Treatment effect of antipsychotics in combination with horticultural therapy on the inpatients with schizophrenia: a randomized, case-controlled study
2016-12-09ShunhongZHUHengjingWANZhideLUHuipingWUQunZHANGXiaoqiongQIANChenyuYE
Shunhong ZHU, Hengjing WAN, Zhide LU, Huiping WU, Qun ZHANG, Xiaoqiong QIAN, Chenyu YE*
·Original research article·
Treatment effect of antipsychotics in combination with horticultural therapy on the inpatients with schizophrenia: a randomized, case-controlled study
Shunhong ZHU1, Hengjing WAN1, Zhide LU2, Huiping WU1, Qun ZHANG1, Xiaoqiong QIAN1, Chenyu YE3,*
horticultural therapy; schizophrenia; randomization; placebo-controlled; China
1. Introduction
Schizophrenia is a severe mental illness with high inpatient rate and disabling rate; it is one of the major psychiatric disorders prevented and treated by any country.[1]There were over 7800,000 patients with schizophrenia, which occupied 50% of the lifelong psychiatric disorders (except neurosis).[2]The most important treatment method till now is antipsychotic medication. Likewise, the rehabilitation therapy plays a significant role in alleviating psychiatric symptoms, enabling patients with schizophrenia to readapt to society and totally restoring their social functions. Horticultural therapy as a newly developed rehabilitation therapy has gained several attentions.
There is no uniform definition on horticultural therapy. The relatively aggregable definition is posed by the American Horticultural Therapy Association(AHTA), which defines ‘horticultural therapy’ as ‘the engagement of a person in gardening and plantbased activities, facilitated by a trained therapist, to achieve specific therapeutic treatment goals’.[3]Early in the Egyptian times, people learned that agricultural activities such as farming could benefit physical and psychological health. But it was not until the late 18thcentury that Benjamin Rush, the pioneer of Psychiatry,formally suggested the idea of the treatment effects of engaging in horticultural activities on patients with psychiatric disorders. Many domestic and international literatures thought that the horticultural therapy had relatively good treatment effects on emotions, physical health, social networking and cognitions and that the horticultural therapy could improve patients overall health and quality of life, especially in promoting patients’ physical strength and cardiac functions.[4,5]A large cross-sectional study in Scotland conducted by Shiue found that of the 9709 studied adults, there were certain higher improvements in mental health especially in attention, feeling the significance of life, and being capable of making life decisions and so on among those who had recently participated in gardening than those who had not.[6]But there is a severe lack of standardized study in horticultural therapy. Kamioka and colleagues tried to include randomized, placebo-controlled studies in decades in order to conduct systematic review, and the results showed that only 4 articles met the inclusion criteria.[7]Of those 7 articles related to horticultural therapy which did not meet the criteria of randomized,placebo-controlled studies, the research subjects were all elderlies and other patients with chronic diseases in nursing facilities without investigation on mental illness. Of the 4 articles included, there was only 1 article related to patients with psychiatric disorders and the sample size was just 24.[8]Whereas the systematic review of horticultural therapy by Liu and colleagues also found only that article met inclusion criteria.[9]
There are few studies on horticultural therapy in China; mostly are systematic reviews by foresters and agriculturists. In 2001, Ban once conducted a placebocontrolled study on horticultural therapy and found that it had certain benefits in improving mental health,social adaptability and self-care ability among patients with schizophrenia.[10,11]However, there were several limitations in this study: the control group in the study was not randomized; researchers mainly investigated the indicators in rehabilitation; the ‘horticultural therapy’ was just spreading seeds and researchers let patients themselves sow seeds without specific criteria and standardized instructions.
The study aims at using standardized horticultural therapy instructions with randomized, placebocontrolled method to investigate the treatment effect of horticultural therapy on patients with schizophrenia in a relatively large sample in order to further test its application possibility of standardized implementation in psychiatric hospitals.
2. Methods
2.1 Participants
Inpatients of the two rehabilitation wards in the Minhang District Mental Health Center were screened for participation into the study in September to December 2015. The inclusion criteria are (a) the schizophrenic patients who met the ICD-10 Diagnostic Criteria; (b) the course of disease above two years;(c) age 18 to 70; (d) basic control of the psychiatric symptoms (PANSS < 60); (e) ability to communicate and express self-feeling orally; (f) having a certain degree of motility; and (g) signed informed consent. Exclusion criteria include (a) no comorbidity of other psychiatric diseases; (b) presence of the attack, suicidal, and selfinjurious behaviors; (c) difficulty in communication;(4) presence of severe somatic diseases in patients,restraining the patients from performing a certain level of physical activities.
