Device-associated healthcare-associated infection in intensive care unit of a university hospital in China: a descriptive study
2017-01-11-,-,-
-, -, -
( Dongguan Hospital of Traditional Chinese Medicine, Guangzhou University of Chinese Medicine, Dongguan 523000, China)
Device-associated healthcare-associated infection in intensive care unit of a university hospital in China: a descriptive study
WANGJian-cong,MOQi-jun,QIKe-xin
(DongguanHospitalofTraditionalChineseMedicine,GuangzhouUniversityofChineseMedicine,Dongguan523000,China)
Objective To identify the occurrence and microorganism profile of device-associated healthcare-associa-ted infections (DA-HAIs) in the intensive care unit (ICU) of a university hospital in China.Methods From Janua-ry 1 to November 30, 2015, patients admitted to the ICU of a university hospital in China for more than 48 hours were performed prospective descriptive study. DA-HAIs were defined according to the criteria of the Centers for Disease Control and Prevention (CDC) of U.S., descriptive statistical analysis was performed.Results Of 254 patients admitted to ICU, the overall incidence of DA-HAIs was 15.35%, with 10.23 cases of DA-HAIs per 1 000 ICU-days; the incidence of ventilator-associated pneumonia (VAP), catheter-associated urinary tract infection (CAUTI), and central line-associated bloodstream infection (CLABSI) were 7.05 per 1 000 ventilator-days, 4.91 per 1 000 urinary catheter-days, and 3.22 per 1 000 central line-days, respectively. The main infection site was lower respiratory tract, accounting for 48.27%, followed by bloodstream system(27.59%), urinary tract(22.99%), and gastrointestinal tract(1.15%). The major isolated microorganism wasAcinetobacterbaumannii(21.52%).Conclusion The surveillance system can identify the epidemiological status of DA-HAIs and make effective control measures to ensure the healthcare safety.
device-associated infection; catheter-associated urinary tract infection; central line-associated bloodstream infection; ventilator-associated pneumonia; healthcare-associated infection; intensive care unit; descriptive study; microorganism
[Chin J Infect Control,2016,15(12):902-906]
Introduction
DA-HAIs are principal public health problems in intensive care units (ICUs) of hospitals worldwide[1-3]. It has been reported by U.S. National Healthcare Safety Network (NHSN) and International Nosocomial Infection Control Consortium (INICC) that DA-HAIs have posed the principal threat to patients’ healthcare safety in ICUs[3,4]. Therefore, targeted surveillance is an efficient tool for monitoring and understanding the occurrence of DA-HAIs in ICUs, which is helpful for ensuring the safety of healthcare through the implementation of healthcare improvement activities.
The occurrence of DA-HAIs varies among diffe-rent studies and different parts of the world, incidence in developing countries is higher than developed countries. It has been shown that the incidence of DA-HAIs ranged from 5.3% to 14.7%, with from 6.4 to 24.9 DA-HAIs per 1 000 device-days[2,3,5-8]. U.S. National Nosocomial Infections Surveillance(NNIS)/NHSN has established standardized criteria for DA-HAIs surveillance that provides useful data as benchmark among healthcare settings to INICC[3]. However, in the resource-limited healthcare settings in developing countries, paucity of data exists regarding the epidemiological status and reports on incidence of DA-HAIs due to the lack of information surveillance system[2]. The purpose of this study is to evaluate the occurrence and epidemiological status of DA-HAIs as well as associated microorganisms in the ICU of a university hospital in China.
Methods
Studied patients
This was a prospective descriptive study on DA-HAIs in ICU at a 955-bed university hospital in China. The hospital was established in 1965, with the integrated function of medical treatment, teaching and research.
Patients who were admitted to the ICU of this hospital for more than 48 hours between January 1 and November 30, 2015 were enrolled in the study, they were followed up for 48 hours after discharged from ICU, and were eligible to be diagnosed with ICU-acquired infection within 48 hours after discharged from ICU.
Data collection
This study recorded all data which were already in the hospital information surveillance system. All DA-HAIs were defined according to the U. S. CDC criteria[9,10], which were classified as ventilator-associated pneumonia (VAP), catheter-associated urinary tract infection (CAUTI), and central line-associated bloodstream infection (CLABSI). The infection control practitioners (ICPs) performed bed-side observation and inspected patients undergoing invasive procedures twice a week, and paid close attention to patient who had a positive microbiological results and/or infection-related complications. Clinical microbiology laboratory provided microbiological identification and antimicrobial susceptibility testing results.
