Neurotrophic factors and corneal nerve regeneration
2017-09-04MartaSacchettiAlessandroLambiase
Marta Sacchetti, Alessandro Lambiase
Department of Sense Organs, Sapienza University of Rome, Rome, Italy
Neurotrophic factors and corneal nerve regeneration
Marta Sacchetti, Alessandro Lambiase*
Department of Sense Organs, Sapienza University of Rome, Rome, Italy
How to cite this article:Sacchetti M, Lambiase A (2017) Neurotrophic factors and corneal nerve regeneration. Neural Regen Res 12(8):1220-1224.
neurotrophic keratitis; corneal sensitivity; nerve regeneration; nerve growth factor
Introduction
Several local and systemic conditions that affect the cornea such as diabetes, dry eye, herpes simplex keratitis and neurotrophic keratitis, are associated with impairment of corneal innervation leading to decrease in tear production and impairment of wound healing (Sacchetti and Lambiase, 2014; Mastropasqua et al., 2017). The cornea is characterized by peculiar properties that make it a unique tissue to be used as a model for regenerative medicine studies, in fact, the cornea can be directly visualized and corneal structures, including nerves may be easily evaluated for both function and morphology using standard instruments such as slit lamp andin vivoconfocal microscopy (IVCM) (Cruzat et al., 2016). Recently, the cornea model has been successfully used in phase I/II clinical trials to obtain regulatory approval for cell therapy in limbal stem cell def i ciency, a rare corneal disease, orphan of medical treatment. In fact, the possibility of a direct visualization of corneal structures, including the epithelium, associated with well standardized clinical safety and ef ficacy outcomes, allowed scholars to demonstrate the regenerative effects of epithelial stem cell transplantation (Rama et al., 2017).e cornea represents also a useful model to characterize neuroregeneration and to evaluate novel neuroregenerative therapeutic approaches in humans.
Instruments for the assessment of corneal sensitivity have been developed and some of them are available for clinical use. Among them, the most used is the Cochet-Bonnet aesthesiometer, that allows scholars to easily evaluate mechanical corneal sensitivity. More recently, other clinical devices able to assess more specific sensitivity patterns, including chemical, thermal and mechanical corneal sensitivity, such as the Belmonte’s no-contact esthesiometer, have been introduced for clinical and research purposes (Belmonte et al., 2004; Golebiowski et al., 2011).
In addition, morphology of corneal nerves can be easily evaluated and visualized by IVCM, that is a rapid and non-invasive imaging method (Cruzat et al., 2017).In vivoconfocal microscopy allows scholars to visualize corneal nerves in health and in several ocular and systemic pathologic conditions and to assess their morphology in terms of nerve density and length, nerve branching, ref l ectivity and tortuosity (Lambiase et al., 2013; Cruzat et al., 2017) (Figure 1). This technique has also been used to assess peripheral neuropathy in patients with diabetes, idiopathic small fibre neuropathy, Charcot-Marie-Tooth Neuropathy Type 1 (CMT1A), Fabry’s disease and paraneoplastic neurological syndromes (Cruzat et al., 2017). In addition, IVCM is used to evaluatein vivothe ef f ects of treatments on corneal nerveregeneration and to evaluate recovery of corneal innervation during pathological conditions or aer surgery (Tavakoli et al., 2013; Cruzat et al., 2017; Culver et al., 2017; Lewis et al., 2017).
Recently, a neurofluorescent mouse model has been developed to study nerve regenerationin vivo. Specif i cally, thethy1-YFP transgenic mouse allowsin vivovisualization of fl uorescent sensory nerves and axonal regeneration and degeneration can be visualized and quantif i edin vivoallowing the possibility to investigate the neurotrophic potential of molecules and drugs (Yu and Rosenblatt, 2007; Leckelt et al., 2016).
Corneal Innervation Morphology and Function
Corneal innervation is provided by trigeminal nerve bundles that lose their perineurium and myelin sheaths and penetrate into the corneal stroma at the corneoscleral limbus, branching into the stromal plexus and then into the subepithelial and subbasal nerve plexus that provide sensitivity to the corneal epithelium (Muller et al., 2003). Corneal primary afferent neurons are represented by polymodal receptors that respond to mechanical, thermal and chemical stimuli, mechanoreceptors activated by mechanical stimuli, and cold receptors that respond to corneal cooling (Muller et al., 2003). Corneal sensory nerves react to ocular surface damage by inducing symptoms of pain and irritation and by eliciting protective reflexes such as blinking and tearing. In addition, corneal nerves provide trophic support to the ocular surface tissues, stimulate wound healing and maintain anatomic integrity by releasing neuromediators and growth factors (Muller et al., 2003; Shaheen et al., 2014; Mastropasqua et al., 2017).
