腹腔镜前侧切除术治疗直肠癌的临床疗效
2017-12-20刘一萍杨萍黎笑欢张奎林周文明阳飞良任海波
刘一萍,杨萍,黎笑欢,张奎林,周文明,阳飞良,任海波
腹腔镜前侧切除术治疗直肠癌的临床疗效
刘一萍,杨萍,黎笑欢,张奎林,周文明,阳飞良,任海波
(江西省萍乡市第二人民医院普外科,江西 萍乡 337000)
目的 探究腹腔镜前侧切除术治疗直肠癌的临床疗效。方法 将76例直肠癌患者根据处理方式不同分对照组、腹腔镜组,各38例。对照组采用传统的开腹直肠癌切除手术治疗;腹腔镜组则用腹腔镜前侧切除术治疗。比较两组患者直肠癌治疗效果;术后排气时间、术中出血量、术后镇痛次数、住院时间;吻合口瘘、腹腔粘连等并发症发生率;手术前后SF-36生活质量评分。结果 腹腔镜组患者直肠癌治疗效果100.00%比对照组76.32%高,差异有统计学意义(P<0.05);腹腔镜组术后排气时间、术中出血量、术后镇痛次数、住院时间(2.01±0.32)d、(230.24±37.13)mL、(1.71±0.13)次、(6.21±0.55)d比对照组(3.72±1.91)d、(385.24±56.13)mL、(2.62±1.82)次、(8.13±1.66)d好,差异有统计学意义(P<0.05);腹腔镜组吻合口瘘、腹腔粘连等并发症发生率2.27%比对照组23.68%低,差异有统计学意义(P<0.05)。在术前两组患者SF-36生活质量评分比较差异无统计学意义;术后腹腔镜组患者SF-36生活质量评分显著高于对照组,差异有统计学意义(P<0.05)。结论 腹腔镜前侧切除术治疗直肠癌的临床疗效确切,可有效改善患者病情,减少创伤,缩短术后胃肠功能恢复时间,减轻术后疼痛,减少并发症,改善患者生活质量,值得推广。
腹腔镜前侧切除术;直肠癌;临床疗效;生活质量;并发症
直肠癌为常见消化系统恶性肿瘤,传统开腹手术治疗效果欠佳,创伤大,并发症多,而腹腔镜前侧切除术治疗具有微创性、无瘢痕、并发症少等优势,但手术难度也相对较高,在操作时需注意细节和无菌操作,以提高手术安全性[1]。本文将76例直肠癌患者根据处理方式不同分对照组、腹腔镜组,探讨了腹腔镜前侧切除术治疗直肠癌的临床疗效,报道如下。
1 资料与方法
1.1 临床资料 将本院2016年1月~2017年1月76例直肠癌患者根据处理方式不同分对照组、腹腔镜组,各38例。对照组男28例、女10例,年龄43~75岁,平均(48.73±5.01)岁。低分化3例,中分化20例,高分化15例。腹腔镜组男29例、女9例,年龄41~75岁,平均(48.92±5.24)岁。低分化3例,中分化19例,高分化16例。两组患者临床资料比较差异无统计学意义,具有可比性。
1.2 方法 对照组采用传统的开腹直肠癌切除手术治疗,实施静吸复合全麻,取截石位,左下腹旁正中切口,先对腹腔进行探查,观察有无肿瘤转移。分离血管,对淋巴结进行清扫,对直肠背侧进行锐性游离直至盆底,在距离肿瘤远端5 cm下将直肠切断,并用聚乙烯吡咯烷酮消毒,将乙状结肠端切断,乙状结肠远端和直肠上段吻合。
