重型颅脑创伤合并非腹源性肠梗阻24例临床分析
2017-03-29王伟王博姚鑫
王伟 王博 姚鑫
·临床研究·
重型颅脑创伤合并非腹源性肠梗阻24例临床分析
王伟 王博 姚鑫
目的探讨重型颅脑创伤合并非腹源性肠梗阻临床治疗方法。方法共48例重型颅脑创伤患者中24例合并非腹源性肠梗阻,其中3例(12.50%)行开颅血肿清除术、5例(20.83%)行开颅血肿清除术+去骨瓣减压术、16例(66.67%)予保守治疗,均予胃肠减压和肠外营养支持治疗;24例未合并非腹源性肠梗阻,其中4例(16.67%)行开颅血肿清除术、6例(25%)行开颅血肿清除+去骨瓣减压术、14例(58.33%)予保守治疗,均予肠内营养支持治疗。分别于治疗后10和20 d检测血红蛋白、白蛋白和前白蛋白表达变化。结果与对照组相比,观察组患者血红蛋白(P=0.008)、白蛋白(P=0.002)、前白蛋白(P=0.031)水平均降低;与治疗后10 d相比,治疗后20 d血红蛋白(P=0.003)、白蛋白(P=0.000)、前白蛋白(P=0.005)水平均降低。结论早期诊断并及时治疗重型颅脑创伤合并非腹源性肠梗阻,可以有效缓解肠梗阻症状,有利于早期肠内营养支持,提高患者康复能力。
脑损伤;肠梗阻;颅骨切开术;胃肠外营养,全;肠道营养
颅脑创伤(TBI)合并非腹源性肠梗阻在神经外科较为少见,但其影响早期肠内营养的实施,延缓脑组织及其他脏器的修复,严重者甚至危及生命[1],因此,早期发现、及时干预即显得至关重要。天津市环湖医院2010年1月-2015年12月共诊断与治疗24例重型颅脑创伤(sTBI)合并非腹源性肠梗阻患者,经积极治疗后均获得较为满意的疗效,现总结报告如下。
资料与方法
一、临床资料
1.纳入与排除标准(1)重型颅脑创伤的诊断符合以下标准:年龄≥16岁,有明确的颅脑创伤史,入院时呈昏迷状态,Glasgow昏迷量表(GCS)评分≤8分[2]。(2)肠梗阻的诊断符合以下标准:清醒患者出现腹痛腹胀、排气排便停止症状,腹部散在轻压痛伴肠鸣音减弱或消失;神志不清患者无腹痛腹胀主诉,但查体可见腹部膨隆,腹部张力较大伴肠鸣音减弱或消失,并于出现肠梗阻症状与体征后24 h内经立位腹部X线或CT证实。(3)排除标准:颅脑创伤前存在颅内器质性病变;入院时处于镇静或麻醉状态;既往有肠梗阻慢性和多次反复急性发作病史;腹腔手术、腹部创伤、腹腔脏器出血、腹腔内异物或腹部炎症病史而不能排除粘连性肠梗阻;持续昏迷,肠梗阻症状不缓解,并于入院后20 d内死亡。(4)本研究经天津市环湖医院道德伦理委员会审核批准,所有患者或其家属均知情同意并签署知情同意书。
2.一般资料(1)重型颅脑创伤合并非腹源性肠梗阻组(观察组):24例,男性16例,女性8例;年龄36~79岁,平均(54.63±15.15)岁;受伤至入院时间1~30 h,中位时间8.00(5.50,14.50)h;致伤原因分别为车祸伤16例(66.67%),高处坠落伤3例(12.50%),摔伤5例(20.83%);入院时GCS评分3~5分8例(33.33%),6~8分16例(66.67%);入院后头部CT显示,颅内血肿18例(75%),弥漫性轴索损伤4例(16.67%),脑干损伤2例(8.33%);3例(12.50%)行开颅血肿清除术,5例(20.83%)行开颅血肿清除术+去骨瓣减压术,16例(66.67%)予以保守治疗。