Production and release of neuromediators during neurodegenerative diseases of the ocular surface can be easily evaluated by non-invasive, simple techniques such as corneal and conjunctival impression cytology and tear sample collection, that allow scholars to perform biochemical and molecular evaluation (Tervo et al., 1995; Yamada et al., 2000; Lambiase et al., 2011; Sacchetti et al., 2011; Mantelli et al., 2015). Several studies using these techniques have extended results on pathogenic mechanisms and drug effects from animal models to human ocular conditions (Lee et al., 2006; Lee and Kim, 2015).
Clinical Evidence of Corneal Neuroregeneration
Total or partial loss of corneal innervation leads to the development of neurotrophic keratitis (NK).is is a rare, degenerative corneal disease characterized by corneal epithelium breakdown with scarce tendency to healing and development of epithelial defects that may progress to corneal ulcer, melting and eye perforation (Mastropasqua et al., 2017). Several ocular and systemic diseases can damage the fifth cranial nerve at various levels, from the trigeminal nucleus to the corneal nerve endings. The most common causes of NK are herpetic viral keratitis, followed by trigeminal ophthalmic branch damage due to intracranial neoplasia and/ or neurosurgical procedures. Other ocular causes of corneal nerve damage include chemical burns, physical injuries, ocular surgery, corneal dystrophies, and chronic topical medications use. Systemic diseases, such as diabetes, multiple sclerosis, congenital syndromes, neurotoxic therapies and leprosy, can also impair corneal sensitivity, leading to NK (Sacchetti and Lambiase, 2014; Hsu and Modi, 2015).
Patients with NK, having a decrease of ocular surface sensitivity, rarely complain symptoms of ocular surface discomfort, while they may refer impaired vision in most severe cases (Sacchetti and Lambiase, 2014).e lack of symptoms in NK patients should be considered in the management of patients with local or systemic conditions causing trigeminal damage, and these patients should be routinely evaluated by an ophthalmologist to identify signs of corneal involvement (Sacchetti and Lambiase, 2014). NK is classif i ed based on the severity of the corneal damage in 3 stages. Stage 1 is characterized by a cloudy appearance of the epithelium associated or not with corneal and conjunctival epithelial damage. Stage 2 is characterized by the presence of a persistent epithelialdefect that may progress to corneal ulcer, perforation and/or stromal melting in stage 3.
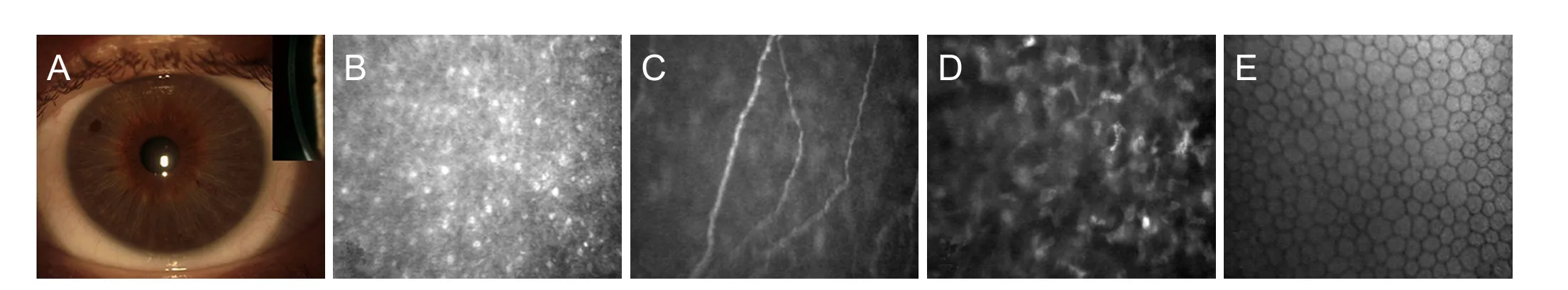
Figure 1 A cornea of a healthy eye observed by slit lamp exam with frontal and longitudinal (insert) view.
