Stereotactic guidance for navigated percutaneous sacroiliac joint fusion
2016-12-13DarrinLeeSungBumKimPhilipRosenthalRipulPanchalKeeKim
Darrin J. Lee, Sung-Bum Kim, Philip Rosenthal, Ripul R. Panchal, Kee D. Kim,✉
1Department of Neurological Surgery, University of California-Davis Medical Center, Sacramento, California;
2Department of Neurological Surgery, Kyung-Hee Medical Center, Seoul, Korea.
Stereotactic guidance for navigated percutaneous sacroiliac joint fusion
Darrin J. Lee1, Sung-Bum Kim2, Philip Rosenthal1, Ripul R. Panchal1, Kee D. Kim1,✉
1Department of Neurological Surgery, University of California-Davis Medical Center, Sacramento, California;
2Department of Neurological Surgery, Kyung-Hee Medical Center, Seoul, Korea.
Arthrodesis of the sacroiliac joint (SIJ) for surgical treatment of SIJ dysfunction has regained interest among spine specialists. Current techniques described in the literature most often utilize intraoperative fluoroscopy to aid in implant placement; however, image guidance for SIJ fusion may allow for minimally invasive percutaneous instrumentation with more precise implant placement. In the following cases, we performed percutaneous stereotactic navigated sacroiliac instrumentation using O-arm®multidimensional surgical imaging with StealthStation®navigation (Medtronic, Inc. Minneapolis, MN). Patients were positioned prone and an image-guidance reference frame was placed contralateral to the surgical site. O-arm®integrated with StealthStation®allowed immediate autoregistration. The skin incision was planned with an image-guidance probe. An image-guided awl, drill and tap were utilized to choose a starting point and trajectory. Threaded titanium cage(s) packed with autograft and/or allograft were then placed. O-arm®image-guidance allowed for implant placement in the SIJ with a small skin incision. However, we could not track the cage depth position with our current system, and in one patient, the SIJ cage had to be revised secondary to the anterior breach of sacrum.
sacroiliac joint, arthrodesis, technique, image guidance
Introduction
Sacroiliac joint (SIJ) pathology has been reported as the contributing factor for low back pain in 13% to 30% of patients seen in specialized spinal centers[1-3]. Recent published literature reports that 15%-30% of patients presenting with low back pain had SIJ dysfunction[4]. Additionally, up to 75% of post-lumbar fusion patients develop significant SIJ degeneration within 5 years[2,5-6].
Conservative treatment options include physical therapy, joint injections, and radiofrequency ablation[1-3,7]. For those refractory to nonsurgical treatment, surgical arthrodesis of the sacroiliac joint has regained interest among spine specialists[8-9]. In fact, a randomized controlled trial comparing minimally invasive SIJ fusion versus non-surgical management demonstrated better improvement in pain, function and quality of life with SIJ fusion[10]. As SIJ arthrodesis becomes more popular, current techniques described in the literature are still limited to intraoperative fluoroscopy to aid in implant placement. However, recent literature suggests that CT-guidance may allow for more accurate screw placement than traditional fluoroscopy[11-13]. Interpreting the images can be very challenging due to relatively unfamiliar SIJ anatomy with its deep oblique course. Many different views of the SIJ, such asanteroposterior, lateral, pelvic inlet and outlet views are utilized, but these views can be difficult to interpret and thus are not universally accepted[2,7-8].
Open procedures for SIJ fusion are associated with larger incisions and the comorbidities associated with major soft tissue dissection required for bony exposure[7-8]. Percutaneous iliosacral screw fixation, when performed accurately, is a safe and predictable technique for the treatment of disrupted sacroiliac joints[14]. In fact, minimally invasive SIJ fusion is becoming increasingly preferred over the open technique[15-16]. Stereotactic guidance for navigated percutaneous SIJ fusion allows for minimally invasive percutaneous instrumentation with more precise implant placement. We report our experience with a new percutaneous technique for SIJ arthrodesis using O-arm®multidimensional surgical imaging with StealthStation®navigation (Medtronic, Inc. Minneapolis, MN, USA).