(2)对照组:选择同期在我院神经外科住院治疗的未合并肠梗阻的24例单纯重型颅脑创伤患者,男性15例,女性9例;年龄25~78岁,平均(51.83± 16.03)岁;受伤至入院时间2~23 h,中位时间8.50(6.00,12.75)h;致伤原因分别为车祸伤18例(75%),高处坠落伤2例(8.33%),摔伤4例(16.67%);入院时GCS评分3~5分者7例(29.17%),6~8分17例(70.83%);入院后头部CT显示,颅内血肿19例(79.17%),弥漫性轴索损伤3例(12.50%),脑干损伤2例(8.33%);4例(16.67%)行开颅血肿清除术,6例(25%)行开颅血肿清除术+去骨瓣减压术,14例(58.33%)予保守治疗。两组患者一般资料比较,差异无统计学意义(均P>0.05,表1),具有可比性。

表1 两组患者一般资料的比较Table 1.Comparison of general data between 2 groups
二、研究方法
1.颅脑创伤的治疗患者入院后根据具体病情制定相应治疗方案,存在硬膜下血肿、脑挫裂伤、颅内血肿占位效应明显致颅内高压和脑疝形成的患者,予开颅血肿清除术,若清除血肿或挫伤脑组织后仍有明显脑肿胀,同时予去骨瓣减压术;颅内血肿占位效应不明显,无明显中线移位,侧裂和环池清晰,无进行性颅内高压和脑疝形成的患者,予脱水降低颅内压、止血、抑酸、补液等对症支持治疗。
2.肠梗阻的治疗(1)观察组:肠梗阻一经明确诊断,立即予禁食水、静脉泵持续泵注生长抑素、留置鼻胃管胃肠减压、反复灌肠通便、予针对需氧菌和厌氧菌的抗生素、补液、纠正水电解质和酸碱平衡紊乱、补充血容量等治疗,禁食水期间行肠外营养支持。本组有19例患者治疗后7 d内腹痛腹胀症状逐渐缓解,排气排便恢复,此后3 d内过渡为肠内营养支持;余5例患者经上述对症治疗后5 d[3]仍无排气排便,胃肠减压液日益增多,腹痛腹胀症状进行性加重,复查腹部X线显示肠腔高度膨胀,液平面增宽、不消失,遂行胃镜下肠梗阻导管置入术,术后持续负压吸引,均于术后3 d内腹痛腹胀症状消失,并逐渐恢复排气排便,此后3 d内过渡为肠内营养支持治疗,无梗阻症状后拔除肠梗阻导管。(2)对照组:均予肠内营养支持治疗,若发生腹胀、腹泻、胃潴留、误吸等并发症,减慢输注速度或改行肠外营养支持,症状改善后再过渡为肠内营养支持。
表2 两组患者治疗后10和20 d血红蛋白、白蛋白和前白蛋白水平的比较Table 2.Comparison of Hb,ALB and PA level between 2 groups 10 and 20 d after treatment
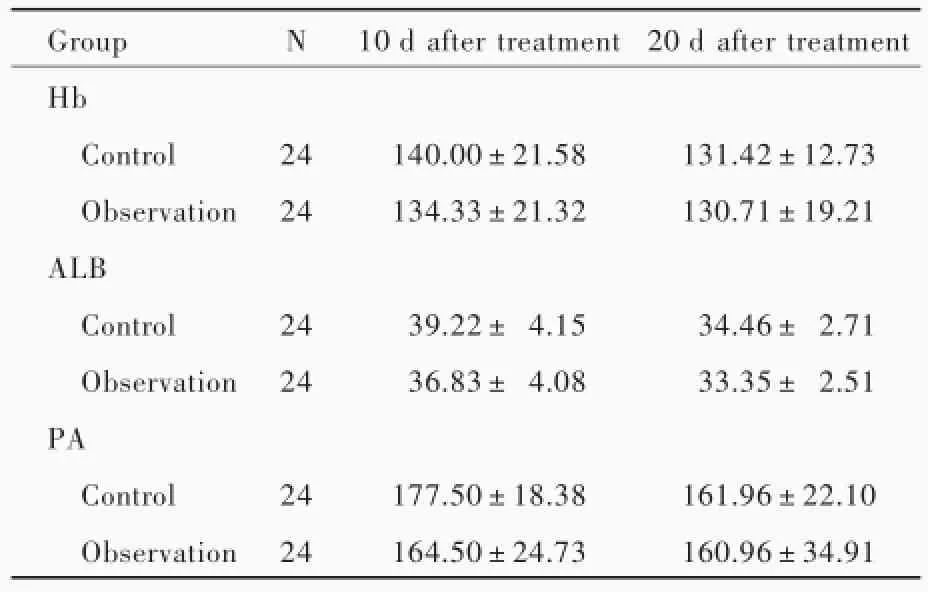
表2 两组患者治疗后10和20 d血红蛋白、白蛋白和前白蛋白水平的比较Table 2.Comparison of Hb,ALB and PA level between 2 groups 10 and 20 d after treatment
Hb,hemoglobin,血红蛋白;ALB,albumin,白蛋白;PA,prealbumin,前白蛋白。The same for table below
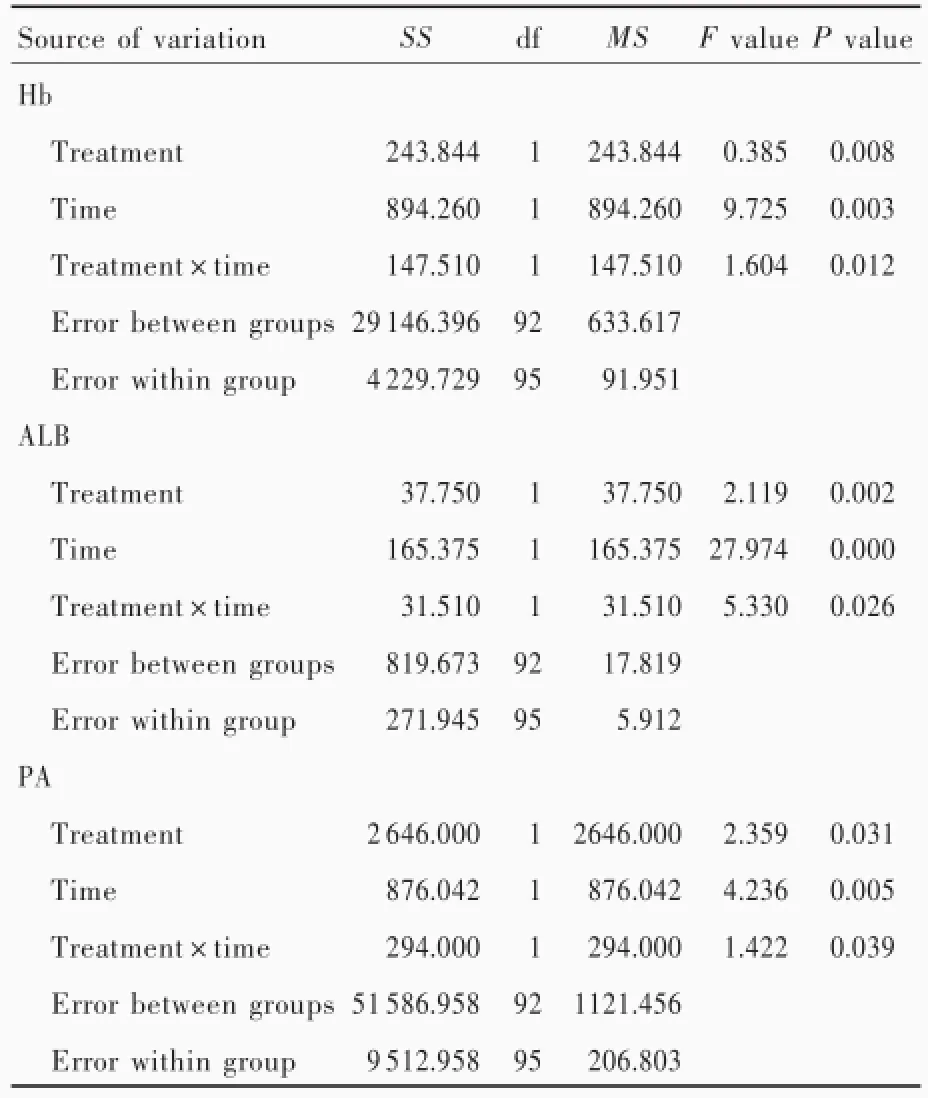