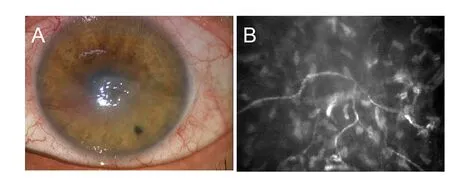
Figure 2 Neurotrophic corneal ulcer (A) associated with impaired corneal innervation as demonstrated by decreased nerve density and increased tortuosity (B) atin vivoconfocal microscopy imaging.
Diagnosis of NK requires a careful clinical history collection to identify risk factors for trigeminal impairment and a multidisciplinary approach including ophthalmologist, neurologist and neuro-radiologist.e ophthalmologist will perform a complete eye examination with the slit lamp to identify corneal and conjunctival signs of NK and to classify NK severity. The diagnosis of NK is confirmed by the presence of decreased corneal sensitivity. Corneal sensitivity can be qualitatively detected by touching the cornea with the tip of a cotton swab, while severity of corneal sensitivity impairment may be quantified by a corneal aesthesiometer (Sacchetti and Lambiase, 2014). The Cochet-Bonnet aesthesiometer, the most frequently used, assesses corneal sensitivity by touching the cornea with a nylon fi lament: the length of the fi lament required to induce a blink reaction or a patient response will quantify the corneal mechanical sensitivity threshold (Sacchetti and Lambiase, 2014).
Corneal nerve imaging by IVCM may also allow thein vivoevaluation of all corneal structures including epithelium, nerves, keratocytes and endothelium (Lambiase et al., 2013). In fact, an IVCM study demonstrated that all corneal structures showed changes in patients with impairment of corneal sensitivity supporting the evidence of the key role of corneal nerves in maintaining homeostasis, survival, metabolism, and renewal of corneal cells (Lambiase et al., 2013) (Figure 2).
Management of NK is a challenge for ophthalmologists because of the lack of specific treatments able to stimulate corneal nerve regeneration and to restore corneal nerve function. Actually, NK treatment options aim at improving corneal healing and preventing progression of corneal damage and treatments able to stimulate corneal nerve regeneration are highly sought-aer (Sacchetti and Lambiase, 2014; Mastropasqua et al., 2017). Currently, the use of preservative-free ocular lubricants is a fi rst-line therapy and can be associated with the use of therapeutic contact lens (Lambiase et al., 1999; Sacchetti and Lambiase, 2014). Recently, a new regenerating agent, Cacicol (Laboratoires Théa, France), has been proposed as therapeutic option for treatment of persistent epithelial defects (Aifa et al., 2012; Arvola et al., 2016).e results of a fi rst open-label study evaluating the ef f ects of Cacicol in 11 patients with refractory NK reported a complete corneal healing in 73% of cases (Aifa et al., 2012). These data were not confirmed in a second study that described a complete corneal healing in only 33% of 6 patients aer 6–10 weeks of treatment (Arvola et al., 2016). Currently, unresponsive cases of NK require a surgical approach such as tarsorraphy, amniotic membrane transplantation, or conjunctival fl ap.ese approaches are ef f ective in achieving corneal healing, however, they result in poor cosmetic outcome and impairment of visual function (Chen et al., 2000; Hick et al., 2005; Khokhar et al., 2005; Turkoglu et al., 2014; Rajak et al., 2015; Uhlig et al., 2015; Ilic et al., 2016).
In the last decades, novel therapeutic approaches aiming at stimulating epithelial healing and/or corneal nerve regeneration and at restoring corneal nerve function and sensitivity have been proposed. Among them, several studies reported an high success rate in patients with NK treated with autologous serum eye drops, topical non-gelified platelet-rich plasma (PRP) eye drops, and umbilical cord serum eye drops. All these agents provide growth factors, neuromediators, and nutrients to the ocular surface and different studies reported corneal healing in 70% to 97% of cases (Lugo and Arentsen, 1987; Alino et al., 1998; Jeng and Dupps, 2009; Geremicca et al., 2010; Guadilla et al., 2013; Giannaccare et al., 2015; Sanchez-Avila et al., 2017). Based on these encouraging results two randomized clinical trials (RCT) are ongoing to evaluate safety and ef fi cacy of topical plasma rich in growth factors and cord blood in patients with NK (NCT03084861, NCT02707120).
