Tongguan Liqiao acupuncture therapy improves dysphagia after brainstem stroke
2016-12-02ChunhongZhangJinlingBianZhihongMengLinaMengXuesongRenZhilinWangXiaoyanGuoXueminShi
Chun-hong Zhang, Jin-ling Bian, Zhi-hong Meng, Li-na Meng, Xue-song Ren, Zhi-lin Wang, Xiao-yan Guo, Xue-min Shi,*
1 Department of Acupuncture and Moxibustion, the First Teaching Hospital of Tianjin University of Traditional Chinese Medicine, Tianjin, China
2 Department of Acupuncture and Moxibustion, Tianjin University of Traditional Chinese Medicine, Tianjin, China
RESEARCH
Tongguan Liqiao acupuncture therapy improves dysphagia after brainstem stroke
Chun-hong Zhang1, Jin-ling Bian1, Zhi-hong Meng1, Li-na Meng1, Xue-song Ren1, Zhi-lin Wang2, Xiao-yan Guo2, Xue-min Shi1,*
1 Department of Acupuncture and Moxibustion, the First Teaching Hospital of Tianjin University of Traditional Chinese Medicine, Tianjin, China
2 Department of Acupuncture and Moxibustion, Tianjin University of Traditional Chinese Medicine, Tianjin, China
Graphical Abstract

orcid: 0000-0003-4580-3117 (Xue-min Shi)
Tongguan Liqiao acupuncture therapy has been shown to effectively treat dysphagia after stroke-based pseudobulbar paralysis. We presumed that this therapy would be effective for dysphagia after bulbar paralysis in patients with brainstem infarction. Sixty-four patients with dysphagia following brainstem infarction were recruited and divided into a medulla oblongata infarction group (n = 22), a midbrain and pons infarction group (n = 16), and a multiple cerebral infarction group (n = 26) according to their magnetic resonance imaging results. All patients received Tongguan Liqiao acupuncture for 28 days. The main acupoints were Neiguan (PC6), Renzhong (DU26), Sanyinjiao (SP6), Fengchi (GB20), Wangu (GB12), and Yifeng (SJ17). Furthermore, the posterior pharyngeal wall was pricked. Before and after treatment, patient swallowing functions were evaluated with the Kubota Water Test, Fujishima Ichiro Rating Scale, and the Standard Swallowing Assessment. The Barthel Index was also used to evaluate their quality of life. Results showed that after 28 days of treatment, scores on the Kubota Water Test and Standard Swallowing Assessment had decreased, but scores on the Fujishima Ichiro Rating Scale and Barthel Index had increased in each group. The total efficacy rate was 92.2% after treatment, and was most obvious in patients with medulla oblongata infarction (95.9%). These findings suggest that Tongguan Liqiao acupuncture therapy can repair the connection of upper motor neurons to the medulla oblongata motor nucleus, promote the recovery of brainstem infarction, and improve patient’s swallowing ability and quality of life.
nerve regeneration; traditional Chinese medicine; acupuncture; stroke; bulbar palsy; brain infarction; swallowing disorder; dysphagia; acupoints; neurological rehabilitation; neural regeneration
Introduction
The World Health Organization states that “Stroke is one of the three largest killers and causes of harm to people’s life and health.” A 2014 Health Statistics report showed that stroke was one factor for which years of life lost increased 12% between 2000 and 2012, making it the third largest cause of mortality in the world (WHO, 2014). Among China’s 1.4 billion people, stroke has become the major cause of harm to health and life among the middle-aged and elderly. According to the statistical census data issued by the Ministry of Health, whether urban or rural, the number of deaths caused by stroke has been rising in recent years (Rao et al., 2005).
Dysphagia is a common complication of stroke, causing swallowing disorder, aspiration pneumonia, electrolyte disturbances, and malnutrition. Martino et al. (2005) reported that the incidence rate of dysphagia was 37-78% in the acute period after cerebral apoplexy. Aspiration caused by dysphagia is the main cause of inhalation pneumonia, with pneumonia being the most common complication and major cause of mortality after stroke. Ensuring adequate energy for patients with dysphagia to participate in neurological rehabilitation is difficult. Additionally, extensive hospitalization is required and medical costs rise, which is often seriously deleterious to the quality of life for the patients. Methods for improving dysphagia treatment after stroke and for reducing stroke incidence and disability are therefore urgently needed to solve this major worldwide public health problem.
Currently, clinical treatment of dysphagia includes improving the quality and physical characteristics of food, changing patient posture and position to prevent aspiration, and rehabilitative training. Changes in food and body posture/position are basic treatments for dysphagia (Garcia and Chambers, 2010). A clinical study has shown that adding a thickener to increase food viscosity, eating pasty food, and adjusting head and body posture, can reduce aspiration and increase nutritional intake (Sura et al., 2012), but there is no strong evidence to support thickeners as effective treatment strategies for dysphagia, and no data suggest that postural adjustments can effectively improve swallowing. Rehabilitative therapies for dysphagia include tongue-muscle training, cold stimulation, electrical stimulation, biofeedback, and acupuncture. However, neither cold stimulation nor electrical stimulation has been proven to improve swallowing. A systematic review of 6,779 patients showed that acupuncture and behavior intervention (including swallowing exercises, dietary improvement, environment changes, and postural changes) can improve the swallowing disorder (Geeganage et al., 2012).