In the two rehabilitation wards, there were 189 inpatients and 130 of them fulfilled the inclusion criteria. In the end, 110 of the 130 qualified patients consented to join the study and were randomized into two groups. Medication treatment was given to both the intervention and control groups based on the clinical application, whereas horticultural therapy along with the medication treatment was only assigned to the intervention group for twelve months. By the fourth week of the follow-up, one patient from the intervention group and two patients from the control group were discharged from the hospital. By the twelfth week, an additional two patients and one patient were discharged from the intervention and control groups respectively.At the end of the study, there were 52 patients who could complete the follow-up in each group (see the Figure 1). There were 55 participants (24 males) in the intervention and control groups respectively. The average age was 46.5 (9.0). The median age were 44 and 48.2 (11.3). The median age was 48 and it is not statistically significant (t=-0.867, p=0.39). The course of disease on average was 20.1 (8.9) years; the median were 19 and 21.2 (10.5) years respectively; the medianwas 20 years. There was no statistically significant difference (t=-0.59, p=0.56). The average times of hospitalization of the intervention and control groups were 59.1 (62.3) and 59.4 (62.2) months; the medians were 45 and 43 months respectively, where there was no statistical significance (t=-0.03, p=0.98). The highest education attainment of the participants was 6 in elementary school, 17 in junior high school, 24 in senior high school or the same grade, and 8 in college or above in the intervention group; 7 in elementary school, 22 in junior high school, 20 in senior high school or the same grade, and 6 in college or above in the control group. There was no statistical significance (χ2=1.37,p=0.71). The marital status of the participants was 27 unmarried, 13 married, and 15 divorced or widowed in the intervention group; 32 unmarried, 10 married, and 13 divorced or widowed in the control group. There was no statistically significant difference (χ2=0.96, p=0.62).The total PANSS scores of the intervention and control groups were 47.7 (5.7) and 48.3 (5.8). There was not statistically significant difference (t=-0.52, p=0.61).

Figure 1. Flowchart of the study
2.2 The design of the horticultural therapy course curriculum
The horticultural therapy course lasted for twelve weeks with three sessions a week, ninety minutes a session. There were both indoor and outdoor activities.Outdoor activities were arranged to take place in relatively nice weather, whereas indoor activities were taken place in continuous unfavorable weather.A rehabilitative therapist who had the qualification of the state consultant psychologist grade 2 led the group and instructed the participants to allocate soil for,plant, water, fertilize, and prune the fl oral plants along with the assistance of another rehabilitative therapist.Moreover, the participants plowed the soil in the garden in addition to seeding, watering, fertilizing, weeding,and catching pests. Towards the end of the therapy,participants could get to enjoy the fl oral plants and pick,cook, and taste the vegetables. Participants were given ten minutes for experience sharing followed by the summary and comments of the therapists.
In the outdoor activities, every participant had a 0.5 square meters of land for planting in a 2 meter times 15 meters outdoor garden. Indoor pot planting was adopted in the floral gardening due to the benefits of convenient planting, management, and maintenance(see table 1).
2.3 Evaluation scale and method
Positive and Negative Syndrome Scale is a rating scale that has been widely used in psychiatry for evaluating the quantitative change of the psychiatric symptoms.The PANSS comprises 30 items including 7 symptoms on the Positive Scale (P), 7 symptoms on the Negative Scale(N), and 16 symptoms on the General Psychopathology Scale (G). Additionally, there are 3 supplementary items for evaluating the assault risk. The Cronbach’s alpha was 0.73 to 0.83 on the scales. Generally, the index of the split-half reliability on the psychiatric scale is 0.8. The test-retest reliability was 0.77 to 0.89[13]. The evaluator,who was a psychiatrist not located in the participants’wards, was blinded in this study, assessing all participants at the baseline, 4 months of treatment, and 12 months of treatment regularly.
2.4 Statistical analysis
SPSS software version 19.0 was used for statistical analysis. T-test and analysis of variance (ANOVA) were used for analyzing categorical data. Chi-square test was used for analyzing quantitative data. Repeated measurement analysis of variance was used for analyzing repeated measurement data. Two-sided test was used in this study. The p-value less than 0.05 is considered statistically significant.
