平均血小板体积与ST段抬高型心肌梗死患者左心室收缩功能的关系研究
2017-05-02黄震浩范成辉
黄震浩,范成辉
·论著·
平均血小板体积与ST段抬高型心肌梗死患者左心室收缩功能的关系研究
黄震浩,范成辉
目的 分析平均血小板体积(MPV)与ST段抬高型心肌梗死(STEMI)患者左心室收缩功能的关系。方法 选取2014-10-01—2016-05-01在同济大学附属东方医院心内科住院的首诊STEMI患者117例,根据是否伴有左心室收缩功能损伤分为对照组83例(无左心室收缩功能损伤)和观察组34例(有左心室收缩功能损伤)。回顾性分析两组患者的病历资料,记录其一般资料、实验室检查指标及入院前药物使用情况,并采用多因素Logistic回归分析STEMI患者左心室收缩功能损伤的影响因素。结果 两组患者性别、腰围、糖尿病发生率、高血压发生率、高脂血症发生率、前壁心肌梗死发生率、梗死前心绞痛发生率、吸烟率、发病至就诊时间及门-球囊扩张时间比较,差异无统计学意义(P>0.05);观察组患者年龄大于对照组(P<0.05)。两组患者总胆固醇、三酰甘油、高密度脂蛋白胆固醇、低密度脂蛋白胆固醇、糖化血红蛋白、血红蛋白水平及血细胞比容、血小板计数比较,差异无统计学意义(P>0.05);观察组患者氨基末端脑钠肽前体水平高于对照组,MPV大于对照组(P<0.05)。两组患者中使用血管紧张素转换酶抑制剂/血管紧张素Ⅱ受体拮抗剂、β-受体阻滞剂、钙通道阻滞剂、华法林、利尿剂、阿司匹林及氯吡格雷者所占比例比较,差异无统计学意义(P>0.05)。多因素Logistic回归分析结果显示,MPV是STEMI患者左心室收缩功能损伤的独立影响因素〔OR=3.640,95%CI(3.047,9.440),P<0.05〕。结论 MPV增大与STEMI患者左心室收缩功能损伤有关。
心肌梗死;平均血小板体积;左心室收缩功能
目前,冠心病的发病率和病死率均较高,已成为严重威胁人类生命健康的主要疾病之一。因此,研究冠心病的发生、发展及治疗具有重要的临床意义。平均血小板体积(MPV)是外周血中单个血小板的平均体积,也是血液中所有血小板体积的平均数,MPV增大表明血小板体积总体增大。有研究显示,肺动脉高压、肥厚型心肌病及失代偿期心力衰竭患者发生血栓事件均与MPV增大有关,而MPV与左心室收缩和舒张功能障碍之间的关系尚未明确[1-3]。
ST段抬高型心肌梗死(ST segment elevation myocardial infarction,STEMI)是常见的冠心病类型,其主要病理学基础是血小板活化、聚集及血栓形成,而血小板活性与MPV密切相关。MPV增大的血小板含有的α颗粒〔血管性血友病因子(vWF)、血小板衍生因子、转化生长因子等〕、致密颗粒(含二磷酸腺苷、Ca2+、5-羟色胺)及血栓素A2较多,活性也相应增强,进而导致血栓栓塞面积变大及心肌缺血持续时间延长,而STEMI患者左心室收缩功能损伤与冠状动脉内血栓栓塞面积变大及心肌缺血持续时间延长有关[4-6],故探究MPV与STEMI患者左心室收缩功能的关系对有效防治左心室收缩功能损伤具有重要意义。
1 对象与方法
