冠状动脉CT血管造影对慢性完全闭塞病变患者介入治疗的预测价值
2017-08-09崔松陈亚磊王瑞贺毅栗佳南田锐葛长江苑飞黄榕翀宋现涛吕树铮
崔松 陈亚磊 王瑞 贺毅 栗佳南 田锐 葛长江 苑飞 黄榕翀 宋现涛 吕树铮
·临床研究·
冠状动脉CT血管造影对慢性完全闭塞病变患者介入治疗的预测价值
崔松 陈亚磊 王瑞 贺毅 栗佳南 田锐 葛长江 苑飞 黄榕翀 宋现涛 吕树铮
目的 运用CT血管造影(CT angiography, CTA)分析影响慢性完全闭塞病变(chronic total occlusion lesions,CTO)介入治疗的病变特征及对介入治疗结果的预测价值。方法 入选113例患者,分为介入治疗成功组(64例)与介入治疗失败组(52例)。收集患者资料,运用CTA分析两组患者CTO特征,并采用多因素logistic回归分析判断影响CTO介入治疗成功的因素,利用ROC曲线判断并评价CT-CTO评分和日本CTO评分(J-CTO评分)的诊断效能。结果 介入治疗失败组患者闭塞段近端分叉(75.0%比54.7%,P=0.042)、闭塞段远端纤维帽形态不清晰(17.3%比4.6%,P=0.023)、闭塞段内是否存在钙化病变(73.1%比53.1%,P=0.033)、闭塞段长度[(26.0±16.6)mm比(16.8±11.3)mm,P=0.003]、闭塞段长度≥20 mm(46.2%比25.0%,P=0.007)均高于介入治疗成功组,差异均有统计学意义。多因素logistic回归分析显示,闭塞段远端纤维帽形态不清晰、闭塞段近端分叉、闭塞长度≥20 mm是影响CTO介入治疗成功的主要因素。ROC曲线下的面积CT-CTO评分预测介入治疗成功率(87.8%比73.9%,P<0.05)高于J-CTO评分。结论 闭塞段远端纤维帽形态不清晰、闭塞段近端分叉、闭塞段长度≥20 mm是影响CTO介入治疗成功的独立危险因素,CTA能够预测CTO介入治疗的成功率,与J-CTO评分相比,CT-CTO评分对介入治疗成功率具有更高的预测价值。
CT血管造影; 慢性完全闭塞病变; 介入治疗
慢性完全闭塞病变(chronic total occlusion lesions, CTO)是冠状动脉介入治疗领域的壁垒。在疑诊冠心病患者中,经冠状动脉造影(coronary angiography,CAG)检查约1/3患者可见至少1支冠状动脉存在CTO,但目前仅有8%~15%患者接受介入治疗,主要在于CTO的介入治疗成功率低,并发症发生风险高、花费高等原因限制了介入治疗的选择[1-2]。术前合理全面评估CTO患者局部病变特征及介入治疗的价值,有助于指导选择治疗策略及提高其介入治疗的成功率。近年来出现大量关于CT血管造影(CT angiography, CTA)评估CTO特征及介入治疗的研究,研究证实病变血管齐头闭塞、钙化、严重扭曲、既往尝试开通失败都是影响介入治疗成功的独立危险因素,闭塞病变长度是导致介入治疗失败的因素之一,并且回旋支闭塞是影响介入治疗成功的因素,不同的研究对病变特征的分析尚存在争议[3-4]。
