图像分析
WB-DWI图像的分期诊断由两位磁共振5年和3年诊断经验的影像科医生独立完成。两位医师再对患者的PETCT联合颅脑MRI资料进行分期诊断。如有分歧则协商后完成。两位医师除知晓肺癌的临床诊断外,对其它信息均未知。诊断标准为2009年第7版UICC的TNM分期标准,将WB-DWI和PET-CT联合颅脑MRI的分期结果分别与术后病理结果对照。
1.4 统计学分析
统计分析使用STATA 13.1软件MP版。数据以平均值±标准差表示。全身DWI与PET-CT及颅脑MRI对肺癌分期的准确性采用McNemar检验和卡方检验,分别对敏感性、特异性、阳性预测值(Positive Predictive Value,PPV)和阴性预测值(Negative Predictive Value,NPV)进行比较。P<0.05表示有统计学意义。
2 结果
PET-CT+颅脑MRI和WB-DWI的肺癌诊断图像,见图1。由PET-CT或WB-DWI检查获得的临床N分期(cN)及病理结果分析N分期(pN)之间的关系,见表1。PET-CT正确识别病理N分期有23例(76.67%),有2例被高估和5例被低估,分别占比为6.67%和16.67%,具有0.767的分期准确性。WB-DWI正确识别病理N分期有26例(86.67%),有1例被高估和3例被低估,分别占比为3.33%和10%,具有0.867的分期准确性。两者之间的准确性差异无统计学意义(P=0.125)。同样,WB-DWI检查与PET-CT之间在敏感性、特异性、阳性预测值、阴性预测值上没有显著性差异(表2)。
由PET-CT联合颅脑MRI或WB-DWI检查获得的肺癌临床分期(cS)及病理结果分析的肺癌临床分期(pS)之间的关系,见表3。PET-CT+颅脑MRI能正确地确定病理分期的有20例(66.67%),有3例被高估和7例被低估,分别占比为10%和23.33%,分期准确性为0.667。WB-DWI能正确地确定病理分期的有21例(70%),有2例被高估和7例被低估,分别占比为6.67%和23.33%,分期准确性为0.7。WB-DWI分期准确性为0.7,PET-CT联合颅脑MRI的分期准确性为0.667,两者之间的差异无统计学意义(P=0.157)。
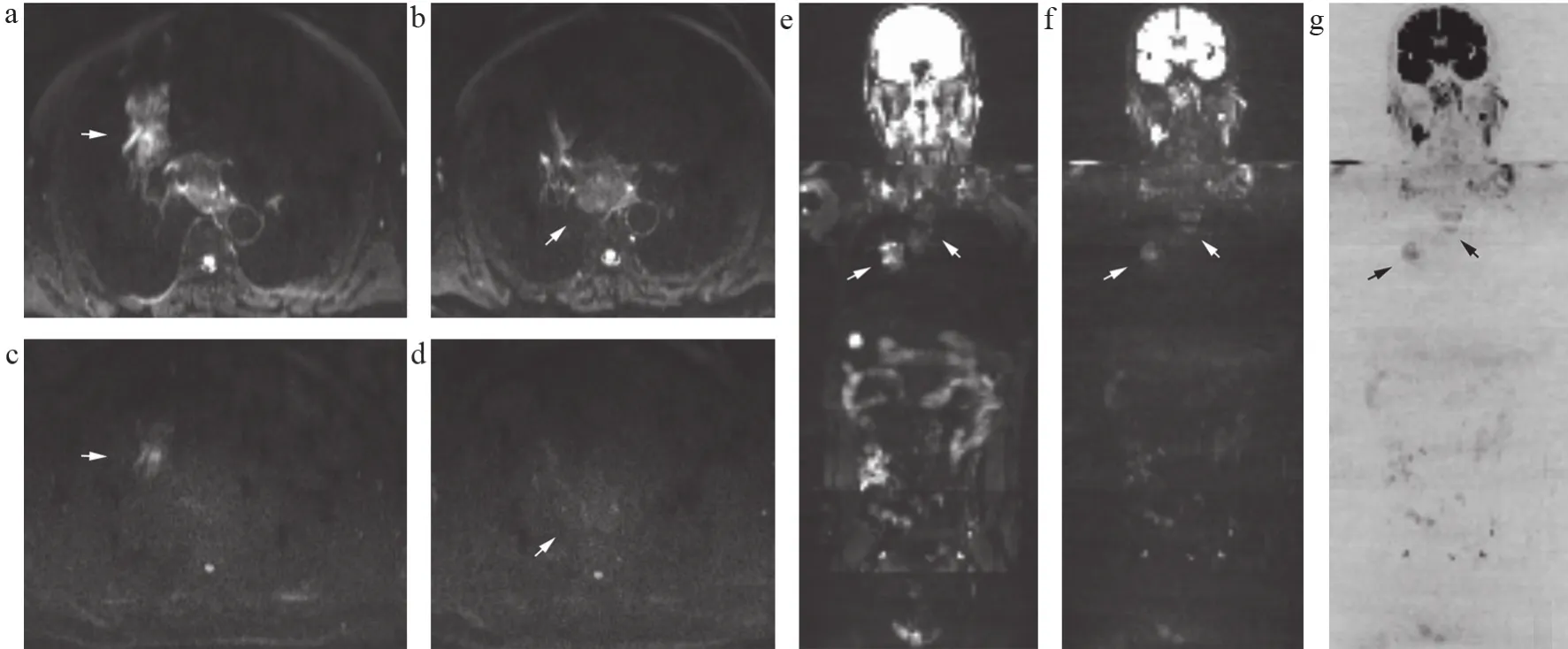
图1 PET-CT+颅脑MRI和WB-DWI的肺癌诊断图像

表1 经由PET-CT或WB-DWI的临床诊断淋巴结分期与淋巴结病理分期的关系(例)
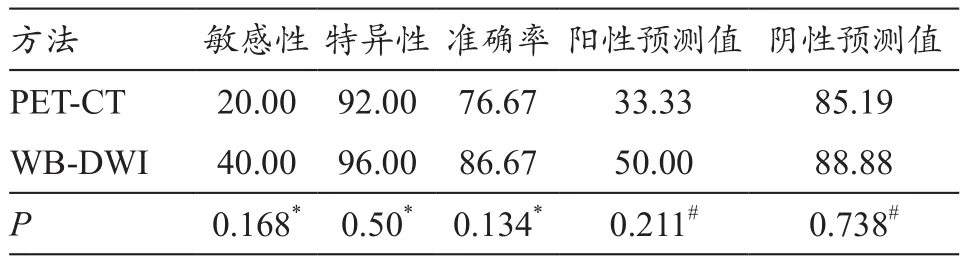
表2 肺癌的肺门及纵隔淋巴结在PET-CT或WB-DWI的诊断准确性评估(%)