1.1 研究对象 选取2014-10-01—2016-05-01在同济大学附属东方医院心内科住院的首诊STEMI患者117例,根据是否伴有左心室收缩功能损伤分为对照组83例(无左心室收缩功能损伤)和观察组34例(有左心室收缩功能损伤)。排除标准:(1)合并先天性心脏病、心肌病及严重感染性疾病者;(2)合并脑梗死、脑出血者;(3)合并严重肝肾功能不全者;(4)合并睡眠呼吸暂停综合征者;(5)合并恶性肿瘤者。
1.2 诊断标准
1.2.1 STEMI 具有典型的缺血性胸痛症状,且持续时间超过30 min;血清心肌坏死标志物水平升高并伴有动态演变;心电图具有典型的ST段抬高特征性改变[7]。
1.2 左心室收缩功能损伤 采用心脏彩色多普勒超声仪检测患者左心室射血分数(LVEF),将LVEF≤50%定义为左心室收缩功能损伤[8]。
1.3 研究方法 回顾性分析两组患者病历资料,记录其一般资料、实验室检查指标及入院前药物使用情况。(1)一般资料包括性别、年龄、腰围、基础疾病(糖尿病、高血压、高脂血症、前壁心肌梗死、梗死前心绞痛)发生情况、吸烟率、发病至就诊时间及门-球囊扩张时间。糖尿病诊断标准:空腹血糖>7.0 mmol/L或餐后2 h血糖>11.1 mmol/L;高血压诊断标准:收缩压≥140 mm Hg(1 mm Hg=0.133 kPa)和/或舒张压≥90 mm Hg;高脂血症诊断标准:总胆固醇(TC)>5.72 mmol/L,三酰甘油(TG)>1.70 mmol/L,高密度脂蛋白胆固醇(HDL-C)<0.91 mmol/L,低密度脂蛋白胆固醇(LDL-C)>3.64 mmol/L;将连续或累积吸烟6个月或以上定义为吸烟。(2)实验室检查指标包括血脂指标、氨基末端脑钠肽前体(NT-proBNP)、糖化血红蛋白(HbA1c)及血常规指标〔血红蛋白(Hb)、血细胞比容(HCT)、血小板计数(PLT)及MPV〕。(3)统计患者入院前血管紧张素转换酶抑制剂(ACEI)/血管紧张素Ⅱ受体拮抗剂(ARB)、β-受体阻滞剂、钙通道阻滞剂、华法林、利尿剂、阿司匹林及氯吡格雷使用情况。

2 结果
2.1 两组患者一般资料比较 两组患者性别、腰围、糖尿病发生率、高血压发生率、高脂血症发生率、前壁心肌梗死发生率、梗死前心绞痛发生率、吸烟率、发病至就诊时间及门-球囊扩张时间比较,差异无统计学意义(P>0.05);观察组患者年龄大于对照组,差异有统计学意义(P<0.05,见表1)。
2.2 两组患者实验室检查指标比较 两组患者TC、TG、HDL-C、LDL-C、HbA1c、Hb水平及HCT、PLT比较,差异无统计学意义(P>0.05);观察组患者NT-proBNP水平高于对照组,MPV大于对照组,差异有统计学意义(P<0.05,见表2)。
2.3 两组患者入院前药物使用情况比较 两组患者中使用ACEI/ARB、β-受体阻滞剂、钙通道阻滞剂、华法林、利尿剂、阿司匹林及氯吡格雷者所占比例比较,差异无统计学意义(P>0.05,见表3)。
2.4 多因素分析 将可能影响左心室收缩功能损伤的指标作为自变量,将左心室收缩功能损伤作为因变量(变量赋值见表4)进行多因素Logistic回归分析,结果显示,MPV是STEMI患者左心室收缩功能损伤的独立危险因素(P<0.05,见表5)。
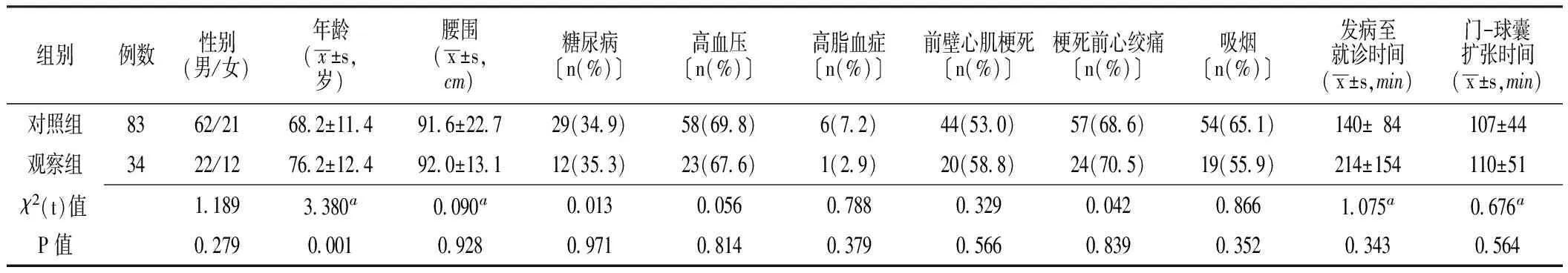
表1 两组患者一般资料比较
注:a为t值