本研究通过CTA分析术前CTO患者病变特征及临床资料,旨在评估CTO介入治疗患者病变特征及对介入治疗的预测价值。
1 对象与方法
1.1 研究对象
本研究为回顾性研究,连续纳入2013年6月至2016年8月就诊于首都医科大学附属北京安贞医院心内科,疑似或确诊为冠心病患者2132例。入选标准:(1)疑似或确诊为冠心病的患者;(2)经CAG确诊至少1支血管完全闭塞,前向 TIMI血流0级,且闭塞时间超过3个月以上的患者;(3)CAG术前60 d内接受CTA检查患者;(4)均接受介入治疗。排除标准:(1)存在3级运动伪影的冠状动脉CTA图像;(2)CAG或者CTA影像资料缺失患者;(3)闭塞血管曾经接受冠状动脉旁路移植术治疗患者;(4)支架内血栓形成患者;(5)频发室性早搏或心房颤动等严重心律失常患者;(6)碘对比剂过敏者;(7)严重肾功能不全者(血肌酸酐>132 μmol/L);(8)活动性出血及明显出血倾向者;(9)孕期或妊娠期妇女。根据入选及排除标准,最终共入选113例患者。所有受试者CTA检查前已被告知该项检查技术的基本信息和对比剂相关信息,并签署知情同意书。
1.2 研究方法
患者介入治疗术前60 d行CTA检查。CTA检查运用Toshiba Aquilion 64 层螺旋CT机,由两位经验丰富的影像医师对图像进行后期重建及分析,包括容积再现、多平面重建、最大密度投影、曲面重建等模式,选择最佳时相重建的全部数据,测量评估。所有患者术中按标准的Judkins法进行CAG检查,所有CTO血管根据术者经验及病变特征选择术式,30 min内导丝通过闭塞病变且介入治疗后病变血管前向TIMI血流Ⅲ级,残余狭窄<25%为闭塞段成功开通,定义为手术成功。若反复尝试导丝无法通过闭塞病变,出现冠状动脉夹层或穿孔等并发症,血流动力学不稳定或患者不能耐受手术时,终止操作定义为失败。介入治疗手术均由5年以上有冠状动脉介入治疗经验的心血管内科医师完成。
1.3 观察指标
患者基础资料收集,包括入院常规检查肝肾功能、血红蛋白和空腹血糖等。并且对患者术前CTA影像进测量评估以下参数:闭塞部位、闭塞段长度、闭塞段钙化程度、闭塞近端纤维帽形态、闭塞近端是否有分叉、闭塞段扭曲程度、闭塞远端纤维帽形态、闭塞远端是否有分叉、闭塞远段血管有否有狭窄、闭塞段以远血管充盈情况。