Materials and methods
We used O-arm®multidimensional surgical imaging with StealthStation®as our stereotactic guidance system (Fig. 1A). The Bagby and Kuslich (BAK) system (Spine Tech, Inc. Minneapolis, MN, USA) or large cannulated screw system (Medtronic, Inc. Memphis, TN, USA) filled with local autograft and/or allograft were used for SIJ arthrodesis. Depending on surgeon (K.D.K.) preference and patient anatomy, SIJ arthrodesis was performed with either 1 or 2 threaded cages (cannulated screws).
Patient positioning
The procedure was performed under general anesthesia with the patient in the prone position on a radiolucent Jackson table, and the navigation camera placed at the foot of table. Both sides of the low back and lateral buttock areas were prepped (Fig. 1A) to allow for an approximately 2 cm skin incision for the fusion sideand a contralateral stab incision for the image-guided navigation system reference frame.
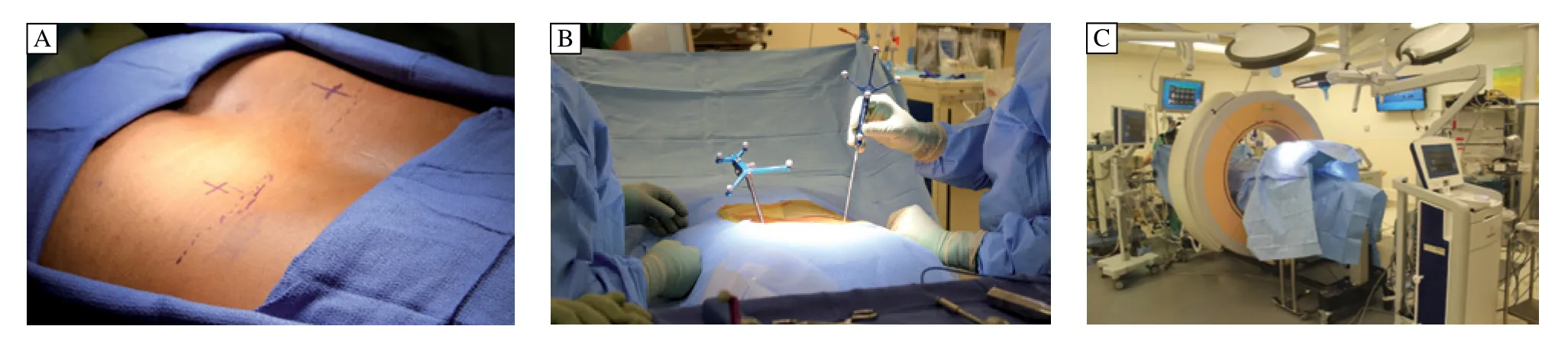
Fig. 1 Patient and O-arm positioning. A: Patient prone on padded radiolucent OR table. The bilateral hips are prepped and draped for a right SIJ fusion with the superior left iliac crest palpated and outlined with a sterile pen for navigation array instrumentation. B: Intraoperative view of the reference arc percutaneously placed on the contralateral iliac crest facing the camera digitizer at the foot of the table. C: Intraoperative position of the O-arm positioned with the cover drapes.
Reference frame placement and O-arm®imaging*
The reference frame was percutaneously secured to the contralateral ilium or sacrum after a stab skin incision was made inferior to the posterior superior iliac crest. The reference frame was adjusted so that the silver spheres faced the navigation camera, unobstructed during surgery (Fig. 1B,C). The O-arm®was positioned to image the entire SIJ to be fused by first obtaining anteroposterior and lateral scout views. 3-D image acquisition with the O-arm®provided CT style images of the SIJ. The image data were then transferred to the StealthStation®for auto-registration, and multiplanar images were displayed on the monitor.