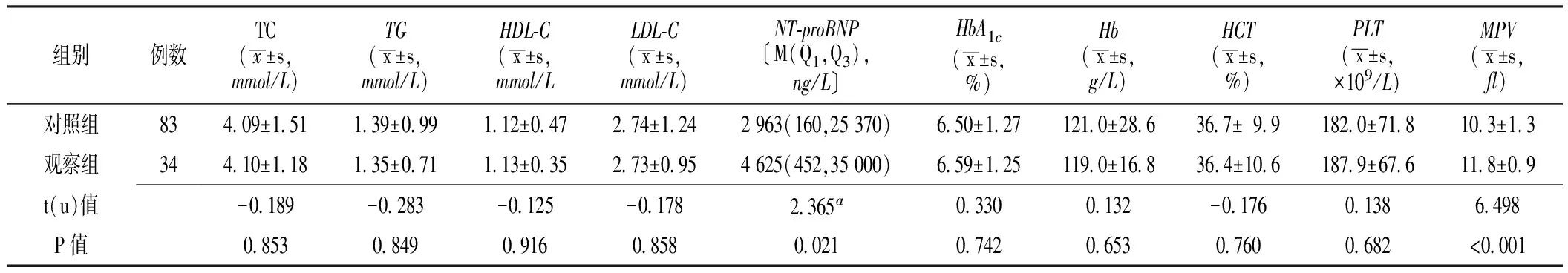
表2 两组患者实验室检查指标比较
注:TC=总胆固醇,TG=三酰甘油,HDL-C=高密度脂蛋白胆固醇,LDL-C=低密度脂蛋白胆固醇,NT-proBNP=氨基末端脑钠肽前体,HbA1c=糖化血红蛋白,Hb=血红蛋白,HCT=血细胞比容,PLT=血小板计数,MPV=平均血小板体积;a为u值
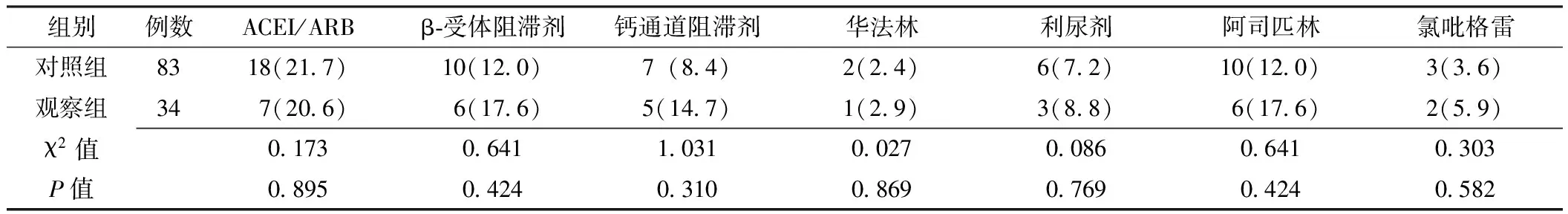
表3 两组患者入院前药物使用情况比较〔n(%)〕
注:ACEI=血管紧张素转换酶抑制剂,ARB=血管紧张素Ⅱ受体拮抗剂
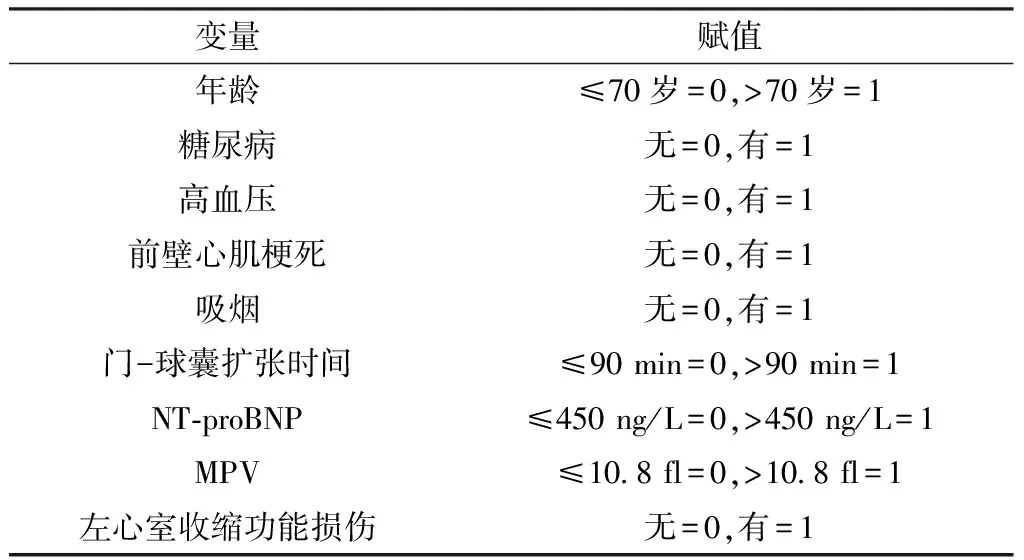
表4 变量赋值
表5 STEMI患者左心室收缩功能损伤影响因素的多因素Logistic回归分析
Table 5 Multivariate Logistic regression analysis on influencing factors of left ventricular systolic dysfuntion of patients with STEMI
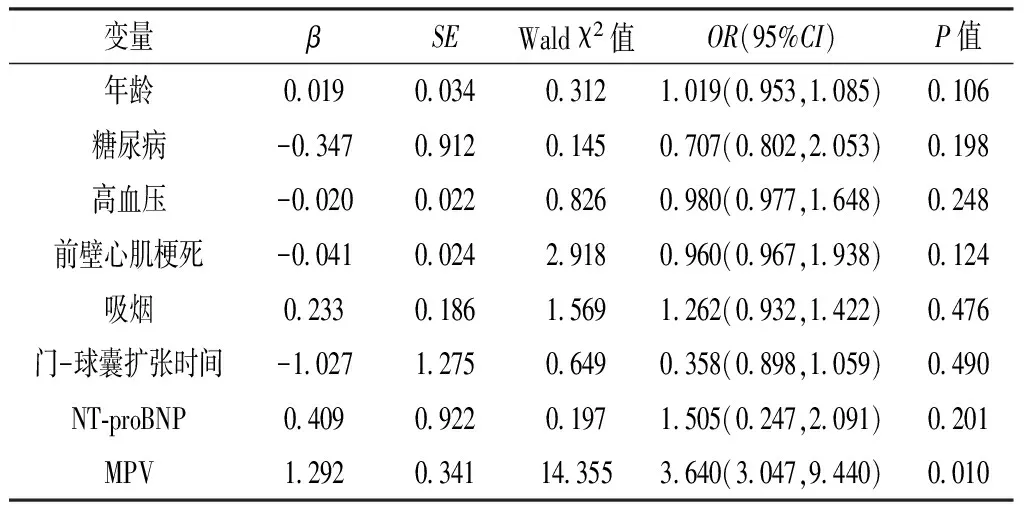
变量βSEWaldχ2值OR(95%CI)P值年龄0019003403121019(0953,1085)0106糖尿病-0347091201450707(0802,2053)0198高血压-0020002208260980(0977,1648)0248前壁心肌梗死-0041002429180960(0967,1938)0124吸烟0233018615691262(0932,1422)0476门-球囊扩张时间-1027127506490358(0898,1059)0490NT⁃proBNP0409092201971505(0247,2091)0201MPV12920341143553640(3047,9440)0010
3 讨论
近年来,国内外有关PLT及MPV的研究报道日益增多,但MPV与左心室收缩功能关系的研究较少。MPV是血细胞分析中的一个重要指标,其参考值为9~13 fl。临床研究表明,MPV与PLT体外功能明显相关,胶原和凝血酶诱导PLT聚集速度及程度与MPV呈正相关,且血小板活性可以预测心血管疾病发生风险[9]。目前,临床上检测血小板活性的方法较多,如血栓弹力图、血小板功能分析仪等,但以上方法均存在费用昂贵、耗时长等缺点。MPV属于血常规检查指标之一,具有方便获取、价格低廉等优点。正常情况下,血小板从生成到凋亡其体积保持不变,而血小板体积增大可能与STEMI、冠状动脉慢血流、冠状动脉异常扩张及侧支循环有关[10-11];除此之外,血小板体积增大还与反复发生心血管事件有关。因此,探究MPV与STEMI患者左心室收缩功能损伤的关系具有重要的临床意义。
本研究结果显示,MPV是STEMI患者左心室收缩功能损伤的独立危险因素,与以往研究结果相一致[12-14]。分析MPV增大导致左心室收缩功能损伤的原因可能如下:血小板在血栓形成的病理生理过程中具有非常重要的作用,血小板体积已成为血小板活性的重要标志,MPV增大的血小板含有更多活性物质,进而促进血栓形成、加重血管收缩及痉挛,从而扩大心肌缺血范围、延长心肌缺血时间,最终导致心脏收缩功能损伤。因此,减小MPV对改善STEMI患者左心室收缩功能可能有益。