腹腔镜组则用腹腔镜前侧切除术治疗。实施静吸复合全麻,取截石位,脐部置入10 mm观察孔,将腹腔镜置入进行探查。根据患者情况设置穿刺孔,以置入超声刀和抓钳、吸引器等,腹腔镜下探查腹腔,并用纱布带进行乙状结肠结扎和牵引。用超声刀进行直肠系膜游离并处理细小血管,将大血管夹闭和切断。在肿瘤下2 cm用直线切割器将直肠下段切断,从左下腹穿刺孔将游离和切断后的直肠组织经无菌袋取出,用传统方法在体外切除,将乙状结肠切断,吻合器头端在近端结肠部位,用固定荷包放回腹腔,并给予体内吻合。术后给予常规抗感染治疗[2-3]。
1.3 观察指标 比较两组患者直肠癌治疗效果;术后排气时间、术中出血量、术后镇痛次数、住院时间;吻合口瘘、腹腔粘连等并发症发生率;手术前后SF-36生活质量评分。
其中,SF-36生活质量评分以100分为满分,分数越高则说明生活质量越高。显效:病灶切除,手术成功,术后无出现并发症;有效:症状改善,术后并发症轻微;无效:未达到上述标准。总有效率=显效率+有效率[4]。
1.4 统计学方法 本研究数据均使用SPSS 18.0软件统计处理,计量资料采用“x±s”表示,组间比较采用t检验;计数资料用例数(n)表示,组间率(%)的比较采用χ2检验。P<0.05为差异有统计学意义。
2 结果
2.1 直肠癌治疗效果比较 腹腔镜组患者直肠癌治疗效果100.00%比对照组76.32%高,差异有统计学意义(P<0.05),见表1。
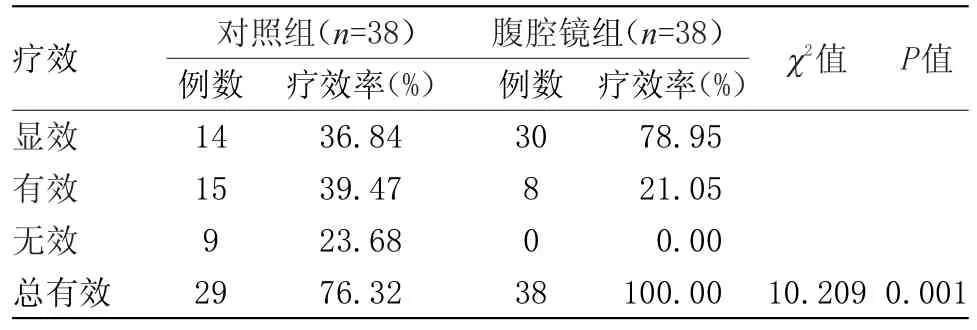
表1 两组患者直肠癌治疗效果比较(n)Table 1 Comparison of the two groups of patients with rectal cancer treatment number of cases(n)
2.2 术后排气时间、术中出血量、术后镇痛次数、住院时间比较 腹腔镜组术后排气时间、术中出血量、术后镇痛次数、住院时间均比对照组好,差异具有统计学意义(P<0.05),见表2。

表2 术后排气时间、术中出血量、术后镇痛次数、住院时间比较(x±s)Table 2 Postoperative exhaust time,intraoperative blood loss,postoperative analgesia,hospitalization time(x±s)
2.3 吻合口瘘、腹腔粘连等并发症发生率比较 腹腔镜组吻合口瘘、腹腔粘连等并发症发生率比对照组低,差异有统计学意义(P<0.05),见表3。

表3 两组患者吻合口瘘、腹腔粘连等并发症发生率比较(n)Table 3 Two groups of patients with anastomotic fistula,abdominal adhesions and other complications of the incidence(n)
2.4 干预前后SF-36生活质量评分 干预前SF-36生活质量评分相似,差异无统计学意义。干预后腹腔镜组SF-36生活质量评分优于对照组,差异具有统计学意义(P<0.05),见表4。
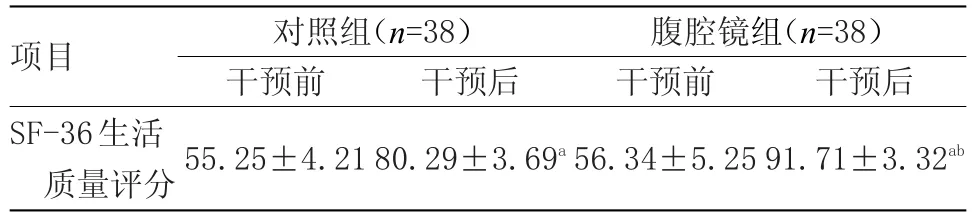
