Comparison of indocyanine green and brilliant blue G to assist internal limiting membrane peeling during macular hole surgery: a systematic review and meta-analysis
2016-12-08ChuanQiXieLingLingZhangShuZhenLiYaDingJia
Chuan-Qi Xie,Ling-Ling Zhang,Shu-Zhen Li, Ya-Ding Jia
1Department of Ophthalmology, First People’s Hospital of Shangqiu, Shangqiu 476000, Henan Province, China2Shangqiu Medical College, Shangqiu 476000, Henan Province, China3Department of Ophthalmology, Shanxi Eye Hospital, Taiyuan 030000, Shanxi Province, China
·Original article·
Comparison of indocyanine green and brilliant blue G to assist internal limiting membrane peeling during macular hole surgery: a systematic review and meta-analysis
Chuan-Qi Xie1,Ling-Ling Zhang2,Shu-Zhen Li1, Ya-Ding Jia3
1Department of Ophthalmology, First People’s Hospital of Shangqiu, Shangqiu 476000, Henan Province, China2Shangqiu Medical College, Shangqiu 476000, Henan Province, China3Department of Ophthalmology, Shanxi Eye Hospital, Taiyuan 030000, Shanxi Province, China
Received: 2016-03-29 Accepted: 2016-09-27
•AIM: To evaluate the outcomes of indocyanine green compared with brilliant blue G used for internal limiting membrane (ILM) peeling in macular hole surgery.
•METHODS: All studies about indocyanine green compared with brilliant blue G for assisting internal limiting membrane peeling during macular hole surgery all over the world were searched. PubMed, Ovid, ScineceDirect, NGC, EBSCO, EMBASE, CNKI, CBM were searched. Two reviewers independently screened the studies for eligibility, evaluated the quality and extracted the data from the eligible studies, with confirmation by cross-checking. Divergence of opinion was settled by discussion or consulted by the expert. Meta-analysis was processed by Rev Man 5.3.
•RESULTS: Seven trials on indocyanine green compared with brilliant blue G for assisting internal limiting membrane peeling during macular hole surgery involving 598 cases met the inclusion criteria in meta-analysis. The baseline of patients’ characteristics were comparable in all studies. By comparing the three common criteria, including best corrected visual acuity (BCVA), macular hole closure rate and postoperative complications, we found that brilliant blue G was better than indocyanine green on improving best corrected visual acuity at 6mo postoperatively[Z=2.10(P=0.04), OR=0.10, 95%CI(0.01, 0.19)]. While there was no statistical difference between two groups on macular hole closure rate[Z=0.69 (P=0.49), OR=0.95, 95%CI(0.82, 1.10)]. And there were no statistical differences in term of postoperative complications between two groups(P>0.05).
•CONCLUSION: The available evidence indicates that the short-term recovery of best corrected visual acuity is significantly better in brilliant blue G (BBG) group than in indocyanine green (ICG) group, especially at 6mo after surgery. The long-term prognosis of BCVA which one study only reported need further study. There were no significant differences on macular hole closure rate and adverse events between two groups.The results indicate that BBG is preferable to ICG for use during macular hole surgery.
indocyanine green; brilliant blue G; macular hole; internal limiting membrane peeling; meta-analysis
INTRODUCTION
Since a report that the macular hole closure rate was improved by staining the internal limiting membrane (ILM) with indocyanine green (ICG) for better visual identification in macular hole surgery[1-2], several dyes have been widely used as vital stains to make the ILM more visible[3-4]. Because ICG is potentially toxic to retina in high concentrations[5]and visual field defects have also been found after surgery using ICG[6]. Brilliant blue G (BBG) has emerged as an alternative dye which was later found to be more effective in staining the ILM[7]. A few studies[8-14]have ever compared the microstructure and function of eyes with macular hole after ILM peeling using different dyes. The toxicity and safety profiles of the dyes have been investigated to determine which dye is the safest. However, there are no exact conclusions of which one of them is preferred in the surgery of macular hole. We performed a meta-analysis to compare the effect of indocynine green versus brilliant blue G during macular hole surgery.
MATERIALS AND METHODS
Eight kinds of relevant databases, including PubMed (1966-2016), Ovid (1984-2016), ScineceDirect (1990-2016), NGC (Guideline Index) (1998-2016), EBSCO (1975-2016), EMBASE (1984-2016), the Chinese biological medical (CBM) literature on CD-ROM database (1978-2016), China National Knowledge Infrastructure (CNKI) (1995-2016) and Cochrane Central Register of Controlled Trials, were searched. We performed computerized literature searches for relevant available articles published through Jan. 2016. The search included studies published both in the English and Chinese language. Searches comprised a combination of the following key words “indocyanine green”, “brilliant blue G”, “macular hole”, and “internal limiting membrane peeling”. Inclusion criteria comprised: 1) randomized control trials (RCTs), or case control studies; 2) the use of ICG or BBG for internal limiting membrane peel; 3) studies containing sufficient information on BCVA, macular hole closure rate or postoperative complications. Exclusion criteria were: 1) studies with insufficient data; 2) non-controlled study; 3) other adjuvants used for ILM peeling; 4) non-human experiments, 5) short-term (less than three months) studies.