Patients were followed up by ICPs for 48 hours after discharged from ICU, and questionnaires for the monitoring of DA-HAIs were filled out.
Statistical analysis
All data were conducted descriptive statistical analysis using IBM SPSS Statistics 23.0.
Results
General data about DA-HAIs
A total of 254 patients who were admitted to the ICU between January 1 and November 30, 2015 were included in the study, 51 of whom developed 87 cases of HAIs, the total length of hospital stay were 3 813 days, the overall HAI rate was 20.08%, with 13.38 HAIs per 1 000 ICU-days. There were 39 cases being diagnosed as DA-HAIs, the DA-HAI case rate was 15.35%, with 10.23 cases of DA-HAIs per 1 000 ICU-days. The average disease severity (ADS) score was 4.5. The trend of HAI rate and ADS are presented in Figure 1.
Figure 1 Trend of HAI rate and ADS score in a university hospital from January to November, 2015
Among 254 ICU patients, incidence of VAP was 7.05 per 1 000 ventilator-days and utilization rate of mechanical ventilator was 59.53%; incidence of CAUTI was 4.91 per 1 000 urinary catheter-days and utilization rate of urinary catheter was 80.12% ; incidence of CLABSI was 3.22 per 1 000 central line-days and utilization rate of central line was 65.17%. DA-HAI rate and device utilization rates in January-November 2015 are shown in Table 1.

Table 1 DA-HAIs and device utilization in ICU patients in a university hospital from January to November, 2015
* Rate per 1 000 device-days=Number of DA-HAIs for specific site/the total number of specific device-days of all patients×1 000
There were 87 cases of infection among 254 ICU patients, the distribution of lower respiratory tract, bloodstream system, urinary tract, and gastrointestinal tract were 48.27%(n=42), 27.59%(n=24), 22.99%(n=20), and 1.15%(n=1) respectively,among specimens which isolated pathogens, the distribution of sputum was the highest, accounting for 41.34%, followed by blood, urine, catheter tip and peripheral blood, and ascitic fluid (Table 2).
Table 2 Distribution of microbiological culture specimens
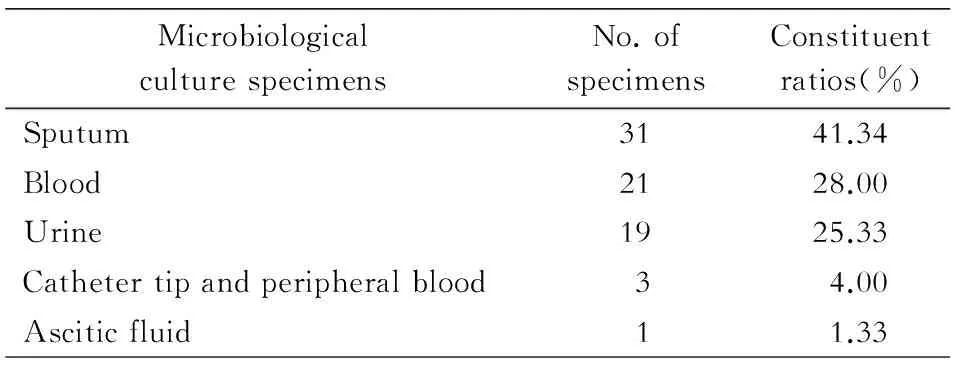
MicrobiologicalculturespecimensNo.ofspecimensConstituentratios(%)Sputum3141.34Blood2128.00Urine1925.33Cathetertipandperipheralblood34.00Asciticfluid11.33
Microbiological profile
A total of 79 pathogenic strains were isolated, gram-negative bacteria, gram-positive bacteria, and fungi accounted for 63.29%, 21.52% and 15.19% respectively. Among 79 pathogenic strains, 27(34.18%) were multidrug-resistant organisms (MDROs).Acinetobacterbaumannii(A.baumannii) was the most commonly isolated microorga-nism related to HAIs in ICU in this university hospital, accounting for 21.52%, 88.24% of which were multidrug-resistant strains. Distribution of pathogens causing DA-HAIs in ICU are shown in Table 3.
Discussion
The incidence of DA-HAIs was 15.35%, with 10.23 DA-HAIs per 1 000 ICU-days. This study indicated that the incidence of DA-HAIs was lower than a meta-analysis reported by Allegranzi[2]that the incidence Table 3 Distribution of pathogens causing DA-HAIs in ICU in a university hospital from January to November, 2015 and density in developing countries were 34.7% (95%CI: 23.6-47.7) and 47.9 per 1 000 ICU-days (95%CI: 36.7-59.1). However, compared with incidence of DA-HAIs reported by U.S. CDC and European CDC (ECDC), the present study is substantially higher[2]. Efforts for the prevention of DA-HAIs should be strengthened.