表4 干预前后SF-36生活质量评分比较(x±s)Table 4 Comparison of SF-36 quality of life before and after intervention(x±s)
3 讨论
直肠癌是临床常见恶性肿瘤,近年来随着饮食结构改变和人口老龄化逐渐严峻,直肠癌发病率逐年升高,因其解剖关系复杂,手术治疗若不彻底,容易出现复发,因此在对直肠癌进行手术治疗时需遵循彻底切除肿瘤,快速恢复肛门排气功能,以确保患者生活质量。传统多采用开腹手术进行治疗,但手术切口比较大,可给患者带来较大的创伤,术后并发症多。另外,传统开腹手术淋巴清扫不彻底,可导致复发,造成患者生活质量下降[5-6]。
腹腔镜前侧切除术治疗直肠癌效果较好,创伤小,出血少,术后并发症少,恢复较快。但需注意的是,腹腔镜前侧切除术后也容易出现吻合口出血、切口感染等并发症,因此在手术中需注意保持视野清晰,在切口吻合器头座放置的时候需根据肠壁厚度合理调整,避免切割肠壁。为预防吻合口出血发生,需注意拧紧吻合,确保设备完善,及时检查吻合后是否发生出血等并发症[7-8]。
和传统的开腹直肠癌切除手术比较,腹腔镜前侧切除术治疗难度显著降低,可减少腹腔污染发生率,容易推广应用[9]。另外,腹壁几乎不遗留手术瘢痕,可提高腹壁美容效果,但在操作过程需注意严格执行无菌操作,并彻底冲洗,预防术后感染和复发[10]。
本研究中,对照组采用传统的开腹直肠癌切除手术治疗;腹腔镜组则用腹腔镜前侧切除术治疗。结果显示,腹腔镜组患者直肠癌治疗效果比对照组高,差异有统计学意义(P<0.05);腹腔镜组术后排气时间、术中出血量、术后镇痛次数、住院时间比对照组好,差异有统计学意义(P<0.05);腹腔镜组吻合口瘘、腹腔粘连等并发症发生率比对照组低,差异有统计学意义(P<0.05)。在术前两组患者SF-36生活质量评分比较差异无统计学意义;术后腹腔镜组患者SF-36生活质量评分显著高于对照组,差异有统计学意义(P<0.05)。
综上所述,腹腔镜前侧切除术治疗直肠癌的临床疗效确切,可有效改善患者病情,减少创伤,缩短术后胃肠功能恢复时间,减轻术后疼痛,减少并发症,改善患者生活质量,值得推广。
[1] 王立强.腹腔镜下直肠癌前恻切除术治疗直肠癌的效果观察[J].中国保健营养,2017,27(9):154.
[2] 王峰,邱涛,龚旭晨,等.完全腹腔镜前侧切除术治疗直肠癌51例临床分析[J].中华腔镜外科杂志(电子版),2016,9(1):41-43.
[3] Maggiulli E,Fiorino C,Passoni P,et al.Characterisation of rectal motion during neo-adjuvant radiochemotherapy for rectal cancer with image-guided tomotherapy: Implicationsforadaptivedoseescalation strategies[J].Acta Oncologica,2012,51(3):318-324.
[4] 蔡文.腹腔镜前侧切除术与开腹术治疗直肠癌的疗效比较[J].临床检验杂志(电子版),2016,5(1):19-21.