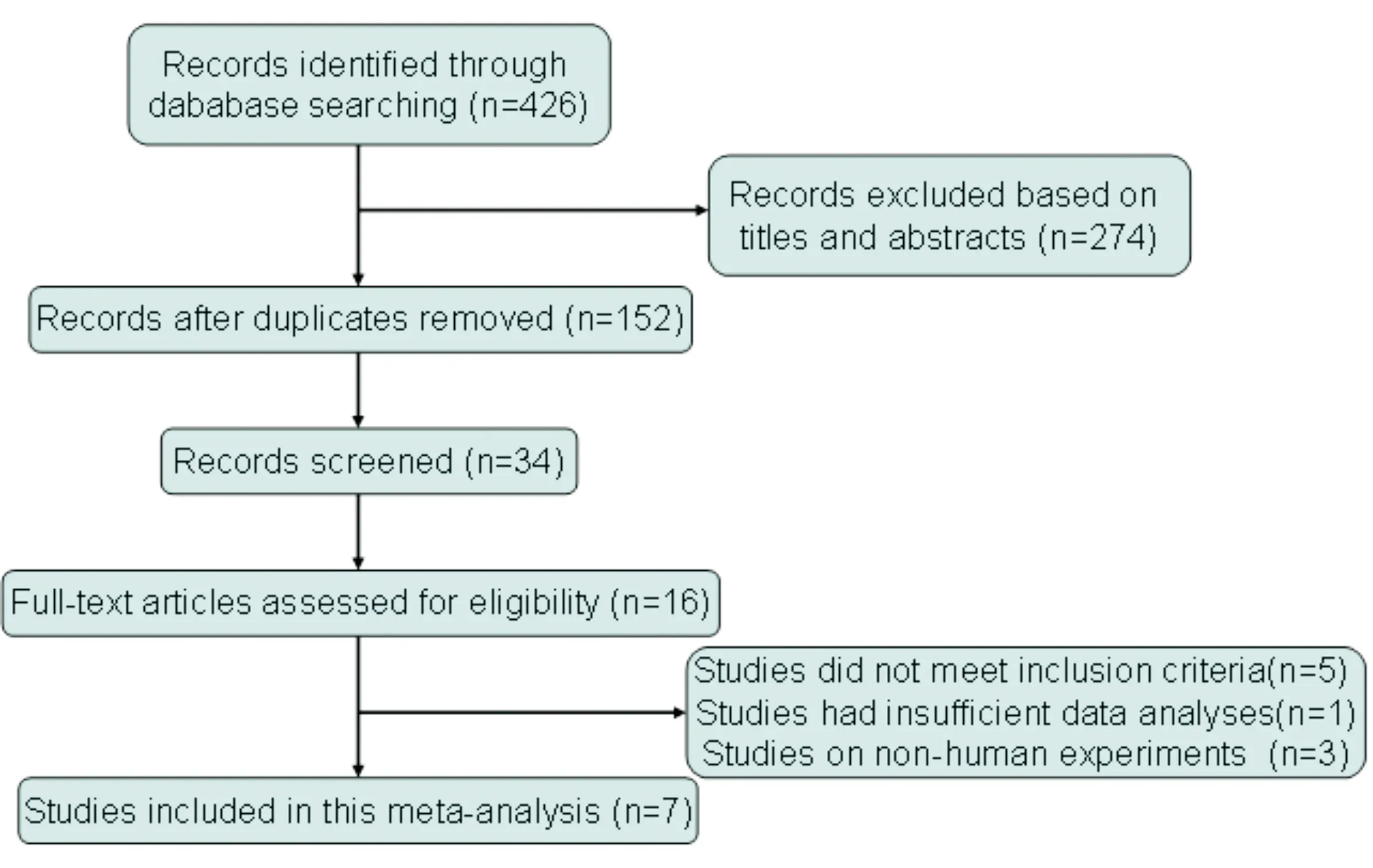
Figure 1 Flow diagram of the study selection formeta analysis.
Document Screeningand Information Extracted The screening was strictly in accordance with inclusion and exclusion criteria. Two reviewers independently screened the studies for eligibility, evaluated the quality and extracted the data from the eligible studies, with confirmation by cross-checking. Divergences of opinion were settled by discussion or consulted by the expert (Jia YD). The lack of information through communicating with the author would be added. Data from the literature included basic information, the patient baseline, interventions, the outcome indicators, the use of statistical methods and results, the author’s conclusions, and so on.