PathogensNo.ofstrainsConstituentratios(%)Gram-negativebacteria5063.29 Acinetobacterbaumannii1721.52 Escherichiacoli78.86 Stenotrophomonasmaltophilia78.86 Pseudomonasaeruginosa78.86 Klebsiellapneumoniae67.59 Burkholderiacenocepacia33.79 Enterobacteraerogenes11.27 Elizabethkingiameningosepticum11.27 Morganellamorganii11.27Gram-positivebacteria1721.52 Staphylococcushaemolyticus56.33 Enterococcusfaecium45.06 Enterococcusfaecalis33.79 Staphylococcusepidermidis22.53 Staphylococcushominis11.27 Staphylococcusaureus11.27 Staphylococcuscapitis11.27Fungi1215.19 Candidaalbicans911.39 Candidatropicalis22.53 Candidaglabrata11.27Total79100.00
In our study, ADS score for infection in ICU patients in January-August 2015 was significantly higher than that of the baseline status, after clinical intervention, ADS score in September-November 2015 presented a downward trend, and was lower than that of the baseline status. Therefore monitoring on ADS in ICU patients can lead to a better understanding for the dynamic change trend in DA-HAIs, and implement intervention measures to control infection under the guidance by ICPs.
Compared to incidences of CAUTI and CLABSI, VAP in the present study was a major burden and safety issue for patients in the ICU setting, the incidence of VAP was 7.05 per 1 000 ventilator-days, which was slightly higher than that of NHSN of the U. S. and German Krankenhaus Infektions Surveillance System (KISS) (ranging from 2.9 to 5.1 per 1 000 ventilator-days[2]), while was lower than incidence of INICC in Shanghai[3]. A possible explanation could be that prevention and control measures of VAP might be not sufficient. The management of DA-HAIs, especially VAP, still remains the first priority for ICU setting[11]. According to guidelines for prevention and control of VAP, it is recommend to elevate head of bed to 30o-45ofor patients with artificial airway, provide daily regular oral care, reduce the colonization of pathogens, timely treat water retention in ventilator pipes, adopt closed sputum suction method, perform sterile sputum suction, conduct hand hygiene among health care workers, and perform daily assessment for removing respirator as soon as possible[12].
The major infection site in the ICU setting was lower respiratory tract, resistance rate of drug-resistantA.baumanniiwas 88.24%, which was consistent with the other scientific literatures[13]. Inchai indicated that the lack of antimicrobial susceptibility testing could result in a high mortality of patients due to treatment failure[13]. In addition, patients colonized or infected byA.baumanniiwere a source of transmission to other high risk patients through environmental contamination and health care workers. So antimicrobial susceptibility testing and homology detection between cases are recommended.
The limitation of the study is that it only provided annual monitoring data in the ICU setting, and did not make comparison with previously monitored data. Additionally, specimen size of the study was unsatisfactory and results cannot be generalized based on case findings from only one ICU setting. Multi-center targeted monitoring on DA-HAIs is recommended. However, this study has already adopted the established routine data of surveillance system in an ICU setting and recognized methods for routine evaluation on the implementation of infection control management in the hospital, all of which are very commendable. Further fortification of routine surveillance can improve the healthcare safety in ICU settings and further reduce the occurrence of DA-HAIs.
Ethical consideration
Participants were anonymous in the questionnaire, only investigators had an access to review and manage the data.
Conflict of interest
The authors declared no potential conflict of interest with respect to the research, authorship, and/or publication of this article.
Acknowledgements
We thank infection control practitioners in department of healthcare-associated infection control and health care workers in the intensive care unit in Dongguan Hospital of Traditional Chinese Medicine for supporting, and Liang Hui LIM for professional English advice.
[1] Naidu K, Nabose I, Ram S, et al. A descriptive study of nosocomial infections in an adult intensive care unit in fiji: 2011-12[J]. J Trop Med, 2014, 2014:545160.
[2] Allegranzi B, Bagheri Nejad S, Combescure C, et al. Burden of endemic health-care-associated infection in developing countries: Systematic review and meta-analysis[J]. Lancet, 2011, 377(9761):228-241.