表3 两组患者治疗后10和20 d血红蛋白、白蛋白和前白蛋白的重复测量设计的方差分析表Table 3.ANOVA of repeated measurement design for Hb,ALB and PA level between control group and observation group 10 and 20 d after treatment
3.评价指标两组患者于治疗后10和20 d检测血红蛋白、白蛋白和前白蛋白表达变化。
4.统计分析方法采用SPSS 18.0统计软件进行数据处理与分析。计数资料以相对数构成比(%)或率(%)表示,采用χ2检验。呈正态分布的计量资料以均数±标准差表示,采用重复测量设计的方差分析,两两比较行LSD-t检验;呈非正态分布的计量资料以中位数和四分位数间距[M(P25,P75)]表示,采用Mann-Whitney U检验。以P≤0.05为差异具有统计学意义。
结果
与对照组相比,观察组患者血红蛋白(P= 0.008)、白蛋白(P=0.002)、前白蛋白(P=0.031)水平均降低且差异有统计学意义;与治疗后10 d相比,治疗后20 d血红蛋白(P=0.003)、白蛋白(P= 0.000)、前白蛋白(P=0.005)水平均降低且差异有统计学意义(表2,3)。
讨论
颅脑创伤后或手术后机体处于应激状态,体内儿茶酚胺、胰高血糖素、糖皮质激素等表达上调,使机体处于高分解代谢状态,能量消耗增加,蛋白质分解增加致负氮平衡,导致机体免疫力下降,延缓脑组织及其他脏器的修复,易发生感染等并发症,使病残率和病死率升高[4-6]。如果颅脑创伤后早期给予足够的营养支持,对维持机体正常代谢、预防与治疗创伤后早期代谢紊乱和急性期低蛋白血症、减轻继发性脑损伤具有重要意义[7-8]。Dhandapani等[9]研究显示,颅脑创伤早期予营养支持治疗,可以显著降低病死率和不良预后发生率,并有助于降低感染发生率。
研究显示,重型颅脑创伤后经下丘脑-垂体-肾上腺(HPA)轴、脑-肠肽轴、延髓迷走神经中枢和细胞因子途径对胃肠道动力造成影响,表现为胃肠蠕动抑制、胃排空延迟和食管下段括约肌张力下降,出现胃潴留增加、食管反流、腹胀、腹泻、呕吐,严重者可以发生肠梗阻[10-11]。肠梗阻导致消化液在肠道内积聚,造成大量体液和电解质丢失,梗阻部位肠腔内细菌增多、肠黏膜破坏,使肠道细菌异位和毒素吸收,导致细菌感染、中毒,甚至休克,同时阻碍早期肠内营养的实施,严重影响患者营养代谢,不利于康复[12-13]。因此,尽快恢复重型颅脑创伤患者胃肠功能是防止胃肠功能衰竭、减少感染并发症和改善预后的关键环节[14]。
对于颅脑创伤合并肠梗阻患者,早期诊断、及时干预是关键。清醒患者均有腹痛腹胀、排气排便停止症状,伴肠鸣音减弱或消失;神志不清患者无腹痛腹胀主诉,但查体可见腹部膨隆,伴肠鸣音减弱或消失。本研究肠梗阻患者均于出现肠梗阻症状与体征24小时内经立位腹部X线和CT证实诊断,并排除腹部术后粘连、肿瘤压迫等机械性梗阻因素。
降低肠腔内压力、减少胃肠液分泌、减少梗阻以上肠腔内液体和气体积聚、改善局部血液循环是治疗肠梗阻的关键[15]。因此,本研究肠梗阻患者一经明确诊断即予生长抑素持续静脉泵注,减少胃酸和胆汁分泌,并通过鼻胃管进行胃肠减压,抽出积聚在梗阻近端的气体和液体,降低肠腔内压力,改善肠壁血液循环,减轻全身中毒症状。然而,目前采用的鼻胃管长度较短,难以到达Treitz韧带以下,仅能吸出胃部和小肠上段的气体和液体,对于小肠中低位潴留的气体和液体,难以有效吸出,导致此类肠梗阻不能有效缓解[16-17]。