3. Results
3.1 The psychotic medication usage status and attendance of the two study groups
The kinds of anti-psychotic medications and the average dosage of the two groups of participants can be referred to table 2. The quantity of all patients’ medications were expressed in terms of the equal amount of Olanzapine according to Leucht and his fellows’findings, where 1 mg/d of Olanzapine was equivalent to 1.4 mg/d of aripiprazole, 32.3mg/d of quetiapine,0.4 mg/d of risperidone, 7.9 mg/d of ziprasidone,or paliperidone (no record for conversion). After the exclusion of a patient who took 6mg/d of paliperidone,the intervention group (54 cases) had a dose of 13.2(5.2) mg/d of Olanzapine equivalent to the originalmedication and the median was 14.3 mg/d. The control group had a dose of 13.8 (6.1) mg/d of Olanzapine equivalent to the original medication and the median was 14.3 mg/d. The difference of the two groups was not statistically significant (t=-0.46, p=0.65).

Table 1. Horticultural therapy curriculum table
The perfect attendance was 1980 times. Yet, the actual attendance was 1787 times. Therefore, the attendance rate was 90.25%. The reasons for the absences include formal discharge from the ward (3 participants with a total of 55 times of absence), leave out (46 times), and illnesses such as body discomfort,cold, and fever (92 times). The attendance rate of the participants who completed the follow-up reached 92.63% after the exclusion of 3 participants lost to follow-up. To complete the horticultural therapy,participants had to attend 30 out of 36 therapeutic sessions. Other than the 3 discharged patients, the rest of the 52 patients successfully completed the therapy.
3.2 The comparison of the total PANSS scores before and after treatment in the two study groups
The difference of the total PANSS scores between the two study groups in the baseline was not statistically significant. Nevertheless, there was statistical significance in week four (t=-3.97, p<0.01) and week twelve (t=-5.57, p<0.001). The difference of the total PANSS score of the two study groups before and after treatment was statistically significant. Repeated measurement analysis of variance was used to compare the change difference of the overall time trend of the treatment and control groups (Ftimexbetweengroup= 16.981,p<0.001), indicating the difference of the total PANSS scores of the treatment and control groups during treatment was statistically significant. See table 3.
3.3 The comparison of the PANSS scales before and after treatment in the two study groups
Comparing the PANSS score of the two groups of patients would find that the difference of the two groups on the scores of Positive Scale and General Psychopathology Scale at week four and twelve of the follow-up were statistically significant. Comparison of its own before and after differences also had statistical significance. On the Negative Scale score, the difference of the two groups at the fourth week of treatment was not statistically significant, but it was at the twelfth week. There were statistically significant differences in their before and after comparison. Repeated measurement analysis of variance compared the change of time on the overall time trend of the treatment and control groups, resulting (Ftimexbetweengroup=9.200, p <0.001) on the Positive Scale; (Ftimexbetweengroup=9.197, p <0.001) on the Negative Scale; and (Ftimexbetweengroup=2.478,p = 0.106) on the General Psychopathology Scale. See table 4.

Table 2 Comparison of the common medications used in the two groups
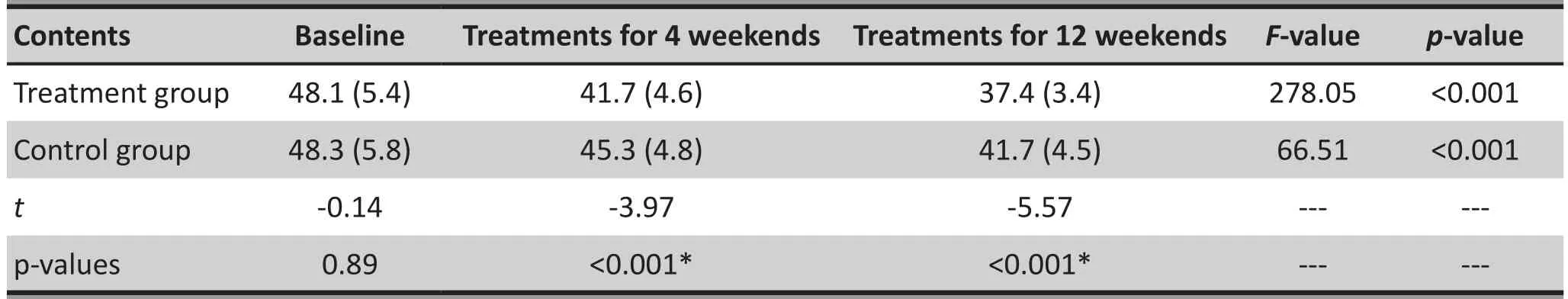
Table 3. Comparison of the total PANSS of the two groups