日本CTO评分(J-CTO 评分)[5]和CT-CTO评分[6]根据CAG及临床特征参数制定。 J-CTO评分包含病变血管齐头闭塞、钙化、闭塞段长度>20 mm及严重扭曲4项病变特征和既往尝试开通失败1项临床特征。CT-CTO评分包括闭塞段远端纤维帽形态不清晰、闭塞近段分叉、闭塞长度≥20 mm是影响CTO介入治疗失败的主要因素。
1.4 统计学分析

2 结果
2.1 两组患者临床资料分析
113例患者根据介入治疗成功与否分为介入治疗成功组64例和介入治疗失败组52例。两组患者年龄、性别、体重指数(BMI)、高血压病、糖尿病、心肌梗死病史比较,差异均无统计学意义(均P>0.05)。介入治疗失败组吸烟史(65.4%比42.2%,P=0.033)高于介入治疗成功组;但高密度脂蛋白胆固醇(HDL-C)[(0.9±0.2)mmol/L比(1.0±0.2)mmol/L,P=0.006]显著低于介入治疗成功组,差异均有统计学意义(表1)。
2.2 CTA分析CTO特征
介入治疗失败组患者闭塞段近端分叉(75.0%比54.7%,P=0.042)、闭塞段远端纤维帽形态不清晰(17.3%比4.6%,P=0.023)、钙化病变(73.1%比53.1%,P=0.033)、闭塞段长度[(26.0±16.6)mm比(16.8±11.3)mm,P=0.003]、闭塞段长度≥20 mm(46.2%比25.0%,P=0.007)均高于介入治疗成功组,差异均有统计学意义(表2)。
2.3 CTA病变特征多因素回归分析
将闭塞段近端分叉、闭塞段远端纤维帽形态不清晰、闭塞段内是否存在钙化病变、闭塞段长度、闭塞段长度≥20 mm纳入多因素logistic回归分析模型。CTA预测CTO介入治疗成功病变特征的多因素Logistic回归分析显示:闭塞段远端纤维帽形态不清晰、闭塞段近端分叉、闭塞长度≥20 mm是影响CTO介入治疗失败的主要因素(表3)。

表1 两组患者临床基线资料比较
注:BMI,体重指数;TC,总胆固醇;LDL-C,低密度脂蛋白胆固醇;HDL-C,高密度脂蛋白胆固醇;LAD,左前降支;LCX,回旋支;RCA,右冠状动脉
2.4 评价CT-CTO评分的诊断效能
根据CTO病变特征多因素logistic回归分析,CT-CTO评分包括闭塞段远端纤维帽形态不清晰,闭塞段近端分叉、闭塞长度≥20 mm各赋予为1分,分为0、1、2、3四个等级。随着CT-CTO评分等级的升高,CTO介入治疗成功率逐渐减低,分别为85.7%、65.8%、33.3%、0;当等级为3级时,介入治疗失败率为100%(图1)。J-CTO评分包含齐头闭塞、钙化、闭塞段长度>20 mm及严重扭曲4项病变特征和既往尝试开通失败1项临床特征各赋予1分,分为0、1、2、3、4五个等级。