近年来,肠梗阻导管的临床应用,为此类患者提供有效治疗方法。经鼻型肠梗阻导管全长3 m,可以随肠蠕动前进至梗阻部位,依靠负压抽吸肠内容物,减轻肠腔内压力,减轻肠壁水肿,促进肠壁血运恢复,恢复肠蠕动[18-20]。本研究观察组有5例患者肠梗阻症状持续未缓解,均于置入肠梗阻导管72小时内逐渐恢复排气排便,肠梗阻症状解除,显示出其独特优势。临床实践中为避免误吸,肠梗阻导管应于患者清醒状态下经胃镜下直视置入,限制其在昏迷合并肠梗阻患者中的应用。进行胃肠减压的同时,应及时大量补液,并配合应用针对需氧菌和厌氧菌的抗生素,以防止肠道菌群过度繁殖、菌群失调、细菌异位[21]。肠梗阻症状解除前,经静脉途径予营养支持治疗,待排气排便恢复后,逐步过渡为肠内营养支持[22]。
由于颅脑创伤应激期机体的高消耗,且肠梗阻阻碍早期肠内营养支持的实施,故观察组患者血红蛋白、白蛋白和前白蛋白水平均低于对照组;经积极干预,患者均可早期恢复胃肠道功能并予肠内营养支持治疗,治疗后20天血红蛋白、白蛋白和前白蛋白水平均低于治疗后10天。
综上所述,重型颅脑创伤合并非腹源性肠梗阻经早期诊断并及时干预,可以早期恢复胃肠道功能并逐渐过渡为肠内营养支持,有利于改善患者营养代谢,为颅脑创伤患者的早期康复打下基础。
[1]Liu SC,Chen XL,Huang JB,Zhang XJ,Yang JX,Xie XS. Research of related factors for craniocerebral injury with non ventral intestinal obstruction.Gannan Yi Xue Yuan Xue Bao, 2003,23:282-285[.刘胜初,陈晓雷,黄建斌,章雄军,杨建雄,谢贤生.颅脑损伤后并发非腹源性肠梗阻相关因素研究.赣南医学院学报,2003,23:282-285.]
[2]Galgano M,Toshkezi G,Qiu X,Russell T,Chin L,Zhao L. Traumatic brain injury:current treatment strategies and future endeavors.Cell Transplant,2016[.Epub ahead of print]
[3]Tanaka S,Yamamoto T,Kubota D,Matsuyama M,Uenishi T, Kubo S,Ono K.Predictive factors for surgical indication in adhesive small bowel obstruction.Am J Surg,2008,196:23-27.
[4]Zheng H,Huang Y,Shi Y,Chen W,Yu J,Wang X.Nutrition status,nutrition support therapy,and food intake are related to prolonged hospital stays in China:results from the Nutrition Day 2015 Survey.Ann Nutr Metab,2016,69(3/4):215-225.