Planning the entry point and cage placement
The navigatable instruments were registered and then the image-guided navigation probe was used to select the ideal skin incision site. Tip projection views were utilized to ensure that the intended skin incision site would accommodate the planned entry and trajectory for implant placement (Fig. 2A). A small incision, approximately 2 cm in length, was made. The fascia was incised, and using an index finger and small Cobb dissector, the muscle was split. The navigation probe was used to confirm the ideal entry point in the ilium. An image-guided awl was malleted into the ilium to create the bony entry point along the planned trajectory (Fig. 2B). A navigated tap was used to create the pilot hole for the cage (Fig. 2C).
The tip projection view was utilized to select the proper dimensions such as diameter and length of the threaded cage (Fig. 2D). Since the cage inserter was not navigatable, the cage was inserted in the tapped area without image-guidance.
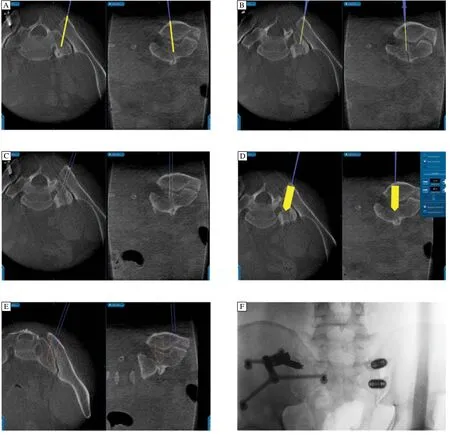
Fig. 2 Intraoperative navigation. A: Surgeon positioning the navigation probe on the skin while referring to the monitor screen for surgical planning. B: Navigation probe positioned on iliac bone to confirm the planned site for navigated awl after skin incision with confirmation of planned trajectory on the StealthStation®. C: Lining up the image-guided awl with the preoperative trajectory plan. D: Navigation monitor displaying the navigated tap (blue) and projected cage plan (yellow) based on the surgeon's hand positioning. The theoretical cage width, length and position (yellow) are shown. E: The relative positions of the second planned cage (orange and violet outlines) are entered as the surgeon positions the navigation probe (blue) over the iliac bone for the second cage placement relative to the first cage. F: After cage placement, the final O-arm spin is used to check cage placement. The intraoperative O-arm view demonstrates the reference arc on the contralateral iliac crest and two perpendicular SIJ cages.
The second cage was placed in a similar fashion just caudal to the first cage using the same skin incision. Virtual views were utilized to ensure that the cages were at an adequate distance from each other (Fig. 2E). After placement of the second cage, we palpated the ilium to confirm that the cages were flush or slightly recessed to avoid muscle irritation. The O-arm®was then used to rescan the patient prior to wound closure to confirm adequate placement of the implants (Fig. 2F).
Closure/follow-up
After proper cage placement was confirmed using the O-arm®, the reference frame was removed and that incision was closed. The surgical site incision was irrigated with antibiotic saline, fascia was re-approximated and the wound was closed in multiple layers. Patients were discharged home the same day with instructions to avoid any strenuous activity. Routine postsurgical follow-up and X-rays were also performed.
Illustrative case 1
A 52-year-old man presented with a history of lower back pain that localized to the right hip. He had under gone a diagnostic right SIJ injection that briefly improved 70% of his pain. He was most comfortable lying on his right side or bending his body to the right. Although his lumbar CT revealed L5-S1 degenerative disc changes with a left L5 pars defect, the SIJ was thought to be the primary pain generator based on examination and positive response to SIJ injection. In addition, he failed to respond to epidural steroid injections. Image-guided SIJ arthrodesis was performed and a single BAK cage was placed parallel to the SIJ. Intraoperative O-arm® was utilized for navigation as well as to check the implant position, requiring two spins (Fig. 3). The patient was discharged the same day. He had complete relief of preoperative pain and remained symptom free at 6 months.