随着J-CTO评分等级逐渐增加,CTO介入治疗成功率逐渐减低,介入治疗成功率分别为92.9%、63.0%、45.0%、36.8%、20.0%(图2)。CT-CTO 评分ROC曲线下面积0.877(95%CI0.764~0.991,P<0.001)。J-CTO 评分曲线下面积0.739(95%CI0.589~0.889,P<0.005)。CT-CTO评分预测介入治疗成功率(87.8% 比73.9%,P<0.05)高于J-CTO评分,差异有统计学意义(图3)。
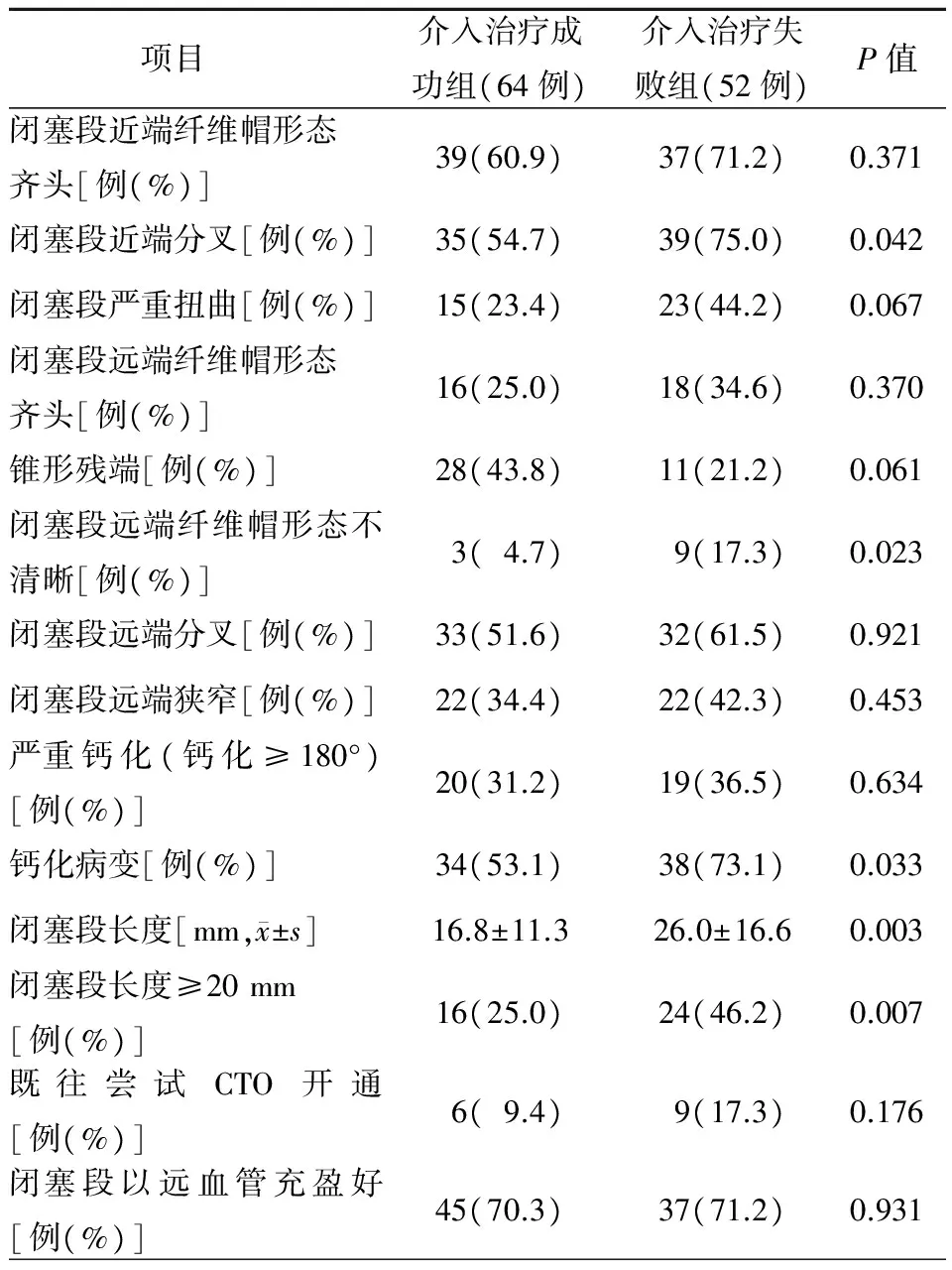
表2 CTA评价两组患者病变特征比较
注:CTA,CT血管造影;CTO,慢性完全闭塞病变
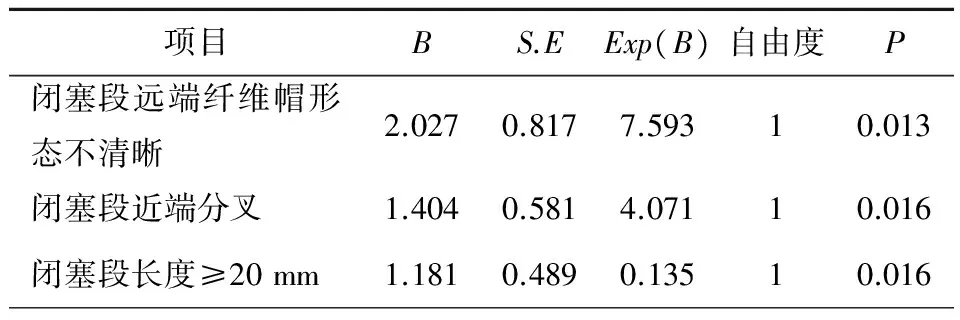
表3 多因素logistic回归分析CTO特征
注:CTO,慢性完全闭塞病变

图1 CT-CTO 评分与手术成功率(%)的相关性(Pearson r=-0.994, P<0.01)
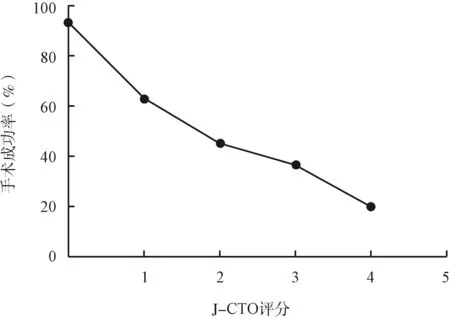
图2 J-CTO 评分与手术成功率(%)的相关性(Pearson r=-0.977; P<0.05)
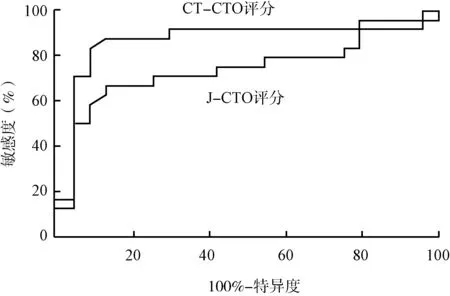
图3 对比CT-CTO评分与J-CTO评分的诊断效能
3 讨论
既往研究发现,术前应用CTA对CTO特征的局部判断,有助于指导介入治疗和提高手术成功率,同时可以减少手术时间、对比剂剂量,最大限度降低手术治疗过程中受到的放射性损害,术前能够准确筛选适合介入治疗的患者,可将手术成功率提高至90%以上[7]。
本研究发现闭塞段远端纤维帽形态不清晰、闭塞段近端分叉、钙化病变、闭塞段长度、闭塞段长度≥20 mm是影响CTO介入治疗成功的独立危险因素。闭塞段远端纤维帽形态不清晰,导致导丝无法识别血管走行,增加导丝通过闭塞段时间可能是导致介入治疗失败的原因。有研究表明,影响CTO介入治疗成功的常见原因包括动脉粥样硬化斑块负荷过重、闭塞段长度过长、无法识别闭塞段近端的残端、闭塞段内存在严重的纤维化及钙化导致支架通过困难、闭塞段的非锥形形态、闭塞段成角大于45°、闭塞节段>20 mm、血管直径<2.5 mm、闭塞血管存在多处病变、严重钙化、桥侧支存在、闭塞部位有分支血管、长闭塞节段、血管迂曲等[7-9],这与本研究结果一致。
