血管外肺水指数及肺血管通透性指数对重症急性呼吸窘迫综合征患者预后的预测价值研究
2017-09-03易智婷王建春
易智婷,王建春
·论著·
血管外肺水指数及肺血管通透性指数对重症急性呼吸窘迫综合征患者预后的预测价值研究
易智婷1,王建春2
目的 探讨血管外肺水指数(EVLWI)及肺血管通透性指数(PVPI)对重症急性呼吸窘迫综合征(ARDS)患者预后的预测价值。方法 选取2014年3月—2016年3月湖北省鄂东医疗集团黄石市中心医院(湖北理工学院附属医院)收治的重症ARDS患者31例,根据预后分为存活组14例与死亡组17例。两组患者入院后均予以常规治疗,治疗期间监测患者生命体征。比较两组患者治疗前及治疗24 h、48 h、72 h EVLWI、PVPI、氧合指数,比较治疗72 h不同EVLWI或PVPI患者急性生理学与慢性健康状况评分系统Ⅱ(APACHEⅡ)评分、感染相关器官功能衰竭评分系统(SOFA)评分、氧合指数;EVLWI和PVPI与重症ARDS患者氧合指数的相关性分析采用Pearson相关性分析,采用四格表评估EVLWI和PVPI对重症ARDS患者预后的预测价值。结果 时间与方法在EVLWI、PVPI、氧合指数上无交互作用(P>0.05);时间在EVLWI、PVPI、氧合指数上主效应不显著(P>0.05);方法在EVLWI、PVPI、氧合指数上主效应显著(P<0.05);治疗48 h、72 h存活组患者EVLWI、PVPI低于死亡组,氧合指数高于死亡组(P<0.05)。Pearson相关性分析结果显示,EVLWI和PVPI与重症ARDS患者氧合指数呈负相关(r值分别为-0.772、-0.691,P<0.05)。治疗72 h,EVLWI≥10 ml/kg和PVPI≥3患者APACHEⅡ评分、SOFA评分分别高于EVLWI<10 ml/kg和PVPI<3患者,氧合指数分别低于EVLWI<10 ml/kg和PVPI<3患者(P<0.05)。以10 ml/kg为临界值,EVLWI预测重症ARDS患者预后的灵敏度为88.2%,特异度为100.0%,阳性预测值为100.0%,阴性预测值为87.5%,符合率为93.5%;以3为临界值,PVPI预测重症ARDS患者预后的灵敏度为76.5%,特异度为100.0%,阳性预测值为100.0%,阴性预测值为77.8%,符合率为87.1%。结论 EVLWI和PVPI与重症ARDS患者氧合指数呈负相关,二者对重症ARDS患者预后的预测价值均较高。
呼吸窘迫综合征,成人;血管外肺水指数;肺血管通透性指数;预后
易智婷,王建春.血管外肺水指数及肺血管通透性指数对重症急性呼吸窘迫综合征患者预后的预测价值研究[J].实用心脑肺血管病杂志,2017,25(7):36-40.[www.syxnf.net]
YI Z T,WANG J C.Predictive value of extravascular lung water index and pulmonary vascular permeability index on prognosis in patients with severe acute respiratory distress syndrome[J].Practical Journal of Cardiac Cerebral Pneumal and Vascular Disease,2017,25(7):36-40.