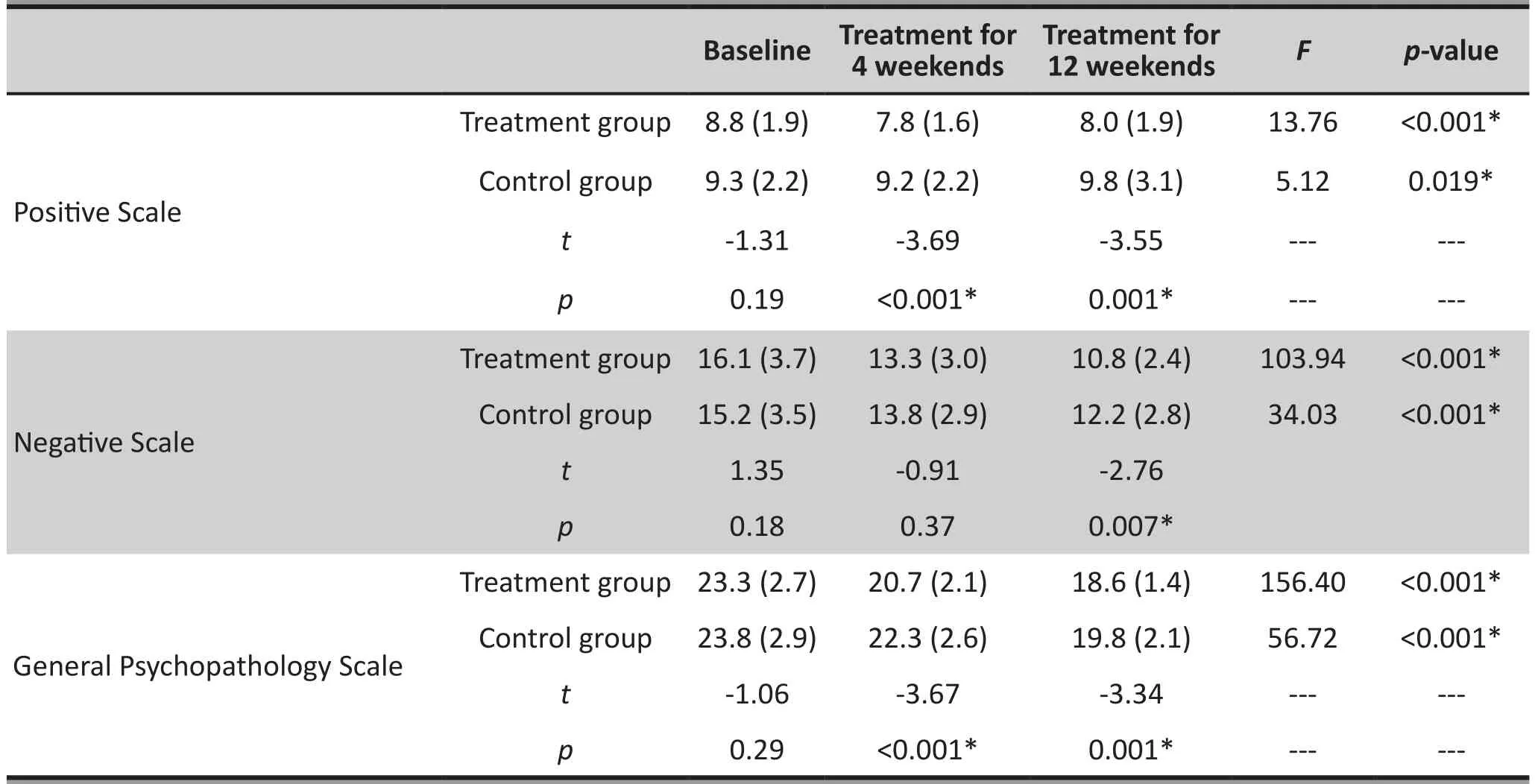
Table 4. Comparison of the scales of the two groups before and after treatment
4. Discussion
4.1 Main findings
The research is the first randomized, assesementblind, case-controlled study investigating the treatment effect of antipsychotic medication in combination with horticultural therapy on inpatients with schizophrenia in China. Research in patients with dementia[14,15]showed that there were several benefits in the process of conducting horticultural therapy: Utilizing various sensory organs, touching and smelling plants,seeing plants growing, and harvesting and tasting fruits all helped patients gain confidence and sense of achievement and improve their quality of life;the needs to interact with people and plants could boost emotional communication and interpersonal relationship; the needs to keep focus on gardening and to use their hands and brains could improve patients’cardiopulmonary function and attention; having understandings of the basic instruction and practice about gardening, gaining related knowledge, and grasping planting techniques could further improve the rehabilitation of patients’ social functions. Previous research suggested that although there was a lack of more effective evidence, the horticultural therapy might improve the negative symptoms among inpatients with schizophrenia.[9]The implementation of the horticultural therapy needs strong operability, not enough understandings and communication skills, and a certain degree of responsibility. Patients with schizophrenia receiving horticultural therapy need to communicate and interact with each other, which can improve negative emotions and change their listless lifestyles.So the horticultural therapy is suitable for alleviating negative emotions and showing declines in activities in the late phase of patients with schizophrenia.The study found that the sole use of medication could further alleviating psychotic symptoms among inpatients with schizophrenia, including both positive and negative symptoms, but this effect was sounder in combination with the horticultural therapy. Considering that participants in the intervention group and in the control group are in the same ward, the possibility of‘contamination effect’ made it obvious for the alleviation of psychotic symptoms. Likewise, scheduled follow-ups conducted by psychiatrists who were not in charge of the experimental ward might also show the ‘Hawthorne effect’; in other words, the psychotic symptoms got alleviation because of psychiatrists’ extra attentions.Compared with previous studies, such improvements were depicted in both positive and negative symptoms,and the improvements were quite obvious. The phenomena may be related to the design of the therapy duration. The duration of the horticultural therapy lasted relatively long (approximately 3 months), thus patients were more involved in it than the previous participants. So the present study showed more improvements than previous studies. Likewise, as a newly developed and the only outdoor rehabilitation therapy arranged for multiple times, the horticultural therapy can arouse patients’ curiosity and excitement,which may have certain influence on the research results.