Qualitative Assessment Because randomized control trials and non-RCTs were included in this meta-analysis, the Downs and Black (D&B) quality method, which is appropriate for RCTs and non-RCTs, was used to assess the qualities of the studies[15]. The D&B Scale comprises 27 criteria that evaluate the reporting, external validity, internal validity, selection biases, and power of the studies. Based on quality score, each study is grouped into one of four levels: 26-28, 20-25, 15-19, and ≤14[16]. Higher scores indicate higher quality. Because few studies reported the study’s power, this parameter was omitted. Thus, the quality of each study was considered excellent (21-23), good (15-20), fair (10-14), and poor (≤9) by the two independent reviewers, and disagreements were resolved through discussion with a third reviewer(Zhang LL).
Statistical Methods The statistical software Rev Man 5.3 was used for meta-analysis, recommended by Cochrane Collaboration. For continuous variables, using the same measurement unit, outcomes were analyzed by weighted mean difference(WMD), if not by standardized mean difference (SMD), for dichotomous variables by odds ratio (OR), risk ratio(RR) or risk difference(RD), and 95% confidence interval (CI) should be showed. Chi-square test (α=0.1) was used for heterogeneity test. If homogeneity was found, we used the fixed effect model. If heterogeneity was found, we analyzed the cause of heterogeneity, or proceed to sub-group analysis or sensitivity analysis. Data which could not be incorporated into the meta-analysis adopted descriptive study. The results of meta-analysis were explained by forest plot. The potential publication bias was showed by funnel plot, and was assessed by Egger regression asymmetry test and Begg adjusted rank correlation test.
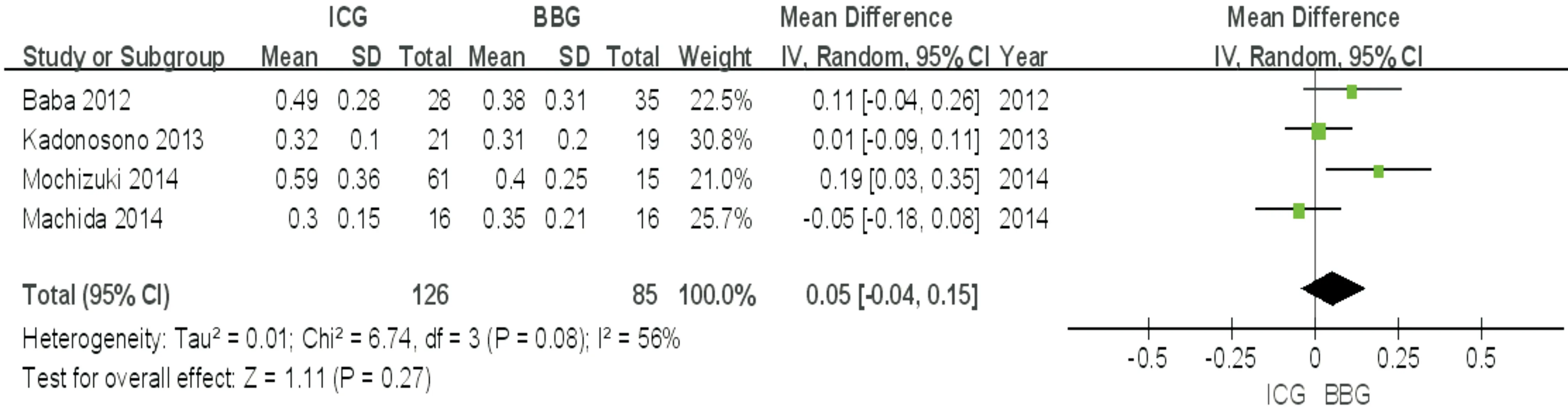
Figure 2 Forest plot from the meta-analysis of BCVA (LogMAR) comparing ICG with BBG at 3mo postoperatively.
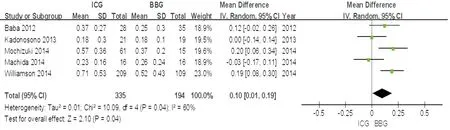
Figure 3 Forest plot from the meta-analysis of BCVA (LogMAR) comparing ICG with BBG at 6mo postoperatively.
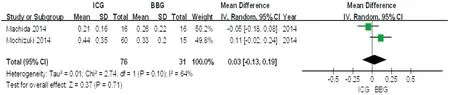
Figure 4 Forest plot from the meta-analysis of BCVA (LogMAR) comparing ICG with BBG at 1y postoperatively.