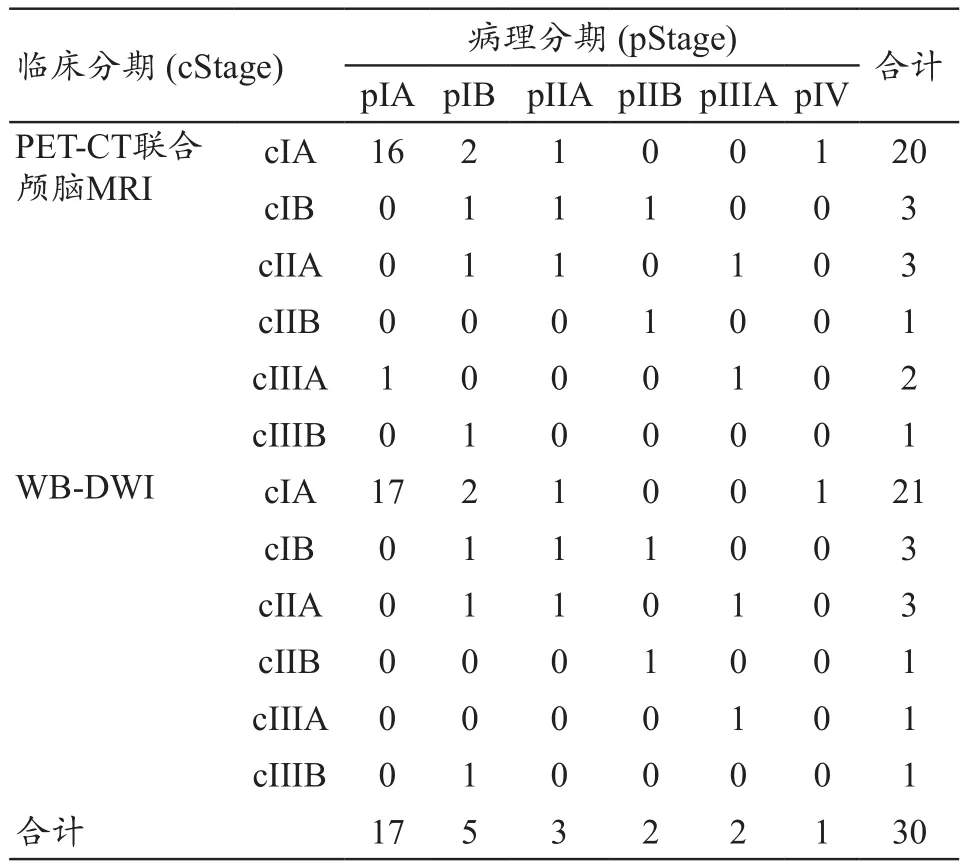
表3 经由PET-CT或WB-DWI诊断的临床分期与病理分期的关系(例)
3 讨论
本研究不仅使用了横断面轴位DWI扫描,且通过WB-DWI在冠状面重建中获得整体效果图,可显示除肿瘤病灶外的诸如血管瘤、肾囊肿、骨梗死等等良性病变。目前已有一些研究比较PET-CT扫描与WB-DWI诊断效能的优劣,指出WB-DWI在诊断脑转移和肝转移方面较PETCT要好[5],这是由于一些器官的高组织学FDG摄取掩盖了病灶的真实面目[6]。另一方面,WB-DWI在腹部和盆腔的影像诊断中,敏感性不如PET-CT[7]。因此,WB-DWI和PET-CT联合使用可以互补来提高诊断的性能。有研究指出,WB-DWI与PET-CT联合颅脑MRI能更加准确地论证肿瘤的临床分期[8],准确率接近98%。
研究发现WB-DWI对肺癌分期的诊断准确性高于PET-CT联合颅脑MRI(0.7>0.667),但两种检查方法没有统计学差异,因而可以认为两者的诊断性能相当。但由于PET-CT昂贵的价格,辐射损伤的影响,其普及率也不如MRI广泛,加上PET-CT对于脑转移的显示较差,必须用颅脑MRI作为辅助,因而可以认为WB-DWI具有更加便捷、直观且整体的统一性,检查方式优于PET-CT。同样我们在表1和表3中发现对于有淋巴结转移的患者,WB-DWI在诊断淋巴结转移方面高于PET-CT (表1中的WB-DWI 2例,PET-CT 0例),而对于有远处脑转移的患者差别不大(表3中两者均为3例),因而WB-DWI是一种有用的肺癌分期检查工具。
WB-DWI在显示远处转移性病变、恶性嗜铬细胞瘤和副神经节瘤等方面具有优势[9]。与PET-CT相比,WBDWI在卵巢癌患者中显示特征性的原发肿瘤灶,潜在病灶及远处病灶精度较高[10]。而本研究显示WB-DWI却与PET-CT诊断性能相当,这是由于远处转移的病例数较少,故无法引证上述研究。但却能显示在淋巴结转移诊断中的优越性。这与其他研究中,WB-DWI在淋巴瘤和消化道肿瘤的诊断性能与PET-CT相当[11],结果是一致的。但也有一些研究显示,WB-DWI在淋巴瘤和乳腺癌的诊断性能不如PET-CT[12]。因而,目前来说还没有统一的结论,需要进一步扩大样本量进行细致分组研究。
虽然PET-CT是作为肿瘤分期的首选影像学检查方法,但由于尘肺、矽肺、肺结核、结节病等病变,会对肺门和纵隔淋巴结的诊断产生假阳性结果,故对多个肺门和纵隔淋巴结FDG积聚的肺癌患者进行WB-DWI评价,可区分淋巴结的良恶性[13]。PET-CT同样可造成假阴性结果,比如在高分化肺腺癌的分期诊断中,PET-CT在淋巴结炎时可能显示假阳性,而在假阴性结果中的淋巴结可能含有少量的癌细胞[14]。这一结果和本研究中淋巴结分期诊断的结果是一致的(WB-DWI诊断准确率为86.67%>PET-CT的76.67%,同样特异性、阳性预测值和阴性预测值均高于PET-CT,见表2)。这也能为临床运用WB-DWI评价肺癌的淋巴结转移提供依据。