根据CTO病变特征多因素logistic回归分析,CT-CTO评分包括闭塞段远端纤维帽形态不清晰,闭塞近段分叉、闭塞长度≥20 mm等因素赋予为1分,0、1、2、3分四个等级,随着评分等级的升高,病变特点越来越复杂,介入治疗成功率呈下降趋势,当病变复杂程度等级为3级时,介入治疗成功率为0。一项多中心回顾性研究发现,CTA预测多节段闭塞、钝性残端、闭塞部位成角、严重钙化、闭塞时间长短以及闭塞部位既往是否介入治疗是预测导丝30 min通过闭塞病变的独立危险因素,危险因素越多,CTO开通成功率越低,当上述危险因素≥3个,介入治疗成功率≤24%[6]。与CT-CTO 评分相比,J-CTO评分包含齐头闭塞、钙化、闭塞段长度>20 mm及严重扭曲4项病变特征和既往尝试开通失败1项临床特征,当存在3个或3个以上危险因素时,成功率仅为10%[2]。本研究同时使用J-CTO评分预测介入治疗成功率,随着评分等级升高,手术成功率逐渐降低。CT-CTO评分预测介入治疗成功率诊断效能(87.8%比73.9%,P<0.05)高于J-CTO评分,主要原因可能与CTA准确地识别闭塞远端纤维帽形态和准确闭塞段长度相关。J-CTO评分显示既往尝试开通失败是预测介入治疗效果的独立危险因素,说明CTO介入治疗的效果与术者经验及操作技巧密切相关,这与Christopoulos等[4]研究结果相一致。
有研究显示,CTO介入治疗成功率为55%~80%,然而非CTO介入治疗成功率可达90%以上[10-13]。随着介入治疗手段和介入器械不断更新与发展,CTO介入治疗成功率不断提高,有经验的术者,CTO介入治疗成功率可达80%~90%。然而不同技术熟练程度的介入医师开通CTO的成功率相差甚远,而且CTO介入治疗中所使用介入器材花费、介入医师与患者接受射线曝光时间均很多[14-16]。
本研究为单中心回顾性研究,纳入样本量较少,同时未对术者经验进行专门的评估,可能会对手术的成功率有所影响,但研究终点采用30 mim内导丝通过闭塞病变定义为手术成功,初步排除术者经验对结局的影响。应进一步进行前瞻性、多中心、大样本量研究,进一步论证本研究结果的价值。
[1] Levine GN, Bates ER, Blankenship JC, et al.2011 ACCF/AHA/SCAI guideline for percutaneous coronary intervention. a report of the American College of Cardiology Foundation/American Heart Association task force on practice guidelines and the society for cardiovascular angiography and interventions.J Am Coll Cardiol,2011,58(24):e44-122.