There is by far no international formal training for horticultural therapist and no standardized criteria which can be applied into health settings. The duration of the horticultural therapy in the present study is 12 weeks, and there are 3 sessions every week. Studies about horticultural therapy in China are usually just spreading seeds to patients and letting them to sow without specific course design. Other relatively formal and similar studies usually consist of 6 weeks durations but 5 sessions each week.[16-18]One study was composed of 2 weeks with 10 successive sessions.[8]Compared with related study described above, the frequency of the present study is longer. There are several advantages:a) the long duration meets the rule of plants growing,and patients can try gardening various plants with not only one harvest; b) the long duration benefits the learning, handling and grasping of gardening techniques; c) the long duration means having many therapeutic contents regardless of the impact of the weather in order to arrange sessions flexibly; d) the long duration benefits group construction, which can boost cooperative behaviors among team members and e) the low frequency lowers the absence rate; in other words, there would be not many records with multiple absence due to weather or having somatic diseases such as cold. There is a limitation: the long duration means high possibility of drop-out. But from the perspective of the clinical practice, once participated in the horticultural therapy, patients showed relatively good conformity. There was no other reason of drop-out other than leaving hospital. The present study provides valuable reference for future standardized design of the horticultural therapy.
There were 6 patients (each group has 3 patients)of whom we have lost contact. The reason was being better off and thus leaving hospital. Because inpatients with schizophrenia in the rehabilitation ward mostly showed stable disease conditions, most of them met the criteria of leaving hospital but had to stay for a long time caused by multiple factors. The 6 patients described before were all brought by their relatives to go home without direct relationship with their own disease conditions.
Research found that movement therapies could help patients keep focus and adjust their own control over activity, which could alleviate the negative symptoms among patiens with schizophrenia. Compared with other rehabilitation therapies, the intellectual and educational requirements of participating in horticultural therapy are relatively low (so many studies investigate patients with dementia), thus participants can participate in such therapy with only listening to the basic instructions. The horticultural therapy can improve participants’ general health status, including quality of life, somatic condition and cardiopulmonary function.Besides, the part of close involvement with nature is also an advantage compared with other rehabilitation therapies.[20]But participating in horticultural therapy needs certain laboring work especially in outdoor environment, so there may be certain restrictions for patients with relatively poor somatic conditions. In the clinical practice we found that many female patients thought gardening to be considerably exhausting. They would be only willing to look rather than garden, but they could positively participate in cultivating indoor bonsai. These circumstances imply that we need to design different therapeutic courses which have special considerations for males and females and people with relatively good stamina and those with relatively poor stamina.
4.2 Limitations
There are several limitations in the present study: a)the research duration consists of spring and autumn,and different seasoning plants show different growing patterns. So there may be certain influence on the standardization of the horticultural therapy; b) the research sample is relatively small, thus it is hard to analyze patients of whim we have lost contact and c)there is no control over antipsychotic medication.