RESULTS
Literature Search and Results Filter Seven trials included two RCTs[8-9]and five case control trials[10-14], involving a total of 598 eyes, of which 368 eyes underwent vitrectomy with internal limiting membrane peeling using indocyanine green and 230 eyes using BBG (Figure 1).
Comparison on BCVA at 3mo postoperatively between two groups The seven trials included in the study, of which two[13-14]didn’t report BCVA at 3mo postoperatively, one[8]only reported retinal nerve fiber layer thickness after surgery. By ommiting the three trials, the remaining fourtrials[9-12]were included in the meta-analysis. Heterogeneity test:P=0.08, the random-effects model was adopted. The pooled estimate of mean difference (MD) was 0.05, and the 95%CIwas (-0.04, 0.15). The result (Figure 2) suggested that although the average best corrected visual acuity was better in BBG group than in ICG group at 3mo after surgery, but the difference had no statistical significance (P=0.27).
Comparison on BCVA at 6mo postoperatively between two groups Six trials[8-9,11-14]reported BCVA of ICG and BBG group at 6mo postoperatively. But BCVA in one trial[10]reported by Baba T was measured using a decimal visual acuity chart, didn’t been convented to the logMAR units for statistical analysis, therefore a sub-group analysis was performed on other five trials. The pooled estimate of MD was 0.10, and the 95%CIwas (0.01, 0.19). The result (Figure 3) suggested that the average BCVA was better in BBG group than in ICG group at 6mo after surgery, the difference had statistical significance (P=0.04). The result of sub-group analysis was in agreement with that reported by Baba T.
Comparison on BCVA at 1y postoperatively between two groups Of the seven trials included in the study, only two[9,11]trials reported BCVA at 1y postoperatively. The pooled estimate of MD was 0.03, and the 95%CIwas (-0.13, 0.19). The result (Figure 4) suggested that the average BCVA was not significantly different between the two groups at 1y after surgery (P=0.71). As the number of the trials had only two, this result had insufficient evidence which needed further study.
Comparison on macular hole closure rate between two groups Two[8,12]of the seven trials didn’t report macular hole closure rate afer surgery, thus the remaining five trials were included. The five trials[9-11,13-14]all reported the initial closure rate after surgery, one[11]of which reported the final closure rate also. The pooled estimate of relative risk(RR) was 0.95, and the 95%CIwas (0.82, 1.10), Z=0.69,P=0.49, (Figure 5). This suggested that between the ICG and BBG groups, the initial macular hole closure rates weren’t significantly different.
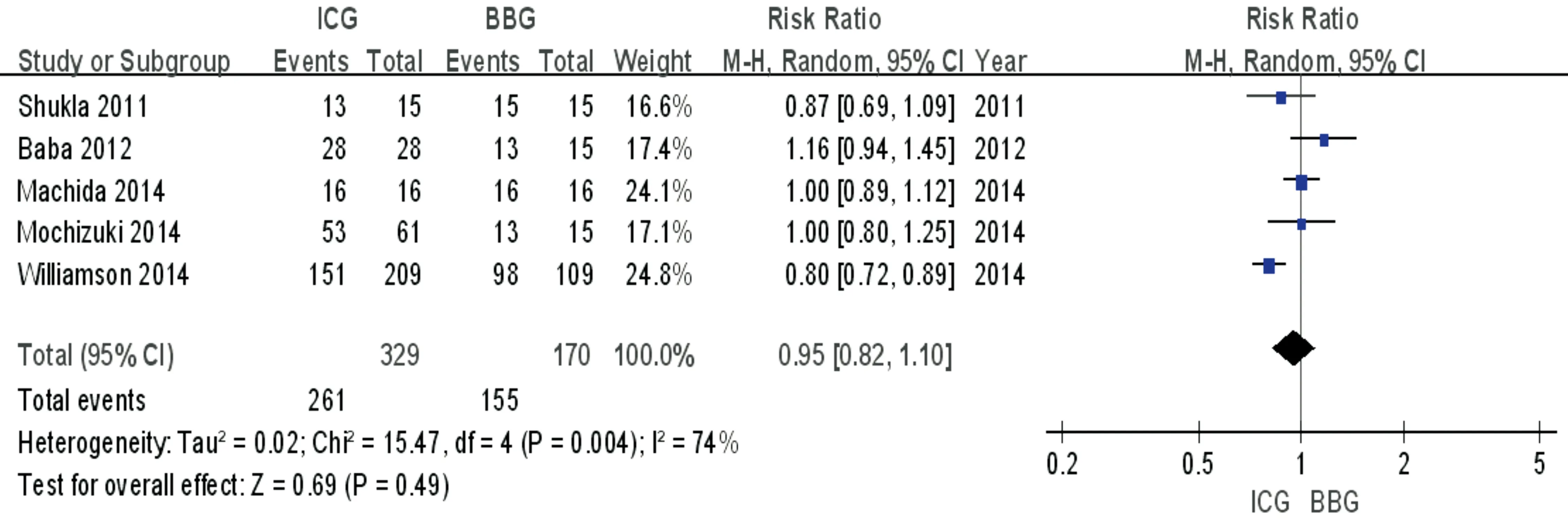
Figure 5 Forest plot from the meta-analysis of macular hole closure rate comparing ICG with BBG postoperatively.