[5]Ma FG,Liu ZF,Bao HP.Effect of enteral nutrition support therapy on the prognosis of post-operative patients with severe traumatic brain injury.Zhongguo Xian Dai Shen Jing Ji Bing Za Zhi,2007,7:536-539[.马福贵,刘泽飞,保红平.肠内营养支持治疗对重型颅脑创伤手术后患者预后的影响.中国现代神经疾病杂志,2007,7:536-539.]
[6]Yu Y,Zhang LY,Yan H.Research progress of early rehabilitation therapy on severe traumatic brain injury. Zhongguo Xian Dai Shen Jing Ji Bing Za Zhi,2014,14:548-551.[于洋,张琳瑛,闫华.重型颅脑创伤早期康复治疗研究进展.中国现代神经疾病杂志,2014,14:548-551.]
[7]Li Z,Wang H,Yang XF.Nutrition support treatment in patients with craniocerebral trauma.Zhonghua Chuang Shang Za Zhi, 2015,31:408-411[.李赵,王浩,杨小锋.颅脑创伤患者的营养支持治疗.中华创伤杂志,2015,31:408-411.]
[8]Zhang F,Meng ZP.Clinical observation of early enteral nutrition therapy for patients with severe traumatic brain injury. Zhongguo Xian Dai Shen Jing Ji Bing Za Zhi,2014,14:350-352.[张锋,孟兆朋.重型颅脑创伤患者早期肠内营养支持治疗的临床观察.中国现代神经疾病杂志,2014,14:350-352.]
[9]Dhandapani S,Dhandapani M,Agarwal M,Chutani AM, Subbiah V,Sharma BS,Mahapatra AK.The prognostic significance of the timing of total enteral feeding in traumatic brain injury.Surg Neurol Int,2012,3:31.
[10]Ott L,Young B,Phillips R,McClain C,Adams L,Dempsey R, Tibbs P,Ryo UY.Altered gastric emptying in the head-injured patient:relationship to feeding intolerance.J Neurosurg,1997, 74:738-742.
[11]McArthur CJ,Gin T,McLaren IM,Critchley JA,Oh TE.Gastric emptying following brain injury:effects of choice of sedation and intracranial pressure.Intensive Care Med,1995,21:573-576.