[5] Attenberger UI,Pilz LR,Morelli JN,et al.MultiparametricMRIofrectalcancer-Doquantitative functional MR measurements correlate with radiologic and pathologic tumor stages?[J].European Journal of Radiology,2014,83(7):1036-1043.
[6] 张逖,张建都,王泰岳,等.腹腔镜下直肠癌前侧切除术治疗直肠癌156例疗效观察[J].山东医药,2013,53(23):81-82.
[7] Lee NK,Kim CY,Park YJ,et al.Clinical implication of negative conversion of predicted circumferential resection margin status after preoperative chemoradiotherapy forlocally advanced rectalcancer[J].European Journal of Radiology,2014,83(2):245-249.
[8] 罗慧,潘燕.腹腔镜下老年直肠癌切除术患者的手术室护理效果评价[J].当代医学,2016,22(29):102.
[9] Kotti A,Holmqvist A,Albertsson M,et al.SPARCL1 expression increases with preoperative radiation therapy and predicts better survival in rectal cancer patients[J].International Journal of Radiation Oncology,Biology,Physics,2014,88(5):1196-1202.
[10]Myerson RJ,Tan B,Hunt S,et al.Five fractions of radiationtherapyfollowedby4cyclesofFOLFOX chemotherapy as preoperative treatment for rectal cancer[J].International Journal of Radiation Oncology,Biology,Physics,2014,88(4):829-836.
Clinical efficacy of laparoscopic anterior resection for rectal cancer
Liu Yi-ping,Yang Ping,Li Xiao-huan,Zhang Kui-lin,Zhou Wen-ming,Yang Fei-liang,Ren Hai-bo
(Pingxiang City,Jiangxi Province Second People's Hospital General Surgery,Pingxiang,Jiangxi,337000,China)
Objective To investigate the clinical efficacy of laparoscopic anterior resection in the treatment of rectal cancer.Methods 76 cases of rectal cancer patients who were divided into three groups according to the treatment group,the laparoscopic group and the 38 cases.The control group was treated with traditional open rectal cancer resection.The laparoscopic group was treated with laparoscopic anterior resection.The number of postoperative ventilation,postoperative analgesia,postoperative analgesia,postoperative analgesia,postoperative analgesia,postoperative analgesia,postoperative analgesia,postoperative analgesia Fistula,abdominal adhesions and other complications;before and after surgery SF-36 quality of life score.Results The treatment effect of rectal cancer in laparoscopic group was 100.00%higher than that in control group(76.32%),the difference was statistically significant(P<0.05).The effect of laparoscopic group was higher than that of the control group.The difference between the two groups was statistically significant(P<0.05).The postoperative ventilation time,intraoperative blood loss,postoperative analgesia,(2.01±0.32)d,(230.24±37.13)mL,(1.71±0.13)times,(6.21±0.55)d,the control group was(3.72±1.91)d,(385.24±56.13)mL,(2.62±1.82)times and(8.13±1.66)d,the difference was statistically significant(P<0.05);laparoscopic group anastomotic fistula,intraperitoneal adhesions,and the number of postoperative analgesia and postoperative analgesia were significantly higher in the laparoscopic group than in the control group.The incidence of complications was 2.27%lower than that of the control group,the difference was statistically significant(P<0.05).There was no significant difference in SF-36 quality of life between the two groups before and after operation.There was no significant difference between the two groups.The quality of life of SF-36 in laparoscopic group was significantly higher than that in control group(P<0.05).Conclusion Laparoscopic anterior resection of rectal cancer is effective in the treatment of rectal cancer,which can effectively improve the condition of the patients,reduce the trauma,shorten the recovery time of postoperative gastrointestinal function,reduce the postoperative pain,reduce the complications and improve the quality of life of patients.
Laparoscopic anterior resection;Rectal cancer;Clinical efficacy;Quality of life;Complication
10.3969/j.issn.1009-4393.2017.36.011