急性呼吸窘迫综合征(ARDS)是指由严重感染、休克、创伤、烧伤、脓毒血症等原因引起弥漫性肺损伤、肺泡萎陷、肺通气不足的以顽固性低氧血症、呼吸衰竭为主要特征的临床综合征,起病急骤,病死率较高,可严重影响患者的生命安全[1]。因此,早期诊断和治疗ARDS具有重要的临床意义。
目前,国内外关于ARDS的诊断标准较多[2-4],但尚无评估患者预后的确切指标。研究表明,急性生理学与慢性健康状况评分系统Ⅱ(APACHEⅡ)、感染相关器官功能衰竭评分系统(SOFA)及氧合指数可在一定程度上评估ARDS患者预后,但预测价值不高[5]。近年来,随着医疗技术的发展,脉搏指示连续心排血量(PiCCO)监测仪在重症医学领域得到了广泛应用,其监测的血管外肺水指数(EVLWI)和肺血管通透性指数(PVPI)可较好地反映ARDS患者血管外肺水量及肺泡毛细血管通透性[6-7]。本研究旨在探讨EVLWI及PVPI对重症ARDS患者预后的预测价值,现报道如下。
1 资料与方法
1.1 一般资料 选取2014年3月—2016年3月湖北省鄂东医疗集团黄石市中心医院(湖北理工学院附属医院)收治的重症ARDS患者31例,均符合2012年欧洲柏林会议制定的ARDS诊断标准[3],且患者氧合指数≤100 mm Hg(1 mm Hg=0.133 kPa);其中脓毒血症11例,有机磷中毒7例,交通事故多发伤5例,肺部感染3例,急性重症胰腺炎2例,急性化脓性胆囊炎2例,胃肠道术后1例。排除标准:(1)存在血流动力学不稳定者;(2)入院72 h内死亡者。根据预后将所有患者分为存活组14例与死亡组17例。两组患者性别、年龄、氧合指数、APACHEⅡ评分、SOFA评分、心率、血压比较,差异无统计学意义(P>0.05,见表1),具有可比性。本研究经医院医学伦理委员会审核批准,患者及其家属均签署知情同意书。
1.2 方法 两组患者入院后均予以常规治疗,包括循环支持、机械通气(保护性通气策略)、全身营养支持及予以肺血管扩张剂、糖皮质激素等药物治疗;且治疗期间采用美国GE公司生产的M70型心电监护仪监测患者生命体征。
1.3 观察指标 比较两组患者治疗前后EVLWI、PVPI、氧合指数,治疗72 h不同EVLWI、PVPI患者APACHEⅡ评分、SOFA评分[8]、氧合指数,并分析EVLWI、PVPI对重症ARDS患者预后的预测价值。(1)患者均经锁骨下静脉留置,静脉导管(购自美国Arrow公司),后于股动脉放置PiCCO动脉导管(购自德国 Pulsion公司),并连接PiCCO监测仪(PULSION PiCCO Plus生产,德国);分别于治疗前及治疗24 h、48 h、72 h经肺热稀释法测量EVLWI和PVPI,测量同时自锁骨下静脉或颈内静脉导管快速均匀注入(<7 s)8 ℃ 0.9%氯化钠溶液15 ml,连续测量2次取平均值。(2)分别采集患者治疗前及治疗24 h、48 h、72 h桡动脉血2 ml,采用德国ABL90型血气分析仪检测动脉血氧分压(PaO2)、吸入氧浓度(FiO2),并计算氧合指数。(3)采用APACHEⅡ评估所有患者病情严重程度,包括急性生理评分、年龄评分及慢性健康评分,APACHEⅡ评分越高表明病情越严重。(4)采用SOFA评估患者预后,SOFA评分越高表明患者预后越差。

2 结果
2.1 两组患者治疗前后EVLWI、PVPI、氧合指数比较 时间与方法在EVLWI、PVPI、氧合指数上无交互作用(P>0.05);时间在EVLWI、PVPI、氧合指数上主效应不显著(P>0.05);方法在EVLWI、PVPI、氧合指数上主效应显著(P<0.05);治疗48 h、72 h存活组患者EVLWI、PVPI低于死亡组,氧合指数高于死亡组,差异有统计学意义(P<0.05,见表2)。