4.3 Implication
The present study is the first one investigating the treatment effect of antipsychotics in combination with standardized horticultural therapy on patients with schizophrenia. The study provides guidance for the standardization of the horticultural therapy, which provides reference for the rehabilitation therapy among patients with schizophrenia.
Funding
The study was funded by the project of the Minhang District Science and Technology Committee (project number: 2015MHZ062).
Conflict of interest statement
The authors declare no conflict of interest related to this manuscript.
Informed consent
All participants and their legal guardians provided signed informed consent to participate this study.
Ethics approval
The study was approved by the Ethics Committee of the Minhang District Mental Health Center (approval number: LW2016001).
Authors’ contributions
Shunhong Zhu was in charge of the actual implementation and data collection; Hengjing Wan was in charge of the designs of the research plan and the treatment plan; Zhide Lu was in charge of the psychiatric examinations; Huiping Wu, Qun Zhang and Xiaoqiong Qian were in charge of the actual implementation and data collection; Chenyu Ye was in charge of the research design and drafting the manuscript.
1. Zhao JP, Shi SX. [Guidelines for Prevention and Treatment of Schizophrenia in China (Second Edition)]. Beijing: China Medical Electronic Audio and Video Publishing House;2015. P. 1-5. Chinese
2. Feng X. [A study of the factors leading to schizophrenic recurrence]. Bao Jian Yi Xue Yan Jiu Yu Shi Jian. 2015; 12(1):27-29. Chinese
3. Hu WF. [The history and research trends of horticultural therapy]. Anhui Nong Ye Ke Xue. 2013; 41(20): 8792-8794. Chinese. doi: http://dx.chinadoi.cn/10.3969/j.issn.0517-6611.2013.20.119
4. Chen XQ, Wu JP. [Status quo of horticultural therapy].Beijing Lin Ye Da Xue Xue Bao. 2011; 10(3): 41-45. Chinese. doi: http://dx.chinadoi.cn/10.3969/j.issn.1671-6116.2011.03.007
5. Loh PL, Wainwright MJ. Horticultural therapy: a psychosocial treatment option at the Stephen D. Hassenfeid Children’s Center for cancer and blood disorders. Primary Psychiatry.2008; 15(7): 73-77. doi: http://dx.doi.org/10.1214/13-AOS1162
6. Ashman J. Growing Healing One Garden at a Time. J Christ Nurs. 2016; 33(1): 35-37
7. Shiue I. Gardening is beneficial for adult mental health:Scottish Health Survey, 2012-2013. Scand J Occup Ther.2015; 16: 1- 6. doi: http://dx.doi.org/10.3109/11038128.2 015.1085596
8. Kamioka H, Tsutani K, Yamada M, Park H, Okuizumi H, Honda T, et al. Effectiveness of horticultural therapy: a systematic review of randomized controlled trials. Complement Ther Med. 2014; 22(5): 930-943. doi: http://dx.doi.org/10.1016/j.ctim.2014.08.009
9. Kam MCY, Siu AMH. Evaluation of a horticultural activity programme for persons with psychiatric illness. Hong Kong J OccupTherapy. 2010; 20(2): 80- 86. doi: http://dx.doi.org/10.1016/S1569-1861(11)70007-9
10. Liu Y, Bo L, Sampson S, Roberts S, Zhang G, Wu W.Horticultural therapy for schizophrenia. Cochrane Database Syst Rev. 2014; 5: CD009413. doi: http://dx.doi.org/10.1002/14651858.CD009413.pub2
11. Ban RY. [Effect of horticultural therapy on rehabilitation of patients with chronic schizophrenia]. Shi Yong Hi Li Za Zhi. 2002; 18(2): 50-51. Chinese. doi: http://dx.chinadoi.cn/10.3760/cma.j.issn.1672-7088.2002.02.034
12. Ban RY. [Rehabilitation effect of gardening therapy to treat chronic schizophrenia patients]. Hu Li Yan Jiu. 2001; 15(6):327-329. Chinese. doi: http://dx.chinadoi.cn/10.3969/j.issn.1009-6493.2001.06.011
13. Li HF. [Common Scales on the Psychiatric Medicine Clinical Research (Second Edition)]. Shanghai: Shanghai science and Technology Education Publishing House; 2014. P. 32.Chinese
14. Leucht S, Samara M, Heres S, Patel MX, Furukawa T,Cipriani A, et al. Dose equivalents for second-generation antipsychotic drugs: The classical mean dose method.Schizophr Bull. 2015; 41(6): 1397-1402. doi: http://dx.doi.org/10.1093/schbul/sbv037
15. Blake M, Mitchell G. Horticultural therapy in dementia care:a literature review. Nurs Stand. 2016; 30(21): 41-47. doi:http://dx.doi.org/10.7748/ns.30.21.41.s44
16. Noone S, Innes A, Kelly F, Mayers A. ‘The nourishing soil of the soul’: The role of horticultural therapy in promoting well-being in community-dwelling people with dementia.Dementia (London). 2015; pii: 1471301215623889. doi:http://dx.doi.org/10.1177/1471301215623889
17. Jarrott SE, Gigliotti CM. Comparing responses to horticultural-based and traditional activities in dementia care pro-grams. Am J Alzheimers Dis Other Demen. 2010; 25(8): 657 - 665. doi: http://dx.doi.org/10.1177/1533317510385810
18. Tse MM. Therapeutic effects of an indoor gardening programme for older people living in nursing homes.J Clin Nurs. 2010; 19(7-8): 949-958. doi: http://dx.doi.org/10.1111/j.1365-2702.2009.02803.x