综上所述,MPV增大与STEMI患者左心室收缩功能损伤有关。但本研究为回顾性研究,资料收集有限,存在一定偏移,未来尚需要多中心、大规模前瞻性研究进一步探讨MPV与STEMI患者左心室收缩功能损伤的因果关系。
作者贡献:黄震浩进行试验设计、资料收集整理、撰写论文、成文并对文章负责;范成辉进行质量控制及审校。
本文与任何个人或团体无利益冲突。
[1]ACIKGOZ N,ERMIS N,YAGMUR J,et al.The evaluation of mean platelet volume levels in patients with idiopathic and ischemic cardiomyopathy:an observational study[J].Anadolu Kardiyol Derg,2011,11(7):595-599.DOI:10.5152/akd.2011.161.
[2]ZHENG Y G,YANG T,XIONG C M,et al.Platelet distribution width and mean platelet volume in idiopathic pulmonary arterial hypertension[J].Heart Lung Circ,2015,24(6):566-572.DOI:10.1016/j.hlc.2014.11.025.
[3]ELBASAN Z,GUR M,SAHIN D Y,et al.Mean platelet volume and abnormal left ventricle geometric patterns in patients with untreated essential hypertension[J].Platelets,2013,24(7):521-527.DOI:10.3109/09537104.2012.738839.
[4]ACAR Z,AGA M T,KIRIS A,et al.Mean platelet volume on admission is associated with further left ventricular functions in primary PTCA patients[J].Eur Rev Med Pharmacol Sci,2012,16(11):1567-1569.
[5]FUJITA S,TAKEDA Y,KIZAWA S,et al.Platelet volume indices are associated with systolic and diastolic cardiac dysfunction,and left ventricular hypertrophy[J].BMC Cardiovasc Disord,2015,15:52.DOI:10.1186/s12872-015-0047-8.