2.2 相关性分析 Pearson相关性分析结果显示,EVLWI和PVPI与重症ARDS患者氧合指数呈负相关(r值分别为-0.772、-0.691,P<0.05)。
2.3 治疗72 h不同EVLWI和PVPI患者APACHEⅡ评分、SOFA评分、氧合指数比较 治疗72 h,EVLWI≥10 ml/kg和PVPI≥3患者APACHEⅡ评分、SOFA评分分别高于EVLWI<10 ml/kg和PVPI<3患者,氧合指数分别低于EVLWI<10 ml/kg和PVPI<3患者,差异有统计学意义(P<0.05,见表3~4)。
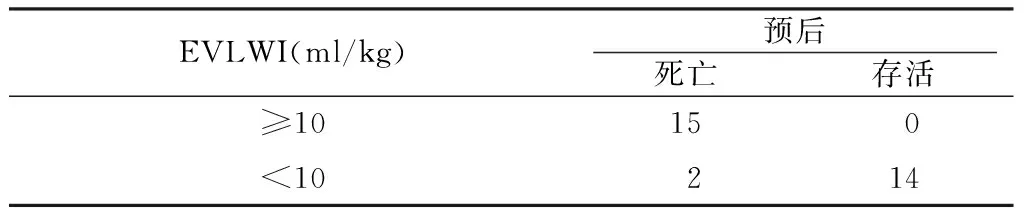
2.4 EVLWI与PVPI对重症ARDS患者预后的预测价值 以10 ml/kg为临界值,EVLWI预测重症ARDS患者预后的灵敏度为88.2%,特异度为100.0%,阳性预测值为100.0%,阴性预测值为87.5%,符合率为93.5%(见表5);以3为临界值,PVPI预测重症ARDS患者预后的灵敏度为76.5%,特异度为100.0%,阳性预测值为100.0%,阴性预测值为77.8%,符合率为87.1%(见表6)。

Table 3 Comparison of APACHEⅡ score,SOFA score and OI in patients with different EVLWI after 72 hours of treatment
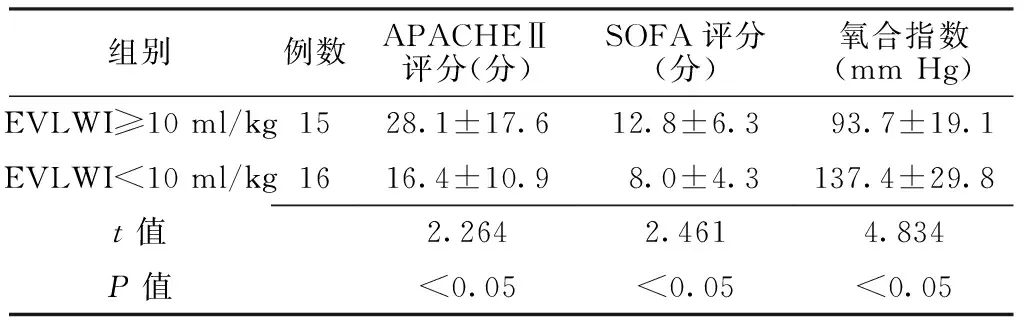
组别例数APACHEⅡ评分(分)SOFA评分(分)氧合指数(mmHg)EVLWI≥10ml/kg1528.1±17.612.8±6.3 93.7±19.1 EVLWI<10ml/kg1616.4±10.9 8.0±4.3 137.4±29.8t值2.2642.4614.834P值<0.05<0.05<0.05

Table 4 Comparison of APACHEⅡ score,SOFA score and OI in patients with different PVPI after 72 hours of treatment
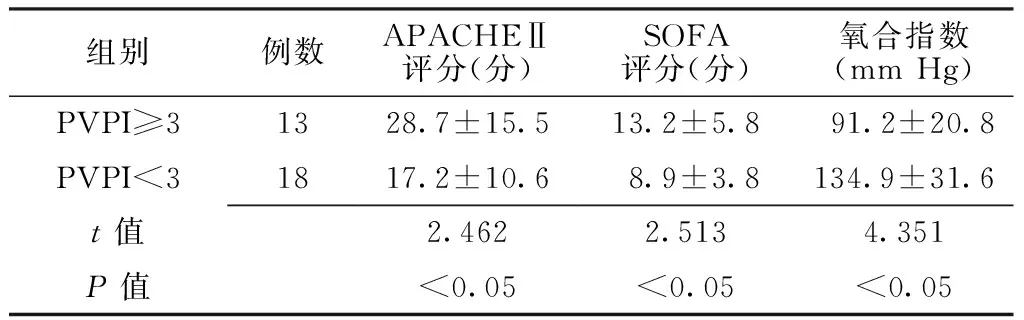
组别例数APACHEⅡ评分(分)SOFA评分(分)氧合指数(mmHg)PVPI≥31328.7±15.513.2±5.8 91.2±20.8 PVPI<31817.2±10.6 8.9±3.8 134.9±31.6t值2.4622.5134.351P值<0.05<0.05<0.05
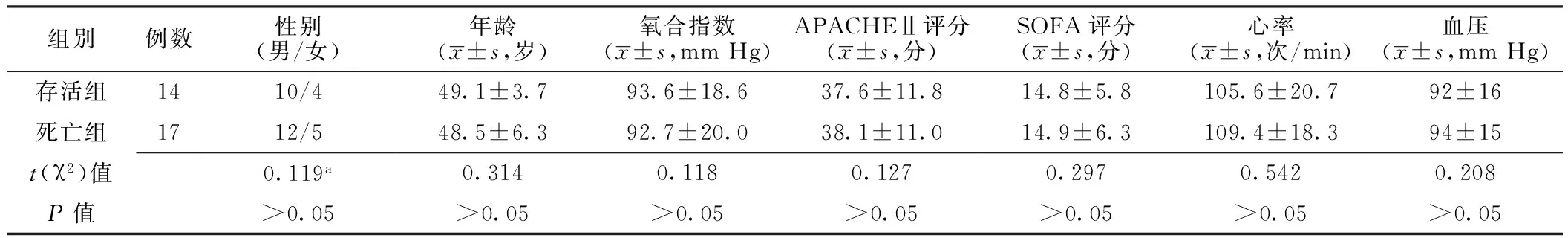
表1 两组患者一般资料比较
注:a为χ2值;APACHEⅡ=急性生理学与慢性健康状况评分系统Ⅱ,SOFA=感染相关器官功能衰竭评分系统
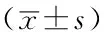
表2 两组患者治疗前后EVLWI、PVPI、氧合指数比较
注:与死亡组比较,aP<0.05;EVLWI=血管外肺水指数,PVPI=肺血管通透性指数
表5 EVLWI对重症ARDS患者预后的预测价值(例)
Table 5 Predictive value of EVLWI on prognosis in patients with severe ARDS
EVLWI(ml/kg)预后死亡存活≥1015 0 <10 2 14
表6 PVPI对重症ARDS患者预后的预测价值(例)