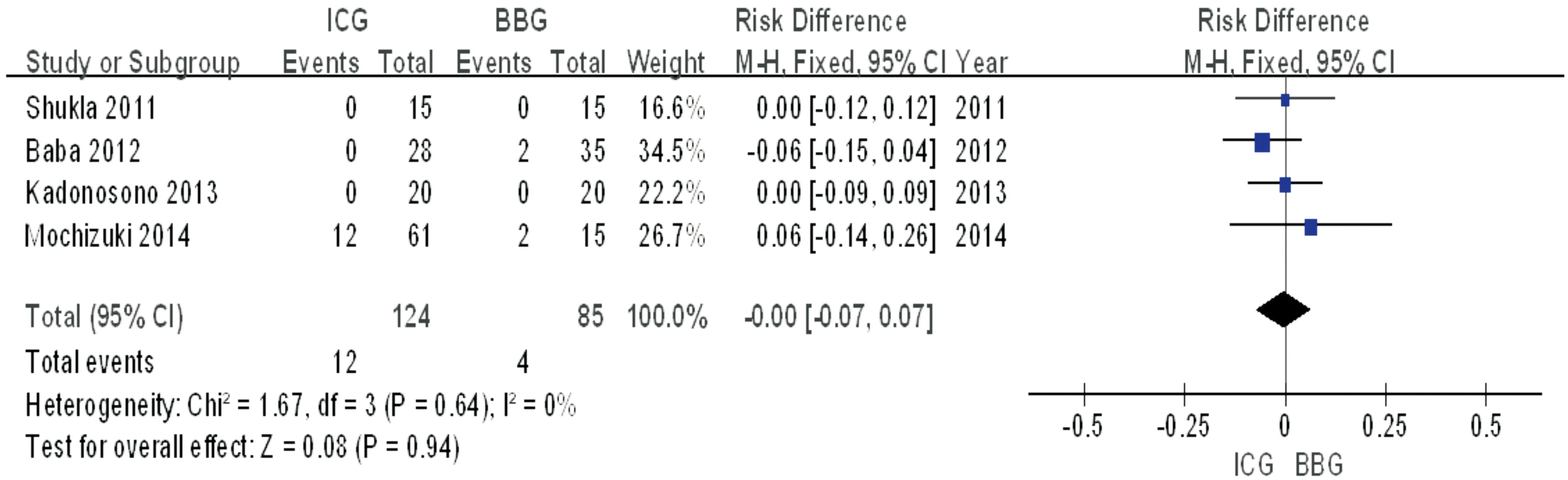
Figure 6 Forest plot from the meta-analysis of adverse events comparing ICG with BBG postoperatively.
Adverse Events Three trials[8-9,13]included in the literature didn’t describe adverse events, and the remaining four trials described adverse events which included retinal detachment, reopening of the macular hole(MH), macular pucker, retinal tear, intraocular hypotension, intraocular hypertension and endophthalmitis. Mochizukietal[11]reported that a retinal tear in the peripheral retina occurred in 2 eyes in BBG group intraoperatively, 11 eyes in ICG group, and reopening of the macular hole occurred in 1 eye in ICG group. Babaetal[10]reported the MH was closed in all cases after the initial surgery in ICG group, and two eyes in BBG group required a second surgery. Shuklaetal[14]and Kadonosonoetal[12]both reported that none of the patients developed any intraoperative or postoperative complications. The four trials[10-12,14]were included in meta-analysis. Heterogeneity test:P=0.64, the fixed-effects model was adopted and the effect size for meta-analysis was RD. The pooled estimate of RD was 0, and the 95%CIwas (-0.07, 0.07),Z=0.08,P=0.94 (Figure 6). The result suggested that compared with BBG group, ICG group had no difference in the incidence of adverse events.
Comparison on retinal nerve fiber layer thickness between two groups Only one trail[8]demonstrated that a transient increase of the retinal nerve fibre layer (RNFL) thickness was seen in the mean overall and sectoral thicknesses except for the nasal/inferior sector at 1mo after surgery in two groups. Then, the thickness gradually decreased and returned to the baseline level in all sectors except for the nasal/inferior sector. The differences in the RNFL thickness between the two groups weren’t significant for at least 12mo postoperatively.