近年来,DWI可在动物模型的恶性转移淋巴结中区分炎症组织[15-16]。这使WB-DWI在评估肺结节和肿块方面比PET-CT更具有优势。WB-DWI中ADC值和信号强度可以区分良性和恶性纵隔淋巴结肿大,较PET-CT检查更具有数据说服力。因此,WB-DWI可成为肺癌分期评估的更有用的检查工具,其诊断性能优于PET-CT。
[1] Cossetti RJ,Bezerra RO,Gumz B,et al.Whole body diffusion for metastatic disease assessment in neuroendocrine carcinomas:comparison with OctreoScan® in two cases[J].World J Surg Oncol,2012,10:82.
[2] Ohno Y,Koyama H,Onishi Y,et al.Non-small cell lung cancer:whole-body MR examination for M-stage assessment utility for whole-body diffusion-weighted imaging compared with integrated FDG PET/CT[J].Radiology,2008,248(2):643-654.
[3] Heusch P,Köhler J,Wittsack HJ,et al.Hybrid [18F]-FDG PET/MRI including non-Gaussian diffusion-weighted imaging(DWI): preliminary results in non-small cell lung cancer(NSCLC)[J].Eur J Radiol,2013,82(11):2055-2060.
[4] Asamura H,Chansky K,Crowley J,et al.The international Association for the Study of Lung Cancer Lung Cancer Staging Project: proposals for the revision of the N descriptors in the forthcoming 8thedition of the TNM classification for lung cancer[J].J Thorac Oncol,2015,10(12):1675-1684.
[5] Kim HS,Lee KS,Ohno Y,et al.PET/CT versus MRI for diagnosis, staging, and follow-up of lung cancer[J].J Magn Reson Imaging,2015,42(2):247-260.
[6] Schmidt GP,Kramer H,Reiser MF,et al.Whole-body MRI and FDG-PET/CT imaging diagnostics in oncology[J].Radiologe,2010,50(4):329-338.
[7] Stecco A,Romano G,Negru M,et al.Whole-body diffusion weighted magnetic resonance imaging in the staging of oncological patients: comparison with positron emission tomography computed tomography (PET-CT) in a pilot study[J].Radiol Med,2009,114(1):1-17.
[8] Plathow C,Aschoff P,Lichy MP,et al.Positron emission tomography/computed tomography and whole-body magnetic resonance imaging in staging of advanced nonsmall cell lung cancer-initial results[J].Invest Radiol,2008,43(5):290-297.
[9] Laurent V,Trausch G,Bruot O,et al.Comparative study of two whole-body imaging techniques in the case of melanoma metastases: advantages of multi-contrast MRI examination including a diffusion-weighted sequence in comparison with PET-CT[J].Eur J Radiol,2010,75(3):376-383.