Table 6 Predictive value of PVPI on prognosis in patients with severe ARDS
PVPI(%)预后死亡存活≥313 0 <3 4 14
3 讨论
ARDS是以肺泡上皮细胞及毛细血管内皮细胞损伤导致肺水肿及弥漫性肺间质炎症为病理特征的临床综合征,临床表现为呼吸窘迫和持续低氧血症[9]。目前,临床常采用肺泡灌洗液蛋白含量与血清蛋白比值、EVLWI等指标反映肺毛细血管通透性[10-11]。PiCCO监测仪是通过中心导管注入冷指示剂(0~8 ℃的0.9%氯化钠溶液15 ml),经体循环、肺循环再到达导管探头末端,采用热稀释法计算两导管温度探头测得的温度差并输入PiCCO监测仪后得出多项具有临床意义的指标。近年来,随着PiCCO监测仪的发展,其可通过检测EVLWI与PVPI而提高对重症ARDS患者预后的预测价值[12]。
血管外肺水(EVLW)是分布于肺血管外的液体,由细胞内液、细胞外液及肺间质液组成,正常人约400 ml[13];其可客观反映肺损伤程度[14];肺毛细血管内静水压、肺间质静水压、肺毛细血管内胶体渗透压和肺间质胶体渗透压均可引起EVLWI变化,当EVLWI≥10 ml/kg时提示发生严重肺水肿[5,15]。PVPI可以客观反映肺泡毛细血管通透性,其正常值为1~3,对ARDS患者病情评估具有重要意义[16]。
本研究结果显示,治疗48 h、72 h存活组患者EVLWI、PVPI低于死亡组,氧合指数高于死亡组,提示治疗后存活重症ARDS患者的EVLWI、PVPI较低,氧合指数较高。本研究结果显示,EVLWI和PVPI与氧合指数呈负相关,提示EVLWI和PVPI与氧合指数有关,且氧合指数是评估ARDS患者病情的重要指标,故EVLWI和PVPI对患者预后可能具有评估价值。既往研究表明,以10 ml/kg为临界值时,EVLWI预测ARDS患者预后的灵敏度为67.00%,特异度为65.00%[17];3为临界值时,PVPI预测ARDS患者预后的灵敏度为85%,特异度为100%[18]。本研究结果显示,治疗72 h,EVLWI≥10 ml/kg和PVPI≥3患者APACHEⅡ评分、SOFA评分分别高于EVLWI<10 ml/kg患者,氧合指数低于EVLWI<10 ml/kg和PVPI<3患者;以10ml/kg为临界值时,EVLWI预测重症ARDS患者预后的灵敏度为88.2%,特异度为100.0%,阳性预测值为100.0%,阴性预测值为87.5%,符合率为93.5%;以3为临界值时PVPI预测重症ARDS患者预后的灵敏度为76.5%,特异度为100.0%,阳性预测值为100.0%,阴性预测值为77.8%,符合率为87.1%,与既往研究报道一致[19],提示EVLWI和PVPI对重症ARDS患者预后的预测价值较高。
综上所述,EVLWI和PVPI与重症ARDS患者氧合指数呈负相关,二者对重症ARDS患者预后的预测价值均较高,临床可通过动态监测EVLWI和PVPI而评估重症ARDS患者预后,继而指导治疗。但本研究样本量较小,EVLW与PVPI测定依赖于温度稀释技术,可能造成导管相关性感染等,且严重静脉压增高及全身炎性反应均会影响PVPI,有待扩大样本量并密切结合临床及其他监测指标进一步研究。
作者贡献:易智婷进行试验设计与实施、资料收集整理、撰写论文、成文并对文章负责,并进行质量控制及审校;王建春进行试验实施、评估、资料收集。
本文无利益冲突。
[1]侯昌权,陈文凯.氧合指数与血管外肺水指数的动态变化对急性呼吸窘迫综合征患者预后的判断价值[J].内科急危重症杂志,2016,22(6):454-456.DOI:10.11768/nkjwzzzz20160617.