In the last decades, several growth factors and neuroptptides have been shown to exert a positive ef f ect on corneal regeneration, including nerve growth factor (NGF), epidermal growth factor (EGF), SP and insulin-like growth factor-1 (IGF-1), vascular endothelial growth factor (VEGF), sema-phorins, neurotrophins 3 and 4 (NT-3; NT-4), growth associated protein-43 (Daniele et al., 1992; Muller et al., 2003; Nishida et al., 2007; Yanai et al., 2015). Despite encouraging results showed by the dif f erent trophic factors in stimulating corneal healing in patients with NK, very few demonstrated the ef ficacy in restoring corneal sensitivity and nerve morphology as demonstrated byin vivoimaging.
Topical treatment with NGF also represents a promising strategy to induce a durable recovery of trigeminal nerve function. A fi rst open-label study evaluating the ef ficacy of NGF eye drops treatment in 12 patients with neurotrophic keratitis at stage 2 and 3 reported complete corneal healing in 100% of cases after 10 days to 6 weeks treatment associated with a recovery of corneal sensitivity in most of the patients (Lambiase et al., 1998). A subsequent open-label, non-comparative study confirmed the previous results showing a complete corneal healing in 45 out of 45 eyes with NK at stage 2 and 3 refractive to medical treatments within 6 weeks of treatment. In this study, patients also showed signif i cant improvement of corneal sensitivity, tear function and visual acuity (Bonini et al., 2000).
In addition, the potential ef f ect of NGF in inducing nerve regeneration has been clearly demonstrated in several human diseases, such as diabetic, traumatic and toxic neuropathy (Sacchetti and Lambiase, 2014). Recently, a novel recombinant human NGF has been developed and has successfully completed the clinical development phase and recently received marketing authorization in Europe (EU/1/17/1197) opening new prospective for its next clinical use for inducing corneal neuroregeneration (Ferrari et al., 2014).
An open study reported that treatment with oral nicergoline was ef f ective in reaching a complete corneal healing in 23 out of 27 eyes with NK and in improving corneal sensitivity.ese ef f ects were associated with a signif i cant increase in tear level of NGF (Lee and Kim, 2015).
Other neurotrophic factors are under investigation. Specifically, topical treatment with CNTF in mice with wounded corneas showed an increased nerve fi ber density 8 weeks aer wounding (Reichard et al., 2014).e administration of pigment epithelial-derived factor in association with docosahexaenoic acid aer experimental surgery in rabbits showed a 75% of recovery of corneal sensitivity after 7 weeks of treatment (He et al., 2015). Subconjunctival injection of neuropeptide FF in diabetic mice promoted corneal nerve injury recovery and epithelial wound healing (Dai et al., 2015).
Conclusions
The cornea represents a unique model to evaluate in vivo the morphology and function of sensory nerves, their role in maintaining tissue trophism, the crosstalk between nerves and cells and the ef f ect of neuroregenerative drugs.e “human model” of the corneal disease induced by sensory nerve impairment is called NK. In fact, all local and systemic conditions causing damage to the trigeminal nerve may decrease corneal sensitivity and lead to the development of NK that is characterized by the development of non-healing corneal defects associated with lack of ocular symptoms. A multidisciplinary approach to patients with NK will aid at early identifying patients with NK and at improving their clinical outcome.e management of NK is still a challenge, due to the lack of pathogenic treatments targeting nerve regeneration.e development of novel molecules stimulating corneal nerve regeneration will improve the clinical management and outcomes of this disease.
Author contributions:AL and MS substantially contributed to condecptuzlization, acquisition of data, writing the draand revising the article.
Conf l icts of interest:None declared.
Plagiarism check:Checked twice by ienticate.
Peer review:Externally peer reviewed.
Open access statement:
Open peer review reports:
Reviewer 1: Rayaz Ahmed Malik, Weill Cornell Medical College in Qatar, Qatar.
Reviewer 2: Steven Levy, MD Stem Cells, USA.