[6]O′GARA P T,KUSHNER F G,ASCHEIM D D,et al.2013 ACCF/AHA guideline for the management of ST-elevation myocardial infarction:executive summary:a report of the American College of Cardiology Foundation/American HeartAssociation Task Force on Practice Guidelines:developed in collaboration with the AmericanCollege of Emergency Physicians and Society for Cardiovascular Angiography and Interventions[J].Catheter Cardiovasc Interv,2013,82(1):E1-27.DOI:10.1002/ccd.24776.
[7]ANDERSON J L,ADAMS C D,ANTMAN E M,et al.2012 ACCF/AHA focused update incorporated into the ACCF/AHA 2007 guidelines for themanagement of patients with unstable angina/non-ST-elevation myocardial infarction:a report of the American College of Cardiology Foundation/American Heart Association Task Force onPractice Guidelines[J].J Am Coll Cardiol,2013,61(23):e179-347.DOI:10.1016/j.jacc.2013.01.014.
[8]YAZICI H U,POYRAZ F,SEN N,et al.Relationship between mean platelet volume and left ventricular systolic function in patients with metabolic syndrome and ST-elevation myocardial infarction[J].Clin Invest Med,2011,34(6):E330.
[9]DEMIR S,AVSAR M K,KARAKAYA Z,et al.Increased mean platelet volume is associated with coronary artery ectasia[J].Postepy Kardiol Interwencyjnej,2013,9(3):241-245.DOI:10.5114/pwki.2013.37502.
[10]DURAN M,GUNEBAKMAZ O,UYSAL O K,et al.Relation between mean platelet volume and coronary collateral vessels in patients with acute coronary syndromes[J].J Cardiol,2013,61(4):295-298.DOI:10.1016/j.jjcc.2012.12.011.