[2]BERNARD G R,ARTIGAS A,BRIGHAM K L,et al.Report of the American-European consensus conference on ARDS:definitions,mechanisms,relevant outcomes and clinical trial coordination.The Consensus Committee[J].Intensive Care Med,1994,20(3):225-232.
[3]KUSHIMOTO S,TAIRA Y,KITAZAWA Y,et al.The clinical usefulness of extravascular lung water and pulmonary vascular permeability index to diagnose and characterize pulmonary edema:a prospective multicenter study on the quantitative differential diagnostic definition for acute lung injury/acute respiratory distress syndrome[J].Crit Care,2012,16(6):R232.DOI:10.1186/cc11898.
[4]中华医学会重症医学分会.急性肺损伤/急性呼吸窘迫综合征诊断与治疗指南(2006)[J].中华内科杂志,2007,46(5):430-435.DOI:10.3760/j.issn:0578-1426.2007.05.037.
[5]KUSHIMOTO S,ENDO T,YAMANOUCHI S,et al.Relationship between extravascular lung water and severity categories of acute respiratory distress syndrome by the Berlin definition[J].Crit Care,2013,17(4):R132.DOI:10.1186/cc12811.
[6]SIVAPALAN P,ST☞HR JENSEN J U.Timing of Therapy in Sepsis:Are Early Antibiotics Important for Prognosis?[J].Crit Care Med,2015,43(9):2030-2031.DOI:10.1097/CCM.0000000000001179.
[7]张瑜荣,邓立普,张小华,等.血管外肺水及肺血管通透性监测在ARDS患者中的临床价值[J].基础医学与临床,2014,34(5):719-722.
[8]孙丽晓.血管外肺水指数对急性呼吸窘迫综合征患者的预后评价[D].天津:天津医科大学,2014.
[9]严正,严洁,王秋卉,等.肺血管通透性指数用于急性呼吸窘迫综合征患者的预后评估[J].中国临床保健杂志,2013,16(4):404-406.DOI:10.3969/J.issn.1672-6790.2013.04.028.
[10]董旻.肺水相关指数对重症烧伤并发急性呼吸窘迫综合征患者病情预后的评估价值[D].南宁:广西医科大学,2014:1-39.
[11]ARDS DEFINITION TASK FORCE,RANIERI V M,RUBENFELD G D,et al.Acute respiratory distress syndrome:the Berlin Definition[J].JAMA,2012,307(23):2526-2533.DOI:10.1001/jama.2012.5669.
[12]唐钟祥,彭环庆,张燕华,等.血管外肺水指数及肺血管通透性指数对脓毒症相关ARDS预后的预测价值[J].牡丹江医学院学报,2016,37(5):36-38,50.
[13]JOZWIAK M,SILVA S,PERSICHINI R,et al.Extravascular lung water is an independent prognostic factor in patients with acute respiratory distress syndrome[J].Crit Care Med,2013,41(2):472-480.DOI:10.1097/CCM.0b013e31826ab377.
[14]TAGAMI T,KUSHIMOTO S,YAMAMOTO Y,et al.Validation of extravascular lung water measurement by single transpulmonary thermodilution:human autopsy study[J].Crit Care,2010,14(5):R162.DOI:10.1186/cc9250.
[15]胡雪珍.血管外肺水指数和肺血管通透性指数在急性呼吸窘迫综合征患者中的应用价值探讨[D].苏州:苏州大学,2016:1-77.
[16]唐坎凯.ARDS患者血管外肺水指数与预后的关系[D].杭州:浙江大学,2015:1-52.
[17]吴翔,陶飞,胡桂芳,等.急性呼吸窘迫综合征患者血管外肺水指数与肺毛细血管通透性指数的临床意义[J].深圳中西医结合杂志,2016,26(9):130-133,封3.DOI:10.16458/j.cnki.1007-0893.2016.09.066.