Illustrative case 2
A 59-year-old man with a history of morbid obesity (BMI of 50) presented with lower back pain and left hip pain. He had undergone a diagnostic left SIJ injection that temporarily relieved 80% of his pain. We then performed image-guided placement of 2 threaded cages perpendicular to the SIJ (Fig. 4 A,B). After surgery, the patient reported resolution of preoperative pain but new sharp left leg pain. A postoperative lumbar CT demonstrated that the cages had breached the ventral cortical wall of the sacrum (Fig. 4C). When his new left leg pain did not improve, he was taken back to the OR for cage revision. Using the cage driver, the cages were backed out slightly (Fig. 4D). Immediately afterwards, he reported that his left leg pain had resolved, but he did note residual numbness that gradually improved.
Discussion
Initially, SIJ arthrodesis techniques were used to treat traumatic injury to the sacroiliac region(9). Techniques then evolved to treat those with SIJ-derived pain refractory to conservative treatment[1-3,7-9]. The described SIJ fusion techniques include: non-instrumented arthrodesis with bone graft, instrumented arthrodesis with or without bone graft, open anterior or posterior surgical approaches, and percutaneous instrumented arthrodesis using fluoroscopy or CT[1-3,7-9,14,17]. None, however, has been widely accepted due to a variety of limitations. Noninstrumented arthrodesis relies on the SIJ ligaments to secure stability. Arthrodesis via open anterior or posterior approaches may cause major complications such as injury to erector spinae muscle insertions, nerve roots,sacral plexus, and internal iliac vessels(3,8). Percutaneous instrumented arthrodesis requires familiarity with SIJ anatomy and intraoperative fluoroscopic interpretation[14].While studies have suggested that both open and minimally invasive SIJ fusion improve pain, minimally invasive approaches appear to result in shorter operative time, less blood loss and shorter hospital stays[18-19].

Fig. 3 Intraoperative and postoperative cage post-placement view. A: Intraoperative coronal O arm view of the parallel placed SIJ cage. B: Three month post-operative antero-posterior X-ray of the parallel placed SIJ cage (right).
O-arm®is one of the latest advances in intraoperative spinal imaging and navigation that allows for multidimensional views. Lower peri-operative morbidity using O-arm®-based navigation techniques have been reported for other spinal procedures[20-22]. Use of O-arm®as opposed to fluoroscopy permits more accurate implant placementin spine surgery[23-29]. However, there are reported longer operative times with the use of O-arm®[26-27].
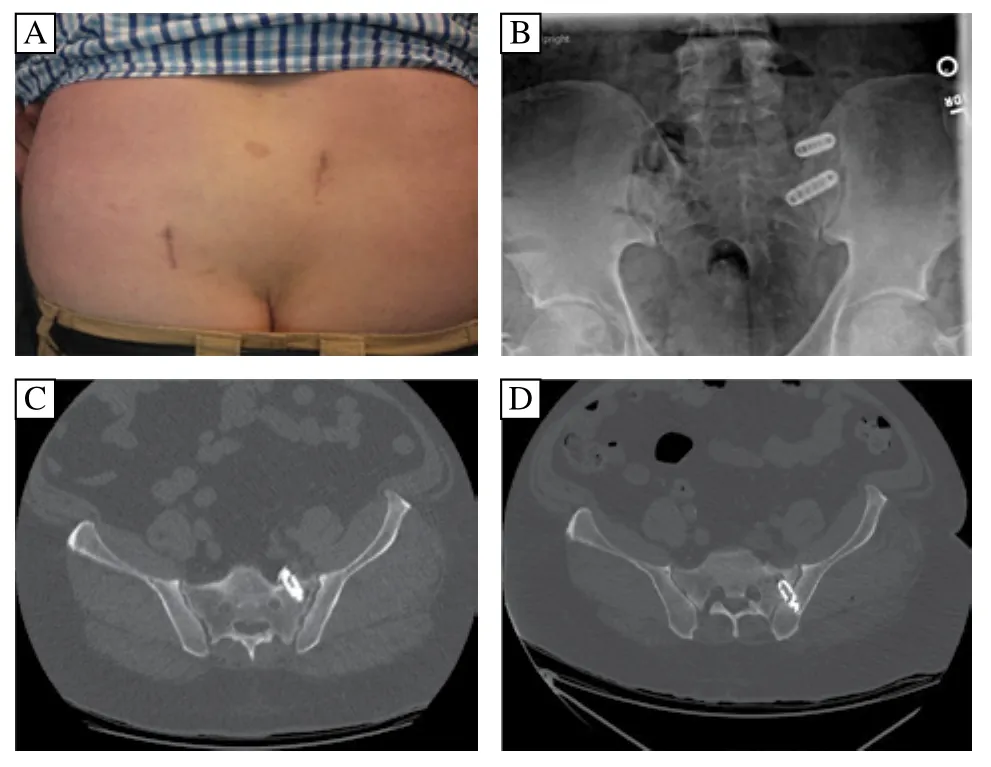
Fig. 4 Postoperative wound and imaging with revision. A: Early postoperative wound appearance (reference arc wound, right; SIJ fusion wound, left). B: The post-operative x-ray demonstrates cage placement; however, the pre-revision X-ray was not helpful in confirming the proper cage position. C: Thus, a post-operative axial CT was performed. It demonstrated that the lower SIJ cage was placed deeply, breaching the ventral cortical wall of the sacrum and compressing the neural structure. D: An axial CT of the SIJ cage after revision demonstrated adequate positioning of the cage in the cortical bone.