Comments to authors: This is an excellent review of the physiology of the corneal nerves and the etiologies and disease manifestations of Neurotrophic Keratitis (NK).e paper also provides a well researched review of the current and previously published interventions using various neurotrophic factors. Having additional information detailing the completed studies within the paper would be helpful.
Aifa A, Gueudry J, Portmann A, Delcampe A, Muraine M (2012) Topical treatment with a new matrix therapy agent (RGTA) for the treatment of corneal neurotrophic ulcers. Invest Ophthalmol Vis Sci 53:8181-8185.
Alino AM, Perry HD, Kanellopoulos AJ, Donnenfeld ED, Rahn EK (1998) Conjunctival fl aps. Ophthalmology 105:1120-1123.
Arvola RP, Robciuc A, Holopainen JM (2016) Matrix regeneration therapy: a case series of corneal neurotrophic ulcers. Cornea 35:451-455.
Belmonte C, Aracil A, Acosta MC, Luna C, Gallar J (2004) Nerves and sensations from the eye surface. Ocul Surf 2:248-253.
Bonini S, Lambiase A, Rama P, Caprioglio G, Aloe L (2000) Topical treatment with nerve growth factor for neurotrophic keratitis. Ophthalmology 107:1347-1351; discussion 1351-1342.
Chen HJ, Pires RT, Tseng SC (2000) Amniotic membrane transplantation for severe neurotrophic corneal ulcers. Br J Ophthalmol 84:826-833.
Cruzat A, Qazi Y, Hamrah P (2016) In vivo confocal microscopy of corneal nerves in health and disease. Ocul Surf 15:15-47.
Culver DA, Dahan A, Bajorunas D, Jeziorska M, van Velzen M, Aarts L, Tavee J, Tannemaat MR, Dunne AN, Kirk RI, Petropoulos IN, Cerami A, Malik RA, Brines M (2017) Cibinetide improves corneal nerve fi ber abundance in patients with sarcoidosis-associated small nerve fiber loss and neuropathic pain. Invest Ophthalmol Vis Sci 58:BIO52-BIO60.
Dai Y, Zhao X, Chen P, Yu Y, Wang Y, Xie L (2015) Neuropeptide FF promotes recovery of corneal nerve injury associated with hyperglycemia. Invest Ophthalmol Vis Sci 56:7754-7765.
Daniele S, Gilbard JP, Schepens CL (1992) Treatment of persistent epithelial defects in neurotrophic keratitis with epidermal growth factor: a preliminary open study. Graefes Arch Clin Exp Ophthalmol 230:314-317.
Dunn SP, Heidemann DG, Chow CY, Crockford D, Turjman N, Angel J, Allan CB, Sosne G (2010) Treatment of chronic nonhealing neurotrophic corneal epithelial defects with thymosin beta4. Ann N Y Acad Sci 1194:199-206.
Ferrari MP, Mantelli F, Sacchetti M, Antonangeli MI, Cattani F, D’Anniballe G, Sinigaglia F, Ruffini PA, Lambiase A (2014) Safety and pharmacokinetics of escalating doses of human recombinant nerve growth factor eye drops in a double-masked, randomized clinical trial. BioDrugs 28:275-283.
Geremicca W, Fonte C, Vecchio S (2010) Blood components for topical use in tissue regeneration: evaluation of corneal lesions treated with platelet lysate and considerations on repair mechanisms. Blood Transfus 8:107-112.
Giannaccare G, Fresina M, Vagge A, Versura P (2015) Synergistic ef f ect of regenerating agent plus cord blood serum eye drops for the treatment of resistant neurotrophic keratitis: a case report and a hypothesis for pathophysiologic mechanism. Int Med Case Rep J 8:277-281.
Golebiowski B, Papas E, Stapleton F (2011) Assessing the sensory function of the ocular surface: implications of use of a non-contact air jet aesthesiometer versus the Cochet-Bonnet aesthesiometer. Exp Eye Res 92:408-413.
Guadilla AM, Balado P, Baeza A, Merino M (2013) Ef f ectiveness of topical autologous serum treatment in neurotrophic keratopathy. Arch Soc Esp Oalmol 88:302-306.
He J, Cortina MS, Kakazu A, Bazan HE (2015)e PEDF neuroprotective domain plus DHA induces corneal nerve regeneration aer experimental surgery. Invest Ophthalmol Vis Sci 56:3505-3513.