[11]BERGOLI L C C,CASTANHO E S,GONÇALVES E C,et al.Mean platelet volume as a predictor of major cardiovascular outcomes and final coronary flow in patients undergoing primary percutaneous coronary intervention[J].Rev Bras Cardiol Invasiva,2014,22(3):430-442.
[12]ÖZLÜ M F,ÖZTÜRK S,AYHAN S S,et al.Predictive value of mean platelet volume in young patients with -ST-segment elevation acute coronary syndromes:a retrospective observational study[J].Anadolu Kardiyol Derg,2013,13(1):57-61.DOI:10.5152/akd.2013.007.
[13]AZAB B,TORBEY E,SINGH J,et al.Mean platelet volume/platelet count ratio as a predictor of long-term mortality after -ST-elevation myocardial infarction[J].Platelets,2011,22(8):557-566.DOI:10.3109/09537104.2011.584086.
[14]YILMAZ M B,CIHAN G,GURAY Y,et al.Role of mean platelet volume in triagging acute coronary syndromes[J].J Thromb Thrombolysis,2008,26(1):49-54.
(本文编辑:谢武英)
Relationship between Mean Platelet Volume and Left Ventricular Systolic Function of Patients with ST-segment Elevation Myocardial Infarction
HUANGZhen-hao,FANCheng-hui
DepartmentofCardiovascularMedicine,ShanghaiEastHospital,TongjiUniversitySchoolofMedicine,Shanghai200120,ChinaCorrespondingauthor:FANCheng-hui,E-mail:fchman@163.com
Objective To explore the relationship between mean platelet volume(MPV)and left ventricular systolic function of patients with ST-segment elevation myocardial infarction.Methods From 2014-10-01 to 2016-05-01,a total of 117 first-visit patients with ST-segment elevation myocardial infarction were selected in the Department of Cardiology,Shanghai East Hospital,and they were divided into control group(without left ventricular systolic function damage,n=83)and observation group(with left ventricular systolic function damage,n=34)according to the incidence of left ventricular systolic function damage.Clinical data of the two groups was retrospectively analyzed,including general information,laboratory examination results and drugs usage before admission,and the influencing factors of left ventricular systolic function of patients with ST-segment elevation myocardial infarction was analyzed by multivariate Logistic regression analysis.Results No statistically significant differences of gender,waistline,incidence of diabetes,hypertension,hyperlipemia,anterior myocardial infarction or angina pectoris before myocardial infarction,smoking rate,duration between attack and admission,or duration between door-balloon expansion was found between the two groups(P>0.05),while age of observation group was statistically significantly older than that of control group(P<0.05).No statistically significant differences of TC,TG,HDL-C,LDL-C,HbA1c,Hb,haematocrit or PLT was found between the two groups(P>0.05);NT-proBNP of observation group was statistically significantly higher than that of control group,meanwhile MPV of observation group was statistically significantly larger than that of control group(P<0.05).No statistically significant differences of proportion of patients using ACEI/ ARB,using β-blockers,using calcium channel blockers,using warfarin,using diuretic,using aspirin or using clopidogrel was found between the two groups(P>0.05).Multivariate Logistic regression analysis results showed that,MPV was the independent risk factor of left ventricular systolic function damage of patients with ST-segment elevation myocardial infarction 〔OR=3.640,95%CI(3.047,9.440),P<0.05〕.Conclusion Increase of MPV is correlated with left ventricular systolic function damage of patients with ST-segment elevation myocardial infarction.
Myocardial infarction;Mean platelet volume;Left ventricular systolic function
范成辉,E-mail:fchman@163.com
R 542.22
A
10.3969/j.issn.1008-5971.2017.02.006
2016-11-15;
2017-02-06)
黄震浩,范成辉.平均血小板体积与ST段抬高型心肌梗死患者左心室收缩功能的关系研究[J].实用心脑肺血管病杂志,2017,25(2):22-25.[www.syxnf.net]
HUANG Z H,FAN C H.Relationship between mean platelet volume and left ventricular systolic function of patients with ST-segment elevation myocardial infarction[J].Practical Journal of Cardiac Cerebral Pneumal and Vascular Disease,2017,25(2):22-25.
200120上海市,同济大学附属东方医院心内科