Our technique using the O-arm®is particularly suited to SIJ fusion. Due to auto-registration, surgeons do not need to perform the registration required using other navigation techniques[8,30-33].With auto-registration and multiplanar views of the SIJ, surgeons can perform arthrodesis in numerous ways. Our two illustrative cases utilized two different techniques for SIJ fusion. For neurosurgeons familiar with the image-guidance surgery but unfamiliar with SIJ anatomy, the learning curve should be less than attempting SIJ fusion with fluoroscopy. Multiplanar view of the sacroiliac joint afforded by O-arm®is very reassuring as opposed to trying to interpret various fluoroscopic views. Additional benefits include smaller incisions and less blood loss with this percutaneous technique as opposed to larger open procedures.
Our technique, like any guidance system, is limited by dependence on expensive technology that may limit access to many surgeons. Accuracy of implant position using any kind of image-guidance system is predicated on accurate registration. Due to our concern of the surgical procedure interfering with the reference frame, the frame was placed contralateral to the surgical site. With our percutaneous technique, intraoperative confirmation of the registration accuracy is difficult. A cage inserter that can be tracked by the navigation camera may reduce or eliminate the complication reported in our Illustrative Case 2[34]. Therefore, we recommend checking the final position of the SIJ implants using O-arm®prior to reference frame removal and wound closure.
In conclusion, navigated percutaneous sacroiliac joint fusion integrating the O-arm®allows for real-time navigation with the ability to check the implant position before leaving the operating room.
References
[1] Katz V, Schofferman J, Reynolds J. The sacroiliac joint: a potential cause of pain after lumbar fusion to the sacrum [J]. J Spinal Disord Tech, 2003, 16(1):96–99.
[2] Maigne JY, Aivaliklis A, Pfefer F. Results of sacroiliac joint double block and value of sacroiliac pain provocation tests in 54 patients with low back pain [J]. Spine (Phila Pa 1976), 1996, 21(16):1889–1892.
[3] Schwarzer AC, Aprill CN, Bogduk N. The sacroiliac joint in chronic low back pain [J]. Spine (Phila Pa 1976), 1995, 20(1):31–37.
[4] Sembrano JN, Polly DW, Jr. How often is low back pain not coming from the back? [J] Spine (Phila Pa 1976), 2009, 34(1):E27–32.
[5] DePalma MJ, Ketchum JM, Saullo TR. Etiology of chronic low back pain in patients having undergone lumbar fusion [J]. Pain Med, 2011, 12(5):732–739.
[6] Ha KY, Lee JS, Kim KW. Degeneration of sacroiliac joint after instrumented lumbar or lumbosacral fusion: a prospective cohort study over five-year follow-up [J]. Spine (Phila Pa 1976), 2008, 33(11):1192–1198.