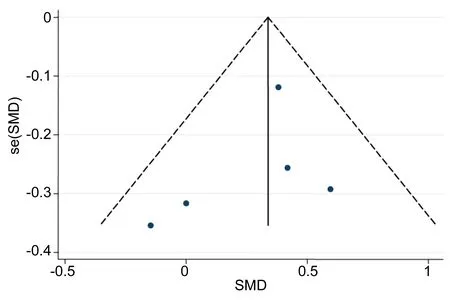
Figure 7 Funnel plot of publication bias.
Publication Bias The publication bias of the study reporting comparison on BCVA at 6mo postoperatively between two groups was shown in the funnel plot (Figure 7). There was no evidence of publication bias (Begg’s test,P=0.142; Egger’s test,P=0.433).
DISCUSSION
Vitrectomy combined with ILM peeling is the main method for the treatment ofidiopathic macular hole (IMH). The application of dyes can improve the resolution of ILM in the operation[17], so that ILM peeling become simple and convenient. ICG is a kind of water soluble dye, which can be combined with type IV collagen and glycoprotein closely. Type IV collagen is the main component of ILM, ICG can effectively dye the ILM pale green, make the border of ILM clear in macular hole surgery[18]. Kadonosonoetal[12]reported that indocyanine green provided a significantly higher contrast ratio than BBG by performing a color contrast ratio analysis. We can get a better visibility of ILM when stained with ICG.
However, fundamental researches have found that ICG was toxic to the retinal pigment epithelial cells, ganglion cells and optic nerve[19]. ICG can not only make the ILM stained, but also penetrate the human retinal epithelium layer and pigment epithelium layer[20]. Cases of visual field defects after ILM staining with ICG were reported[6]. Although the intraocular toxicity of ICG has been recognized, but if the reasonable control of the concentration, osmotic pressure and exposure time, toxicity will be greatly reduced[21]. With the application of advanced surgical equipment and the improvement of surgical experience, the risk of retinal toxicity caused by ICG is greatly reduced. Therefore, ICG is still used in the treatment of IMH. But the toxicity of low concentration ICG on the retina is still inevitable. According to the data collected here, the short-term recovery of BCVA was significantly better in BBG group than in ICG group, especially at 6mo after surgery, as a consequence of the toxicity of ICG on retina which delayed the recovery of visual function.
Moreover, Notomietal[22]reported that photoreceptor apoptosis could be attenuated by BBG, a pharmacologic P2RX7 antagonist that acts by blocking the interaction between extracellular ATP and P2RX7. Pharmacologic inhibition of P2RX7 has been reported to result possibly in neuroprotection of photoreceptors in cases of subretinal hemorrhage[23].These previous reports supported the result of present study that the short-term prognosis of VA was better in the BBG group than in the ICG group.
Although Mochizukietal[11]reported that the magnitude of the improvement at 2y after surgery was significantly better in the BBG group than in the ICG group, but this was a retrospective study ,and sample size was relatively limited. As the number of the long-term trial had only one, this result had insufficient evidence to reach a conclusion.
In this study, the closure rates and intraoperative/postoperative complications didn’t differ between ICG group and BBG group. The diameter of MH and duration of symptoms had been listed as factors affecting the hole closure and visual outcomes[24-25]. The macular hole closure rate and adverse events weren’t significantly related to the type of vital stain. It had also been reported that early inner segment/outer segment (IS/OS) junction restoration affected the prognosis of the postoperative visual acuity[17]. As a result, the use of ICG and BBG appeared to yield similar macular hole closure rate. In addition, only one study[8]demonstrated that the RNFL thickness was significantly increased at 1mo after MH surgery but then decreased to the baseline thickness in two groups. The degree of change of the RNFL thickness was not significantly related to the type of vital stain.
In conclusion, this meta-analysis outcomes revealed that the short-term recovery of the BCVA was significantly better in the BBG group than in the ICG group, especially at 6mo after surgery (P<0.05). The long-term prognosis of BCVA which one study only reported needed further study. There was no significant difference on the macular closure rates and adverse events between two groups (P>0.05). Based on these findings, the results indicated that BBG was preferable to ICG for use during macular hole surgery, which provided clinical practice from evidence-based medicine.
Limitations of this study This meta-analysis only included two randomized control trial(RCT) studies, other five studies were comparative and retrospective case series. We didn’t get unpublished study and sample size was small. The concentration of ICG and BBG, follow-up time and measurement indicators were not totally consistent, which brought many difficulties to data analysis. These factors may cause bias. Because of the existing restrictions, it is suggested that a multi center, large sample, randomized controlled clinical study is required to be conducted, which might provide more convincing evidence for clinical practice.