19. Kim SY, Son KC, Jung HJ, Yoo JH, Kim BS, Park SW. Effect of horticultural therapy on functional rehabilitation in hemiplegic patients after stroke. Korean J Hortic Sci Technol.2003; 44: 780-785
20. Martin LA, Koch SC, Hirjak D, Fuchs T. Overcoming disembodiment: The effect of movement therapy on negative symptoms in schizophrenia-a multicenter randomized controlled trial. Front Psychol. 2016; 7: 483.doi: http://dx.doi.org/10.3389/ fpsyg.2016.00483
12. Ashman J. Growing healing one garden at a time. J Christ Nurs. 2016; 33(1): 35-37

Shunhong Zhu Graduated from Shanghai Jiaotong University School of Medicine and obtained the Bachelor’s degree in Nursing in 2009. She had been working at the Minhang District Mental Health Center since 1998. She is currently the chief nurse and the rehabilitation therapist at the Department of Rehabilitation. Her main research interest are the influence and treatment effect of horticultural therapy on patients with psychiatric disorders.
合并园艺治疗对慢性精神分裂症住院患者随机对照研究
诸顺红,万恒静,陆志德,吴慧萍,张群,钱晓琼,叶尘宇
园艺治疗,精神分裂症, 随机,对照
Background:As a newly developed treatment method for schizophrenia, horticultural therapy is gaining more and more attentions. However, there is by far few researches investigating it, and there is also a lack of related standardized treatment program.Aim:Investigate treatment effect of horticultural therapy on patients with schizophrenia and its possibility of standardized application in psychiatric hospitals.Methods:110 patients with schizophrenia who met the inclusion criteria and signed the consent form were selected at the rehabilitation ward of the Minhang District Mental Health Center from September 2015 to December 2015. We used random-number methods to classify patients into either the intervention group or the control group. While the two groups both received normal medications, the intervention group also attended horticultural therapy. Patients in the intervention group were led to implement the therapy by rehabilitation therapist who had obtained the second class psychological counselor qualification. The whole session lasted for 12 weeks. It is 3 times every week and each session lasted for 90 minutes. The specific contents included ridging, planting, watering, fertilizing and pruning for fl owers; plowing, sowing, watering,fertilizing, weeding and catching pests for gardens; appreciating, collecting vegetables, cooking and tasting for flowers and grasses. Before the 10 minutes end of every session, patients mutually expressed their thoughts and experiences and rehabilitation therapist concluded. The two groups were measured by the Positive and Negative Syndrome Scale (PANSS) at the baseline, the end of the 4thweek session and the end of the 12thsession.Results:There was no statistically significant difference in gender, age, course of disease, marital status,the mean dosage of using antipsychotic medications and the PANSS score before the intervention among two groups. The PANSS score in the intervention group was statistically significant lower than in the control group both at the end of the 4thweek session (t=-4.03, p<0.001) and the end of the 12thsession (t=-5.57,p<0.001). There was statistically significant difference before and after intervention in the intervention group(F=253.03, p<0.001); there was statistically significant difference before and after intervention in the control group (F=67.66, p<0.001). There was statistically significant difference in the positive scale score among the two groups both at the end of the 4thweek session (t=-3.69, p<0.001) and the end of the 12thsession (t=-3.55,p<0.001); there was statistically significant difference in the general psychopathology scale score among the two groups both at the end of the 4thweek session (t=-3.67, p<0.001) and the end of the 12thsession (t=-3.34,p<0.001). Likewise, there were statistically significant differences in the positive scale scores at the baseline,the end of the 4thweek session and the end of the 12thsession both among the intervention group (F=13.76,p<0.001) and the control group (F=5.12, p=0.02); there were statistically significant differences in the general psychopathology scale scores at the baseline, the end of the 4thweek session and the end of the 12thsession both among the intervention group (F=156.40, p<0.001) and the control group (F=56.72, p<0.001). There was statistically significant difference in the negative scale score at the end of the 12thsession among two groups(t=-2.76, p<0.001). There were statistically significant differences in the positive scale scores at the baseline,the end of the 4thweek session and the end of the 12thsession both among the intervention group (F=103.94,p<0.001) and the control group (F=34.03, p<0.001).Conclusions:Although antipsychotic medications can alleviate the psychiatric symptoms of patients with schizophrenia, the treatment effect for both positive and negative symptoms would be sounder if it is combined with horticultural therapy.