[12]Klausner JM,Gutman M,Rozin RR.Pathophysiology of intestinal obstruction:innovations.Harefuah,1990,118:700-704.
[13]Parthasarathy S,Sripriya R,Krishnaveni N.Anesthetic management of intestinal obstruction:a postgraduate educational review.Anesth Essays Res,2016,10:397-401.
[14]Krakau K,Hansson A,Karlsson T,de Boussard CN,Tengvar C, Borg J.Nutritional treatment of patients with severe traumatic brain injury during the first six months after injury.Nutrition, 2007,23:308-317.
[15]Hor T,Paye F.Diagnosis and treatment of an intestinal obstruction.Rev Infirm,2016,217:19-21.
[16]Declercq D,Van Biervliet S,Robberecht E.Nutrition and pancreatic enzyme intake in patients with cystic fibrosis with distal intestinal obstruction syndrome.Nutr Clin Pract,2015,30:134-137.
[17]Takayama H,Yashio A,Kamijo H,Okamoto K.Ileus and intestinal obstruction.Nihon Rinsho,2013,71:1027-1030.
[18]Ishizuka M,Nagata H,Takagi K,Kubota K.Transnasal fine gastrointestinal fiberscope-guided long tube insertion for patients with small bowel obstruction.J Gastrointest Surg,2009, 13:550-554.
[19]Cui H,Jiang X,Li H.Adhesive small-bowel obstruction treatment using internal intestinal splinting with a nasointestinal ileus tube.Minerva Chir,2015,70:327-330.
[20]Chen XL,Ji F,Lin Q,Chen YP,Lin JJ,Ye F,Yu JR,Wu YJ. A prospective randomized trial of transnasal ileus tube vs nasogastric tube for adhesive small bowel obstruction.World J Gastroenterol,2012,18:1968-1974.
[21]Debnath D,Ogedegbe AJ.Letter 1:clinicoradiological score for predicting the risk of strangulated small bowel obstruction.Br J Surg,2010,97:1119-1125.
[22]Assenza M,De Gruttola I,Rossi D,Castaldi S,Falaschi F, Giuliano G.Adhesions small bowel obstruction in emergency setting:conservative or operative treatment?G Chir,2016,37:145-149.
Clinical analysis on the treatment of 24 cases of severe traumatic brain injury with non ventral intestinal obstruction
WANG Wei,WANG Bo,YAO Xin
Department of Neurosurgery,Tianjin Huanhu Hospital,Tianjin 300350,China Corresponding author:WANG Wei(Email:wangwei_735@126.com)
ObjectiveTo discuss the clinical treatment for severe traumatic brain injury(sTBI) with non ventral intestinal obstruction.MethodsA total of 48 patients with sTBI were enrolled in this study,including 24 with(observation group)and 24 without(control group)non ventral intestinal obstruction.Among 24 patients with non ventral intestinal obstruction,3 cases(12.50%)were treated by craniotomy evacuation of hematoma,5 cases(20.83%)were treated by craniotomy evacuation of hematoma and decompressive craniectomy,and 16 cases(66.67%)were treated by conservative treatment.They were all treated by gastrointestinal decompression and parenteral nutrition.Among 24 patients without non ventral intestinal obstruction,4 cases(16.67%)were treated by craniotomy evacuation of hematoma,6 cases (25%)were treated by craniotomy evacuation of hematoma and decompressive craniectomy,and 14 cases (58.33%)were treated by conservative treatment.They were all treated by enteral nutrition.Hemoglobin (Hb),albumin(ALB)and prealbumin(PA)were detected 10 and 20 d after treatment.ResultsCompared with control group,the level of Hb(P=0.008),ALB(P=0.002)and PA(P=0.031)were significantly reduced in observation group.Compared with 10 d after treatment,the level of Hb(P=0.003),ALB(P= 0.000)and PA(P=0.005)were significantly reduced 20 d after treatment.ConclusionsEarly diagnosis and timely treatment for non ventral intestinal obstruction in patients with severe traumatic brain injury could effectively relieve the symptoms of intestinal obstruction,and is favorable to early enteral nutrition,so as to enhance the patients'recovery.
Brain injuries;Intestinal obstruction;Craniotomy;Parenteral nutrition,total; Enteral nutrition
2016-12-23)
10.3969/j.issn.1672-6731.2017.01.012
300350天津市环湖医院神经外科
王伟(Email:wangwei_735@126.com)