[10] Michielsen K,Vergote I,Beeck K,et al.Whole-body MRI with diffusion-weighted sequence for staging of patients with suspected ovarian cancer: a clinical feasibility study in comparison to CT and FDG-PET/CT[J].Eur Radiol,2014,24(4):889-901.
[11] Li B,Li Q,Nie W,et al.Diagnostic value of whole-body diffusion-weighted magnetic resonance imaging for detection of primary and metastatic malignancies: a meta analysis[J].Eur J Radiol,2014,83(2):338-344.
[12] Heusner TA,Kuemmel S,Koeninger A,et al.Diagnostic value of diffusion-weighted magnetic resonance imaging (DWI)compared to FDG PET/CT for whole-body breast cancer staging[J].Eur J Nucl Med Mol Imaging,2010,37(6):1077-1086.[13] Maturu VN,Agarwal R,Aggarwal AN,et al.Dual-time point whole-body18F-fluorodeoxyglucose PET/CT imaging in undiagnosed mediastinal lymphadenopathy: a prospective study of 117 patients with sarcoidosis and TB[J].Chest,2014,146(6):216-220.
[14] Usuda K,Zhao XT,Sagawa M,et al.Diffusion-weighted imaging is superior to PET in the detection and nodal assessment of lung cancers[J].Ann Thorac Surg,2011,91(6):1689-1695.
[15] Xue HD,Li S,Sun HY,et al.Experimental study of in fl ammatory and metastatic lymph nodes with diffusion weighted imaging on animal model: comparison with conventional methods[J].Chin Med Sci J,2008,23(3):166-171.
[16] Usuda K,Maeda S,Motono N,et al.Diagnostic performance of diffusion-weighted imaging for multiple hilar and mediastinal lymph nodes with FDG accumulation[J].Asian Pac J Cancer Prev,2015,16(15):6401-6406.
Comparative Study of Whole Body Diffusion Weighted Imaging with PET-CT and Craniocerebral MRI in the Clinical Diagnosis of Lung Cancer Staging
TAN Yanhuan, LI Junchen
Department of Radiology, Changshu Affiliated Hospital of Nanjing University of Chinese Medicine, Changshu Jiangsu 215500, China
ObjectiveTo determine whether the diagnostic performance of lung cancer staging by WB-DWI is superior to that of PETCT in combination with craniocerebral MRI.MethodsPET-CT in combination with craniocerebral MRI as well as WB-DWI were used for lung cancer patients before surgery. Among them, 22 were squamous cell carcinomas, 6 were adenocarcinomas and 2 were small cell lung cancer. The accuracy of lung cancer staging was analyzed by McNemar test and chi-square test.ResultsA total of 23 patients (76.67%) with pathological stage of N were correctly identified by PET-CT, with an estimated accuracy of 0.767. However, 2(6.67%) were over staged and 5 (16.67%) were under staged. 26 patients (86.67%) with pathological stage of N were correctly identified by WB-DWI, with an estimated accuracy of 0.867. However, 1 (3.33%) was over staged, and 3 (10%) were under staged. There was no statistical difference between the two detection rates. There were 20 (66.67%) cases who could correctly determine the pathological stage with PET-CT and brain MRI, and there were 3 (10%) over staging cases and 7 (23.33%) under staging cases, and the accuracy of staging was 0.667. There were 21 patients (70%) who could correctly be identified the pathological stage with WB-DWI, and there were 2 (6.67%) over staging cases and 7 (23.33%) cases were underestimated, the staging accuracy was 0.7. There was no statistical difference between the two detection rates.ConclusionWB-DWI is superior in staging diagnosis of lung cancer than PET-CT and brain MRI.
magnetic resonance imaging; positron emission tomography; diffusion weighted imaging; lung cancer; staging
R445.2;R814.42
B
10.3969/j.issn.1674-1633.2017.12.020
1674-1633(2017)012-0083-04
2017-07-01
李俊晨,副主任医师,主要研究方向为放射性脑损伤。
通讯作者邮箱:931903221@qq.com
本文编辑 王静