[2] Morino Y, Abe M, Morimoto T, et al.Predicting successful guidewire crossing through chronic total occlusion of native coronary lesions within 30 minutes: the J-CTO (Multicenter CTO Registry in Japan) score as a difficulty grading and time assessment tool.JACC Cardiovasc Interv,2011,4(2):213-221.
[3] Opolski, MP, Achenbach S, Schuhback A, et al.Coronary computed tomographic prediction rule for time-efficient guidewire crossing through chronic total occlusion: insights from the CT-RECTOR multicenter registry (Computed Tomography Registry of Chronic Total Occlusion Revascularization).JACC Cardiovasc Interv,2015,8(2):257-267.
[4] Christopoulos G, Kandzari DE, Yeh RW, et al.Development and validation of a novel scoring system for predicting technical success of chronic total occlusion percutaneous coronary interventions: the PROGRESS CTO (prospective global registry for the study of chronic total occlusion intervention) score.JACC Cardiovasc Interv,2016,9(1):1-9.
[5] 赵林,金泽宁,张晓江,等. 国产单环网篮导丝在冠状动脉慢性完全闭塞病变逆向介入治疗中的应用.中国介入心脏病学杂志,2017,25(4):197-201.
[6] Hoe J.CT coronary angiography of chronic total occlusions of the coronary arteries: how to recognize and evaluate and usefulness for planning percutaneous coronary interventions.Int J Cardiovasc Imaging,2009, 25 Suppl 1:43-54.
[7] Di Mario C, Werner GS, Sianos G, et al.European perspective in the recanalisation of chronic total occlusions (CTO): consensus document from the EuroCTO Club.EuroIntervention,2007,3(1):30-43.
[8] Stone GW, Colombo A, Teirstein PS, et al.Percutaneous recanalization of chronically occluded coronary arteries: procedural techniques, devices, and results.Catheter Cardiovasc Interv,2005,66(2):217-236.
[9] Ehara M, Terashima M, Kawai M, et al.Impact of multislice computed tomography to estimate difficulty in wire crossing in percutaneous coronary intervention for chronic total occlusion.J Invasive Cardiol,2009,21(11):575-582.
[10] Abbot, JD, Kip KE, Vlachos HA, et al.Recent trends in the percutaneous treatment of chronic total coronary occlusions.Am J Cardiol,2006,97(12):1691-1696.
[11] Galassi AR, Tomasello SD, Reifart N, et al.In-hospital outcomes of percutaneous coronary intervention in patients with chronic total occlusion: insights from the ERCTO (European Registry of Chronic Total Occlusion) registry.EuroIntervention,2011,7(4):472-479.
[12] Joyal D, Afilalo J, Rinfret S,et al.Effectiveness of recanalization of chronic total occlusions: a systematic review and meta-analysis.Am Heart J,2010,160(1):179-187.
[13] Soon KH, Selvanayagam JB, Cox N, et al.Percutaneous revascularization of chronic total occlusions: review of the role of invasive and non-invasive imaging modalities.Int J Cardiol,2007,116(1):1-6.
[14] Michael T, Karmpaliotis D, Brilakis ES, et al.Procedural outcomes of revascularization of chronic total occlusion of native coronary arteries (from a multicenter United States registry).Am J Cardiol,2013,112(4):488-492.