[18]CORNEJO R A,DAZ J C,TOBAR E A,et al.Effects of prone positioning on lung protection in patients with acute respiratory distress syndrome[J].Am J Respir Crit Care Med,2013,188(4):440-448.DOI:10.1164/rccm.201207-1279OC.
[19]GATTINONI L,PESENTI A,CARLESSO E.Body position changes redistribute lung computed-tomographic density in patients with acute respiratory failure:impact and clinical fallout through the following 20 years[J].Intensive Care Med,2013,39(11):1909-1915.DOI:10.1007/s00134-013-3066-x.
(本文编辑:李洁晨)
Predictive Value of Extravascular Lung Water Index and Pulmonary Vascular Permeability Index on Prognosis in Patients with Severe Acute Respiratory Distress Syndrome
YIZhi-ting1,WANGJian-chun2
1.DepartmentofRespiratoryMedicine,HuangshiCentralHospitalofEdongMedicalGroupofHubeiProvince(theAffiliatedHospitalofHubeiPolytechnicUniversity),Huangshi435005,China2.DepartmentofPhysicalExamination,AikangHospitalofHuangshi,Huangshi435000,ChinaCorrespondingauthor:WANGJian-chun,E-mail:jian914@163.com
Objective To evaluate the predictive value of extravascular lung water index(EVLWI)and pulmonary vascular permeability index(PVPI)on prognosis in patients with severe acute respiratory distress syndrome(ARDS).Methods A total of 31 patients with severe ARDS were selected in Huangshi Central Hospital of Edong Medical Group of Hubei Province(the Affiliated Hospital of Hubei Polytechnic University)from March 2014 to March 2016,and they were divided into survival group(n=14)and death group(n=17)according to the prognosis.Patients of the two groups
conventional treatment after admission,and vital signs were monitored during the treatment.EVLWI,PVPI and OI were compared between the two groups before treatment,after 24 hours,48 hours and 72 hours of treatment,APACHEⅡ score,SOFA score and OI were compared in patients with different EVLWI or PVPI after 72 hours of treatment;Pearson correlation analysis was used to analyze the correlations of EVLWI and PVPI with OI of patients with severe ARDS,and four-fold table was used to evaluate the predictive value of EVLWI and PVPI on prognisis in patients with severe ARDS.Results There was no interaction between time and method in EVLWI,PVPI or OI(P>0.05);main effect of time was not significant in EVLWI,PVPI or OI(P>0.05),while main effect of method was significant in EVLWI,PVPI and OI(P<0.05);after 48 hours and 72 hours of treatment,EVLWI and PVPI of survival group were statistically significantly lower than those of death group,while OI of survival group was statistically significantly higher than that of death group,respectively(P<0.05).Pearson correlation analysis results showed that,EVLWI(r=-0.772)and PVPI(r=-0.691)was negatively correlated with OI of patients with severe ARDS,respectively(P<0.05).After 72 hours of treatment,APACHEⅡ score and SOFA score of patients with EVLWI equal or over 10 ml/kg,with PVPI equal or over 3 were statistically significantly higher than those of patients wiht EVLWI less than 10 ml/kg,with PVPI less than 3,while OI of patients with EVLWI equal or over 10 ml/kg,with PVPI equal or over 3 was statistically significantly lower than that of patients wiht EVLWI less than 10 ml/kg,with PVPI less than 3(P<0.05).Taking 10 ml/kg as critical value,the sensitivity of EVLWI in predicting prognosis in patients with severe ARDS was 88.2%,the specificity was 100.0%,the positive predictive value was 100.0%,the negative predictive value was 87.5%,the coincidence rate was 93.5%;taking 3 as critical value,the sensitivity of PVPI in predicting prognosis in patients with severe ARDS was 76.5%,the specificity was 100.0%,the positive predictive value was 100.0%,the negative predictive value was 77.8%,the coincidence rate was 87.1%.Conclusion EVLWI and PVPI are negatively correlated with OI of patients with severe ARDS,both them has significantly high predictive value on prognisis in patients with severe ARDS.
Respiratory distress syndrome,adult;Extravascular lung water index;Pulmonary vascular permeability index;Prognosis
王建春,E-mail:jian914@163.com
R 563.8
A
10.3969/j.issn.1008-5971.2017.07.009
2017-04-02;
2017-07-07)
1.435005湖北省黄石市,湖北省鄂东医疗集团黄石市中心医院(湖北理工学院附属医院)呼吸内科
2.435000湖北省黄石市爱康医院体检科