[7] Buchowski JM, Kebaish KM, Sinkov V, et al. Functional and radiographic outcome of sacroiliac arthrodesis for the disorders of the sacroiliac joint [J]. Spine J, 2005, 5(5): 520- 528; discussion 529.
[8] Giannikas KA, Khan AM, Karski MT, et al. Sacroiliac joint fusion for chronic pain: a simple technique avoiding the use of metalwork [J]. Eur Spine J, 2004, 13(3):253–256.
[9] Moore M. Movement, stability, and low back pain: the essential role of the pelvis. Surgical treatment of chronic painful sacroiliac joint dysfunction. New York: Churchill Livingstone, 1997, 563–572.
[10] Polly DW, Cher DJ,Wine KD, et al. Randomized Controlled Trial of Minimally Invasive Sacroiliac Joint Fusion Using Triangular Titanium Implants vs Nonsurgical Management for Sacroiliac Joint Dysfunction: 12-Month Outcomes [J]. Neurosurgery, 2015, 77(5):674–691.
[11] Daffner RH, Sciulli RL. CT-guided iliosacral screw placement [J]. Semin Musculoskelet Radiol, 2013, 17(4): 407–415.
[12] Sciulli RL, Daffner RH, Altman DT, et al. CT-guided iliosacral screw placement: technique and clinical experience [J]. AJR Am J Roentgenol, 2007, 188(2):W181-W192.
[13] Takao M, Nishii T, Sakai T, et al. CT-3D-fluoroscopy matching navigation can reduce the malposition rate of iliosacral screw insertion for less-experienced surgeons [J]. J Orthop Trauma, 2013, 27(12):716–721.
[14] Shuler TE, Boone DC, Gruen GS, et al. Percutaneous iliosacral screw fixation: early treatment for unstable posterior pelvic ring disruptions [J]. J Trauma, 1995, 38(3):453–458.
[15] Lorio MP, Polly DW, Jr., Ninkovic I, et al. Utilization of Minimally Invasive Surgical Approach for Sacroiliac Joint Fusion in Surgeon Population of ISASS and SMISS Membership [J]. Open Orthop J, 2014, 8:1–6.
[16] Ledonio CG, Polly DW, Jr., Swiontkowski MF. Minimally invasive versus open sacroiliac joint fusion: are they similarly safe and effective? [J] Clin Orthop Relat Res, 2014, 472(6):1831–1838.
[17] Coste C, Asloum Y, Marcheix PS, et al. Percutaneous iliosacral screw fixation in unstable pelvic ring lesions: the interest of O-ARM CT-guided navigation [J]. Orthop Traumatol Surg Res, 2013, 99(4 Suppl):S273-S278.
[18] Smith AG, Capobianco R, Cher D, et al. Open versus minimally invasive sacroiliac joint fusion: a multi-center comparison of perioperative measures and clinical outcomes [J]. Ann Surg Innov Res, 2013, 7(1):14.
[19] Ledonio CG, Polly DW, Jr., Swiontkowski MF, et al. Comparative effectiveness of open versus minimally invasive sacroiliac joint fusion [J]. Med Devices (Auckl), 2014, 7:187–193.
[20] Attia W, Orief T, Almusrea K, et al. Role of the O-arm and Computer-assisted Navigation of Safe Screw Fixation in Children with Traumatic Rotatory Atlantoaxial Subluxation [J]. Asian Spine J, 2012, 6(4):266–273.
[21] Del Curto D, Kim JS, Lee SH. Minimally invasive posterior cervical microforaminotomy in the lower cervical spine and C-T junction assisted by O-arm-based navigation [J]. Comput Aided Surg, 2013, 18(3-4):76–83.
[22] Hellstrom PA, Katisko J, Finnila P, et al. Sacral nerve stimulation lead implantation using the O-arm [J]. BMC Urol, 2013, 13:48.
[23] Castro Castro J, Rodino Padin J, Pinzon Millan A, et al. Posterior lumbar fusion using the O-arm surgical imaging system: initial experience [J]. Neurocirugia (Astur), 2013, 24(1):1–8.