[15] Liu W, Wagatsuma K, Toda M, et al.Short- and long-term follow-up of percutaneous coronary intervention for chronic total occlusion through transradial approach: tips for successful procedure from a single-center experience.J Interv Cardiol,2011,24(2):137-143.
[16] Choi JH, Koo BK, Yoon YE, et al.Diagnostic performance of intracoronary gradient-based methods by coronary computed tomography angiography for the evaluation of physiologically significant coronary artery stenoses. Eur Heart J Cardiovasc Imaging,2012 ,13(12):1001-1007.
Predictive value of coronary CT angiography in chronic total occlusion lesions interventional therapy
CUISong,CHENYa-lei,WANGRui,HEYi,SUJia-nan,TIANRui,GEChang-jiang,YUANFei,HUANGRong-chong,SONGXian-tao,LYUShu-zheng.
DepartmentofCardiology,BeijingAnzhenHospital,CapitalMedicalUniversity,Beijing100029,China
Correspondingauthor:SONGXian-tao,Email:songxiantao@medmail.com.cn
Objective To analyze the characteristics of preoperative CTO lesions by coronary CT angiography (CCTA) and to compare the lesion characteristics and clinical data of patients with subsequent vs failed PCI.Methods A total of 113 patients were randomly selected and 116 vessels were analyzed by CCTA before PCI.The patients were further investigated as PCI success group vs PCI failure group according to their PCI result.Multivariate logistic regression analysis was used to determine the factors that affected the success of CTO intervention. The ROC curve was used to determine and evaluate the CT-CTO score and J-CTO score for diagnostic efficacy.Results The success rate of PCI was 55.2%. 64 lesions were successfully opened, with the success rate of 72.4%. The prevalence of smoking in patients in the PCI failure group was significantly higher than that in PCI success group (65.4%vs. 42.2%,P<0.05).There were no significant differences between the two groups in age, gender, history of hypertension, diabetes mellitus, and myocardial infarction(P>0.05).Statistical differences were observed between the PCI success group and the PCI failure group in the presence of occlusion segment head-end bifurcation, occlusion severe incision, severe calcification (calcification≥ 180°), occlusion segment length ≥20 mm, occlusion of calcification lesions, occlusion segment distal shape of the unambiguous of fiber cap shape of the distal occlusion segment under CCTA(P<0.05).In the PCI failure group, approximately 17.3% of the patients had previous attempt to open the CTO lesions, which were higher than the PCI success group (9.4%).However, The difference was not statistically significant (P>0.05). Multivariate logistic regression analysis showed that the unambiguous distal fibrous cap of the occlusion segment and the occlusion of the proximal branch and the occlusion length ≥20 mm were the main factors affecting the failure of CTO intervention. In terms of prediction, the predictive value 30 CT-CTO score yielded a higher area under the ROC curve than that of the J-CTO score (0.8776vs0.7387 ,P≤0.05).Conclusion CT angiography can predict the success rate of intervention for CTO lesions. Compared with J-CTO score, CT-CTO score has a higher predictive value. Unambiguous fiber cap shape, occlusion segment head end bifurcation, occlusion segment length ≥20 mm were the independent risk factors that affecting the success of CTO operation.
CT angiography; Chronic total occlusion lesions; Interventional therapy
10.3969/j.issn.1004-8812.2017.06.006
首都临床特色应用研究与成果推广(Z161100000516139);北京力生心血管健康基金会领航基金项目(LHJJ20158521);大连医科大学转化医学项目(2015003)
100029 北京,首都医科大学附属北京安贞医院心内科(崔松、陈亚磊、栗佳南、田锐、葛长江、苑飞、宋现涛、吕树铮),放射科(王瑞、贺毅);辽宁大连,大连医科大学第一附属医院心内科(黄榕翀)
宋现涛,Email:songxiantao@medmail.com.cn
R541.4
2017-02-26)