1 Kadonosono K, Itoh N, Uchio E, Nakamura S, Ohno S. Staining of internal limiting membrane in macular hole surgery.ArchivesofOphthalmology2000;118(8):1116-1118
2 Burk SE, Mata APD, Snyder ME, RosaJr RH, Foster RE. Indocyanine green-assisted peeling of the retinal internal limiting membrane.Ophthalmology2000;107(11):2010-2014
3 Peyman GA, Cheema R, Conway MD, Fang T. Triamcinolone acetonide as an aid to visualization of the vitreous and the posterior hyaloid during pars plana vitrectomy.Retina2000;20(20):554-555
4 Balayre S, Boissonnot M, Curutchet L, Dighiero P. Role of trypan blue in epiretinal membrane surgery.JFrOphtalmol2005;28(3):290-297
5Kernt M, Hirneiss C, Wolf A, Liegl R, Rueping J, Neubauer A, Alge C, Ulbig M, Gandorfer A, Kampik A, Haritoglou C. Indocyanine green increases light-induced oxidative stress, senescence, and matrix metalloproteinases 1 and 3 in human RPE cells.ActaOphthalmol2012;90(6):571-579
6 Yamashita T, Uemura A, Kita H, Nakao K, Sakamoto T. Long-term outcomes of visual field defects after indocyanine green-assisted macular hole surgery.Retina2008;28(9):1228-1233
7 Enaida H, Hisatomi T, Hata Y, Ueno A, Goto Y, Yamada T, Kubota T, Ishibashi T. Brilliant blue G selectively stains the internal limiting membrane/brilliant blue G-assisted membrane peeling.Retina2006;26(6):631-636
8 Toba Y, Machida S, Kurosaka D. Comparisons of retinal nerve fiber layer thickness after indocyanine green, brilliant blue G, or triamcinolone acetonide-assisted macular hole surgery.JFrOphtalmol2013;2014(6):1068-1073
9 Machida S, Toba Y, Nishimura T, Ohzeki T, Murai K I, Kurosaka D. comparisons of cone electroretinograms after indocyanine green-, brilliant blue G-, or triamcinolone acetonide-assisted macular hole surgery.GraefesArchClinExpOphthalmol2014;252(9):1423-1433
10 Baba T, Hagiwara A, Sato E, Arai M, Oshitari T, Yamamoto S. Comparison of vitrectomy with brilliant blue G or indocyanine green on retinal microstructure and function of eyes with macular hole.Ophthalmology2012;119(12):2609-2615
11 Mochizuki N, Yamamoto T, Enaida H, Ishibashi T, Yamashita H. Long-term outcomes of 3 surgical adjuvants used for internal limiting membrane peeling in idiopathic macular hole surgery.JpnJOphthalmol2014;58(6):455-461
12 Kadonosono K, Arakawa A, Inoue M, Yamane S, Uchio E, Yamakawa T, Taguri M, Morita S, Ridgeley JR, Yanagi Y. Internal limiting membrane contrast after staining with indocyanine green and brilliant blue G during macular surgery.Retinal2013;33(4):802-807
13 Williamson TH, Lee E. Idiopathic macular hole:analysis of visual outcomes and the use of indocyanine green or brilliant blue for internal limiting membrane peel.GraefesArchClinExpOphthalmol2014;252(3):395-400
14 Shukla D, Kalliath J, Neelakantan N, Naresh KB, ramasamy K. A comparison of brilliant blue G, trypan blue, and indocyanine green dyes to assist internal limiting membrane peeling during macular hole surgery.Retina2011;31(31):2021-2025
15 Downs SH, Black N. The feasibility of creating a checklist for the assessment of the methodological quality both of randomised and nonrandomised studies of health care interventions.JEpidemiolCommunityHealth1998;52(6):377-384
16 Samoocha D, Bruinvels DJ, Elbers NA, Anema JR, van der Beek AJ. Effectiveness of web-based interventions on patient empowerment: a systematic review and meta-analysis.MedInternetRes2010;12(2):e23