[24] RayWZ, RavindraVM, SchmidtMH, et al. Stereotactic navigation with the O-arm for placement of S-2 alar iliac screws in pelvic lumbar fixation [J]. J Neurosurg Spine, 2013, 18(5):490- 495.
[25] Raza SM, See AP, Lim M. Real-time imaging with the o-arm for skull base applications: a cadaveric feasibility study [J]. J Neurol Surg B Skull Base, 2012, 73(5): 293–301.
[26] Shin MH, Ryu KS, Park CK. Accuracy and Safety in Pedicle Screw Placement in the Thoracic and Lumbar Spines: Comparison Study between Conventional C-Arm Fluoroscopy and Navigation Coupled with O-Arm(R) Guided Methods [J]. J Korean Neurosurg Soc, 2012, 52(3): 204–209.
[27] Tabaraee E, Gibson AG, Karahalios DG, et al. Intraoperative cone beam-computed tomography with navigation (O-ARM) versus conventional fluoroscopy (C-ARM): a cadaveric study comparing accuracy, efficiency, and safety for spinal instrumentation [J]. Spine (Phila Pa 1976), 2013, 38(22):1953–1958.
[28] Van de Kelft E, Costa F, Van der Planken D, et al. A prospective multicenter registry on the accuracy of pedicle screw placement in the thoracic, lumbar, and sacral levels with the use of the O-arm imaging system and StealthStation Navigation [J]. Spine (Phila Pa 1976), 2012, 37(25):E1580-E1587.
[29] Yson SC, Sembrano JN, Sanders PC, et al. Comparison of cranial facet joint violation rates between open and percutaneous pedicle screw placement using intraoperative 3-D CT (O-arm) computer navigation [J]. Spine (Phila Pa 1976), 2013, 38(4):E251-E258.
[30] Cho JY, Chan CK, Lee SH, et al. The accuracy of 3D image navigation with a cutaneously fixed dynamic reference frame in minimally invasive transforaminal lumbar interbody fusion [J]. Comput Aided Surg, 2012, 17(6):300–309.
[31] Drazin D, Liu JC, Acosta FL, Jr. CT navigated lateral interbody fusion [J]. J Clin Neurosci, 2013, 20(10):1438–1441.
[32] Dzupa V, Krbec M, Kaderabek R, et al. Intraoperative CT navigation in spinal and pelvic surgery: initial experience [ J]. Rozhl Chir, 2013, 92(7):379–384.
[33] Nelson EM, Monazzam SM, Kim KD, et al. Intraoperative fluoroscopy, portable X-ray, and CT: patient and operating room personnel radiation exposure in spinal surgery [J]. Spine J, 2014, 14(12):2985-2991.
[34] Kim KD, Johnson JP, Masciopinto JE, et al. Universal calibration of surgical instruments for spinal stereotaxy [J]. Neurosurgery, 1999, 44(1):173–177; discussion 177–178.
✉ Kee D Kim, MD, Professor, Department of Neurological Surgery, University of California, Davis School of Medicine, 4860 Y Street, Suite 3740, Sacramento, CA 95817, Tel/fax: 916-734-3102/916-452-2580, E-mail: kdkim@ucdavis.edu.
25 June 2015, Revised 5 October 2015, Accepted 20 November 2015, Epub 10 December 2015
R651, Document code: A.
The authors reported no conflict interests.
杂志排行
THE JOURNAL OF BIOMEDICAL RESEARCH的其它文章
- Organ donation in China: the major progress and the continuing problem
- Cerebral ischemia during surgery: an overview
- Apolipoprotein A-V gene therapy for disease prevention / treatment: a critical analysis
- HDL signaling and protection against coronary artery atherosclerosis in mice
- Prevalence and risk factors of HIV and syphilis, and knowledge and risk behaviors related to HIV/AIDS among men who have sex with men in Chongqing, China
- Effects of closing and reopening live poultry markets on the epidemic of human infection with avian influenza A virus