Hick S, Demers PE, Brunette I, La C, Mabon M, Duchesne B (2005) Amniotic membrane transplantation and fi brin glue in the management of corneal ulcers and perforations: a review of 33 cases. Cornea 24:369-377.
Hsu HY, Modi D (2015) Etiologies, quantitative hypoesthesia, and clinical outcomes of neurotrophic keratopathy. Eye Contact Lens 41:314-317.
Ilic D, Vicovac L, Nikolic M, Lazic Ilic E (2016) Human amniotic membrane gras in therapy of chronic non-healing wounds. Br Med Bull 117:59-67.
Jeng BH, Dupps WJ, Jr. (2009) Autologous serum 50% eyedrops in the treatment of persistent corneal epithelial defects. Cornea 28:1104-1108.
Khokhar S, Natung T, Sony P, Sharma N, Agarwal N, Vajpayee RB (2005) Amniotic membrane transplantation in refractory neurotrophic corneal ulcers: a randomized, controlled clinical trial. Cornea 24:654-660.
Lambiase A, Rama P, Aloe L, Bonini S (1999) Management of neurotrophic keratopathy. Curr Opin Ophthalmol 10:270-276.
Lambiase A, Sacchetti M, Mastropasqua A, Bonini S (2013) Corneal changes in neurosurgically induced neurotrophic keratitis. JAMA Ophthalmol 131:1547-1553.
Lambiase A, Rama P, Bonini S, Caprioglio G, Aloe L (1998) Topical treatment with nerve growth factor for corneal neurotrophic ulcers. N Engl J Med 338:1174-1180.
Lambiase A, Micera A, Sacchetti M, Cortes M, Mantelli F, Bonini S (2011) Alterations of tear neuromediators in dry eye disease. Arch Ophthalmol 129:981-986.
Leckelt J, Guimaraes P, Kott A, Ruggeri A, Stachs O, Baltrusch S (2016) Early detection of diabetic neuropathy by investigating CNFL and IENFD in thy1-YFP mice. J Endocrinol 231:147-157.
Lee HK, Ryu IH, Seo KY, Hong S, Kim HC, Kim EK (2006) Topical 0.1% prednisolone lowers nerve growth factor expression in keratoconjunctivitis sicca patients. Ophthalmology 113:198-205.
Lee YC, Kim SY (2015) Treatment of neurotrophic keratopathy with nicergoline. Cornea 34:303-307.
Lewis EJH, Perkins BA, Lovblom LE, Bazinet RP, Wolever TMS, Bril V (2017) Ef f ect of omega-3 supplementation on neuropathy in type 1 diabetes: A 12-month pilot trial. Neurology 88:2294-2301.
Lugo M, Arentsen JJ (1987) Treatment of neurotrophic ulcers with conjunctival fl aps. Am J Ophthalmol 103:711-712.
Mantelli F, Lambiase A, Sacchetti M, Orlandi V, Rosa A, Casella P, Bonini S (2015) Cocaine snorting may induce ocular surface damage through corneal sensitivity impairment. Graefes Arch Clin Exp Ophthalmol 253:765-772.
Mastropasqua L, Massaro-Giordano G, Nubile M, Sacchetti M (2017) Understanding the pathogenesis of neurotrophic keratitis: the role of corneal nerves. J Cell Physiol 232:717-724.
Muller LJ, Marfurt CF, Kruse F, Tervo TM (2003) Corneal nerves: structure, contents and function. Exp Eye Res 76:521-542.
Nishida T, Chikama T, Morishige N, Yanai R, Yamada N, Saito J (2007) Persistent epithelial defects due to neurotrophic keratopathy treated with a substance p-derived peptide and insulin-like growth factor 1. Jpn J Ophthalmol 51:442-447.
Rajak S, Rajak J, Selva D (2015) Performing a tarsorrhaphy. Community Eye Health 28:10-11.
Rama P, Ferrari G, Pellegrini G (2017) Cultivated limbal epithelial transplantation. Curr Opin Ophthalmol 28:387-389.
Reichard M, Hovakimyan M, Guthof f RF, Stachs O (2014) In vivo visualisation of murine corneal nerve fi bre regeneration in response to ciliary neurotrophic factor. Exp Eye Res 120:20-27.