[3] Tao L, Hu B, Rosenthal VD, et al. Device-associated infection rates in 398 intensive care units in Shanghai, China: International Nosocomial Infection Control Consortium (INICC) findings [J]. Int J Infect Dis, 2011, 15(11):e774-e780.
[4] Edwards JR, Peterson KD, Mu Y, et al. National healthcare safety network (NHSN) report: data summary for 2006 through 2008, issued December 2009[J]. Am J Infect Control, 2009, 37(10):783-805.
[5] Rosenthal VD, Maki DG, Salomao R, et al. Device-associated nosocomial infections in 55 intensive care units of 8 developing countries[J]. Ann Intern Med, 2006, 145(8):582-591.
[6] Cuellar LE, Fernandez-Maldonado E, Rosenthal VD, et al. Device-associated infection rates and mortality in intensive care units of Peruvian hospitals: Findings of the international nosocomial infection control consortium[J]. Rev Panam Salud Publica, 2008, 24(1):16-24.
[7] Kanj S, Kanafani Z, Sidani N, et al. International nosocomial infection control consortium findings of device-associated infections rate in an intensive care unit of a Lebanese university hospital[J]. J Glob Infect Dis, 2012, 4(1):15-21.
[8] Moreno CA, Rosenthal VD, Olarte N, et al. Device-associa-ted infection rate and mortality in intensive care units of 9 Colombian hospitals: findings of the International Nosocomial Infection Control Consortium[J]. Infect Control Hosp Epidemiol, 2006, 27(4):349-356.
[9] Garner JS, Jarvis WR, Emori TG, et al. CDC definitions for nosocomial infections, 1988[J]. Am J Infect Control, 1988, 16(3):128-140.
[10] Horan TC, Andrus M, Dudeck MA. CDC/NHSN surveillance definition of health care-associated infection and criteria for specific types of infections in the acute care setting[J]. Am J Infect control, 2008, 36(5):309-332.
[11] Erdem H, Inan A, Altindis S, et al. Surveillance, control and management of infections in intensive care units in Southern Europe, Turkey and Iran-a prospective multicenter point prevalence study[J]. J Infect, 2014, 68(2):131-140.
[12] Klompas M, Branson R, Eichenwald EC, et al. Strategies to prevent ventilator-associated pneumonia in acute care hospitals: 2014 update[J]. Infect Control Hosp Epidemiol, 2014, 35(8):915-936.
[13] Inchai J, Liwsrisakun C, Theerakittikul T, et al. Risk factors of multidrug-resistant, extensively drug-resistant and pandrug-resistantAcinetobacterbaumanniiventilator-associated pneumonia in a Medical Intensive Care Unit of University Hospital in Thailand[J]. J Infect Chemother, 2015, 21(8):570-574.
(本文编辑:李洁)
2016-01-06
王建聪(1983-),男(汉族), 广东省东莞市人,在读博士研究生,主要从事统计与流行病学及医院感染控制研究。
王建聪 E-mail:jiancong.wang@outlook.com
重症监护病房导管相关医院感染的目标性监测与分析
王建聪,莫绮君,祁可欣
(广州中医药大学附属东莞市中医院,广东 东莞 523000)
目的 分析某教学医院重症监护病房(ICU)导管相关医院感染及其病原微生物的情况。方法采用前瞻性调查, 对2015年1月1日—11月30日所有入住ICU>48 h的患者进行目标性监测,对侵入性操作相关医院感染病例进行分析,以美国疾病控制与预防中心(CDC)颁布的指南作为诊断依据,标准化模式进行数据收集,并采用描述性研究进行统计分析。结果2015年1—11月共监测254例ICU住院患者。导管相关医院感染(DA-HAIs)例次发病率为15.35%,例次日感染发病率为10.23‰。呼吸机相关肺炎(VAP), 导尿管相关尿路感染(CAUTI)及血管导管相关血流感染(CLABSI)发病率分别为7.05‰、4.91‰及3.22‰。ICU医院感染的主要部位为下呼吸道(48.27%), 其次为血液系统(27.59%)、泌尿系统(22.99%)及消化系统(1.15%),常见病原菌为鲍曼不动杆菌,占21.52%。结论该目标性监测系统能有效识别ICU导管相关医院感染的流行病学现状与趋势,并制定有效控制措施,从而确保医疗质量安全。
导管相关医院感染; 导尿管相关尿路感染; 血管导管相关血流感染; 呼吸机相关肺炎; 医院感染; 重症监护病房; 描述性研究; 病原微生物
R181.3+2
A
1671-9638(2016)12-0902-05
10.3969/j.issn.1671-9638.2016.12.002