17 Fukuda K, Shiraga F, Yamaji H, Nomoto H, Shiragami C, Enaida H, Ishibashi T. Morphologic and functional advantages of macular hole surgery with brilliant blue G-assisted internal limiting membrane peeling.Retina2011;31(8):1720-1725
18 Ando F, Sasano K, Suzuki F, Ohba N. Indocyanine green-assisted ILM peeling in macular hole surgery revisited.AmJOphthalmol2004;138(5):886-887
19 Sippy BD, Engelbrecht NE, Hubbard GB, Moriarty SE, Jiang S, Aaberg TM Jr, Aaberg TM Sr, Grossniklaus HE, Sternberg P Jr. Indocyanine green effect on cultured human retinal pigment epithelial cells: implication for macular hole surgery.AmJOphthalmol2001;132(3):433-435
20 Penha FM, Pons M, Costa Ede P, Rodrigues EB, Maia M, Marin-Castao ME, Farah ME; International Chromovitrectomy Collaboration. Effect of vital dyes on retinal pigmented epithelial cell viability and apoptosis: implications for chromovitrectomy.Ophthalmologica2013;230(s2):41-50
21 Enaida H, Sakamoto T, Hisatomi T, Goto Y, Ishibashi T. Morphological and functional damage of the retina caused by intravitreous indocyanine green in rat eyes.GraefesArchClinExpOphthalmol2002;240(3):209-213
22 Notomi S, Hisatomi T, Kanemaru T, Takeda A, Ikeda Y, Enaida H, Kroemer G, Ishibashi T. Critical involvement of extracellular ATP acting on P2RX7 purinergic receptors in photoreceptor cell death.AmJPathol2011;179(6):2798-2809
23 Notomi S, Hisatomi T, Murakami Y, Terasaki H, Sonoda S, Asato R, Takeda A, Ikeda Y, Enaida H, Sakamoto T, Ishibashi T. Dynamic increase in extracellular ATP accelerates photoreceptor cell apoptosis via ligation of P2RX7 in subretinal hemorrhage.PLoSOne2013;8(1):e53338
24 Ullrich S, Haritoglou C, Gass C, Schaumberger M, Ulbig MW, Kampik A. Macular hole size as a prognostic factor in macular hole surgery.BrJOphthalmol2002;86(4):390-393
25 Ip MS, Baker BJ, Duker JS, Reichel E, Baumal CR, Gangnon R, Puliafito CA. Anatomical outcomes of surgery for idiopathic macular hole as determined by optical coherence tomography.ArchOphthalmol2002;120(1):29-35
对比吲哚青绿和亮蓝辅助内界膜剥除治疗黄斑裂孔疗效的Meta分析
解传奇1,张令令2,李淑珍1,贾亚丁3
(作者单位:1476000中国河南省商丘市第一人民医院眼科;2476000中国河南省商丘市,商丘医学高等专科学校;3030000中国山西省太原市,山西眼科医院眼科)
解传奇,毕业于山西医科大学,硕士,主治医师,研究方向:眼底病。
解传奇.xiechuanqi0222@163.com
目的:对比术中应用吲哚青绿与亮蓝辅助内界膜剥除对特发性黄斑裂孔术后临床疗效的影响。方法:搜集世界范围内应用吲哚青绿和亮蓝辅助内界膜剥除治疗特发性黄斑裂孔的临床对照试验的英文及中文文献。计算机检索PubMed,Ovid,ScineceDirect,NGC,EBSCO,EMBASE,CNKI,,CBM数据库。由两位系统评价员做独立文献筛查、质量评价和资料提取,并交叉核对,不同意见时经过讨论或请第三者裁决。使用统计软件Rev Man 5.3完成Meta分析。结果:经筛选最后纳入7篇文献,均是以应用吲哚青绿对比亮蓝辅助内界膜剥除治疗特发性黄斑裂孔的临床对照试验,包括受试患者598例,通过比较术后3个主要临床指标:最佳矫正视力,裂孔闭合率和术后并发症,发现亮蓝辅助内界膜剥除组的术后6mo最佳矫正视力高于吲哚青绿组,差别有统计学意义[Z=2.10(P=0.04),OR=0.10,95%CI(0.01,0.19)];在术后裂孔闭合率和并发症方面,两组比较无明显差别(P>0.05)。结论:亮蓝辅助内界膜剥除治疗特发性黄斑裂孔术后短期内视力恢复快,优于吲哚青绿,是较理想的内界膜染色剂。建议进行大样本、长期随访的高质量临床试验,提供更佳的循证医学证据。
吲哚青绿;亮蓝;特发性黄斑裂孔;内界膜剥除;Meta分析
Chuan-Qi Xie. Department of Ophthalmology, First People’s Hospital of Shangqiu, Shangqiu 476000, Henan Province, China. xiechuanqi0222@163.com
10.3980/j.issn.1672-5123.2016.12.04
:Xie CQ, Zhang LL, Li SZ, Jia YD. Comparison of indocyanine green and brilliant blue G to assist internal limiting membrane peeling during macular hole surgery: a systematic review and meta-analysis.GuojiYankeZazhi(IntEyeSci) 2016;16(12):2184-2189
引用:解传奇,张令令,李淑珍,等. 对比吲哚青绿和亮蓝辅助内界膜剥除治疗黄斑裂孔疗效的Meta分析.国际眼科杂志2016;16(12):2184-2189