[Shanghai Arch Psychiatry. 2016; 28(4): 195-203.
http://dx.doi.org/10.11919/j.issn.1002-0829.216034]
1Department of rehabilitation, Minhang District Mental Health Center, Shanghai, China
2Department of medical management, Minhang District Mental Health Center, Shanghai, China
3Department of psychological medicine, Zhongshan Hospital, Fudan University, Shanghai, China
*correspondence: Dr. Ye Chenyu. Mailing address: RD Fenglin 180, Department of psychological medicine, Zhongshan Hospital, Fudan University, Shanghai,China. Postcode: 200032. E-Mail: cycleye@sina.com
背景:园艺疗法作为一种新兴的精神分裂症康复治疗手段逐渐引起重视,但目前研究很少,也缺乏相应的规范化治疗方案。目标:探讨园艺疗法对慢性精神分裂症住院患者的疗效,探索园艺疗法在精神卫生中心规范化实施的可能性。方法:选择2015年9月—2015年12月在本院康复病房符合入组标准并签署知情同意书的精神分裂症患者共110例,用随机数字法分为试验组和对照组,两组均进行常规的药物治疗,试验组合并园艺治疗,在具有国家二级心理咨询师资格的康复治疗师的带领下进行园艺治疗,每周3次,每次90min,共12周。具体内容包括对花卉进行配土、栽植、浇水、施肥及修剪;对田园进行泥土翻耕、播种、浇水、施肥、拔草及捉虫以及花草的观赏、蔬菜的采摘、烹饪、品尝。每次课程结束前10min由患者互相交流心得体会治疗师总结并点评。两组在基线、治疗4周末、治疗12周末予以阳性和阴性症状量表(PANSS)的评估。结果:两组性别、年龄、病程、婚姻、文化、使用的抗精神病药物平均剂量、在治疗前PANSS得分均无显著差异,具有可比性。试验组PANSS得分在治疗4周末、治疗12周末随访时较对照组得分低,差别均有统计学意义(t=-4.03, p<0.001; t=-5.57, p<0.001);自身前后比较差异均有统计学意义(试验组F=253.03,p<0.001; 对照组 F=67.66, p 均 <0.001),两组阳性症状量表和一般精神病理量表得分在治疗4周和治疗12周随访时差异均有统计学意义(4周随访t=-3.69,p<0.001; t=-3.67, p<0.001; 12 周随访 t=-3.55, p=0.001;t=-3.34, p<0.001),自身前后比较差异也有统计学意义(阳性量表试验组F=13.76 p<0.001;对照组F=5.12, p=0.02;一般精神病理量表试验组F=156.40,p<0.001,对照组 F=56.72, p<0.001)。两组之间阴性量表得分在治疗12周末时差异有统计学意义(t=-2.76,p=0.007),自身前后比较差异均有统计学意义(试验组F=103.94, p<0.001;对照组 F=34.03, p<0.001)。结论:药物治疗可改善慢性精神分裂症住院患者的症状,但药物治疗合并园艺治疗的效果更加明显;其中对于阳性症状、阴性症状均有改善。
猜你喜欢
杂志排行
上海精神医学的其它文章
- Some thoughts on the common issue of psychotherapy in different cultures — report on the China conference of psychoanalysis
- A comparison study of Quetiapine and Risperidone’s effectiveness and safety on treating alcohol-induced mental disorder
- Repetitive transcranial magnetic stimulation combined with venlafaxine and lorazepam for treatment of generalized anxiety
- The prospects for the clinical application of exploratory eye movement among patients with psychotic disorders
- A case report of psychoactive drugs aggravating and alleviating Meige syndrome
- Malignant syndrome or withdrawal reaction?