Sacchetti M, Lambiase A (2014) Diagnosis and management of neurotrophic keratitis. Clin Ophthalmol 8:571-579.
Sacchetti M, Micera A, Lambiase A, Speranza S, Mantelli F, Petrachi G, Bonini S, Bonini S (2011) Tear levels of neuropeptides increase aer specif i c allergen challenge in allergic conjunctivitis. Mol Vis 17:47-52.
Sanchez-Avila RM, Merayo-Lloves J, Riestra AC, Fernandez-Vega Cueto L, Anitua E, Begona L, Muruzabal F, Orive G (2017) Treatment of patients with neurotrophic keratitis stages 2 and 3 with plasma rich in growth factors (PRGF-Endoret) eye-drops. Int Ophthalmol doi:10.1007/s10792-017-0582-7.
Shaheen BS, Bakir M, Jain S (2014) Corneal nerves in health and disease. Surv Ophthalmol 59:263-285.
Tavakoli M, Mitu-Pretorian M, Petropoulos IN, Fadavi H, Asghar O, Alam U, Ponirakis G, Jeziorska M, Marshall A, Efron N, Boulton AJ, Augustine T, Malik RA (2013) Corneal confocal microscopy detects early nerve regeneration in diabetic neuropathy aer simultaneous pancreas and kidney transplantation. Diabetes 62:254-260.
Tervo TM, Mertaniemi P, Ylatupa S, Tervo K, Virtanen T, Partanen P (1995) Release of calcitonin gene-related peptide in tears aer excimer laser photorefractive keratectomy. J Refract Surg 11:126-128.
Turkoglu E, Celik E, Alagoz G (2014) A comparison of the ef fi cacy of autologous serum eye drops with amniotic membrane transplantation in neurotrophic keratitis. Semin Ophthalmol 29:119-126.
Uhlig CE, Frings C, Rohlof f N, Harmsen-Aasman C, Schmitz R, Kiesel L, Eter N, Busse H, Alex AF (2015) Long-term efficacy of glycerine-processed amniotic membrane transplantation in patients with corneal ulcer. Acta Ophthalmol 93:e481-487.
Yamada M, Ogata M, Kawai M, Mashima Y (2000) Decreased substance P concentrations in tears from patients with corneal hypesthesia. Am J Ophthalmol 129:671-672.
Yamada N, Matsuda R, Morishige N, Yanai R, Chikama TI, Nishida T, Ishimitsu T, Kamiya A (2008) Open clinical study of eye-drops containing tetrapeptides derived from substance P and insulin-like growth factor-1 for treatment of persistent corneal epithelial defects associated with neurotrophic keratopathy. Br J Ophthalmol 92:896-900.
Yanai R, Nishida T, Chikama T, Morishige N, Yamada N, Sonoda KH (2015) Potential new modes of treatment of neurotrophic keratopathy. Cornea 34 Suppl 11:S121-127.
Yu CQ, Rosenblatt MI (2007) Transgenic corneal neurof l uorescence in mice: a new model for in vivo investigation of nerve structure and regeneration. Invest Ophthalmol Vis Sci 48:1535-1542.
*< class="emphasis_italic">Correspondence to: Alessandro Lambiase, M.D., Ph.D., alessandro.lambiase@ uniroma1.it.
Alessandro Lambiase, M.D., Ph.D., alessandro.lambiase@ uniroma1.it.
orcid: 0000-0002-8974-991X (Alessandro Lambiase) 0000-0001-5569-778X (Marta Sacchetti)
10.4103/1673-5374.213534
Accepted: 2017-07-20
杂志排行
中国神经再生研究(英文版)的其它文章
- A progressive compression model of thoracic spinal cord injury in mice: function assessment and pathological changes in spinal cord
- A novel triple immunoenzyme staining enables simultaneous identif i cation of all muscle fi ber types on a single skeletal muscle cryosection from normal, denervated or reinnervated rats
- Optical coherence tomography and T cell gene expression analysis in patients with benign multiple sclerosis
- Impact of Pitx3 gene knockdown on glial cell linederived neurotrophic factor transcriptional activity in dopaminergic neurons
- Dried Rehmannia root protects against glutamateinduced cytotoxity to PC12 cells through energy metabolism-related pathways
- Dexmedetomidine mitigates isof l urane-induced neurodegeneration in fetal rats during the second trimester of pregnancy