In China, acupuncture is an important method for treating swallowing disorders. Shi (2004) confirmed that acupuncture improves the oxygen supply to the impaired brain tissue, which in turn improved the level of oxygen saturation. Our preliminary studies have provided satisfactory proof that Tongguan Liqiao acupuncture therapy for dysphagia after stroke improved patient’s quality of life via improved blood circulation, blood rheology, and arterial blood flow in the base of the skull of stroke-based pseudobulbar paralysis patients (Bian et al., 2005; Li, 2007; Zhang, 2007; Shi et al., 2008; Duan, 2010; Su, et al., 2012). Therefore, acupuncture can increase cranial blood supply, improve oxygen supply to cranial tissues, promote the functional recovery of the central nervous system, rebuild the connection of upper motor neurons to the medulla oblongata motor nucleus, and thus promote recovery from this condition (Bian et al., 2005; Li, 2007; Zhang, 2007; Shi et al., 2008; Duan, 2010; Su, et al., 2012). The purpose of this paper is to increase the observation index and to narrow the infarct size to further observe the clinical effect of Tongguan Liqiao acupuncture therapy for dysphagia after brainstem stroke.
Subjects and Methods
Subjects
Patients were screened using magnetic resonance imaging (MRI) from the Inpatient Department of the First Teaching Hospital of Tianjin University of Traditional Chinese Medicine of China from July 2011 to December 2012. Sixty-four patients were diagnosed with brainstem infarctions, including 47 males and 17 females. The average age was 63.86 ± 9.49 years (range 41 to 86 years). The average course of the disease was 23.9 ± 20.7 days (range 7 hours to 180 days). The patients were categorized into three groups based on their symptoms and radiographic results: infarctions of the medulla oblongata (n = 22), midbrain and pons (n = 16), and brainstem combined with basal ganglia and cortex (n = 26).
This is a prospective cohort study of dysphagia patients after ischemic stroke. All patients were treated with necessary supportive treatments and Tongguan Liqiao acupuncture for 28 days. We compared the efficacy of acupuncture therapy in treating infarctions in different regions (i.e., the three groups). The Ethics Committee of the First Affiliated Hospital of Tianjin University of Traditional Chinese Medicine of China approved this protocol (approval No. TYLL2011[K]002), which followed the principles of the Helsinki Declaration and the Chinese version of the International Conference on Harmonization for Good Clinical Practice. All patients provided informed consent. Baseline characteristics of the 64 patients are shown in Table 1.
Diagnostic criteria
Western medicine has been referring to China’s Diagnosis and Treatment Guidelines for Acute Cerebral Infarction for the diagnosis of stroke (Neurology branch of the Chinese medical association cardiovascular epidemiology group guidelines for writing of diagnosis and treatment of acute ischemic stroke, 2010). Chinese medicine has been referred to as the Criterion of Diagnosis and Therapeutic Effect of Apoplexy (1996) and has been helpful in stroke diagnosis .
The standard for the diagnosis of dysphagia was based on the Practical Applications of Neurology (Shi, 2004), as well as Chinese and Western Clinical Neurology (Wang, 1998). Patients satisfied these diagnostic standards by being conscious, having steady vital signs, not suffering from other neurological diseases, and having radiographic reports showing brainstem infarction.
Inclusion criteriaEvidence of stroke (cerebral infarction) and dysphagia according to the diagnostic criteria, and written informed consent.
Exclusion criteria
Having other diseases that might have caused dysphagia, poor consciousness, psychological problems along with difficulty complying with the doctor, or other primary diseases such as those affecting the liver, kidney, or endocrine system.
Intervention Basic treatment
The necessary supportive treatments were performed according to the Guidelines of Diagnosis and Treatment of Acute Ischemic Stroke in China (2010). These antiplatelet, lipid-lowering, blood-pressure control, and blood-sugar control medications.
Acupuncture
Tongguan Liqiao acupuncture therapy was performed. The main acupoints were Neiguan (PC6), Renzhong (DU26), Sanyinjiao (SP6), Fengchi (GB20), Wangu (GB12), and Yifeng (SJ17). Furthermore, the posterior pharyngeal wall was pricked. Acupuncture was performed using Hwato sterile acupuncture needles (Suzhou Medical Equipment Factory, Suzhou, China) with the dimensions of 0.25 mm × 40.00 mm and 0.30 mm × 75.0 mm, twice a day for 28 days. Needles were maintained in place for 30 minutes.
The bilateral Neiguan (PC6) was needled perpendicularly at a depth of 0.5-1.0 cun (1 cun = 33.3 mm). The first kind of twisting and twirling-reducing manipulation was performed for 1 minute. The main direction of both thumbs when twisting was away from the heart. Next, Renzhong (DU26) was acupunctured, with the needle positioned diagonally upwards towards the nasal septum and inserted at a depth of 0.3-0.5 cun. “Bird-pecking” manipulation was performed until the patient’s eyes teared up. Next, Sanyinjiao (SP6) was acupunctured, with the needle at a 45° angle to the surface of the posterior side of the tibia. The needle was inserted at a depth of 1.0-1.5 cun, and lifting and thrusting-reinforcing manipulation was performed until the patient’s leg jerked three times.
Needles were inserted slowly into Fengchi (GB20), Wangu (GB12), and Yifeng (SJ17) in the direction of the laryngeal prominence at 2.0-2.5 cun. The second type of twisting and twirling-reinforcing manipulation was performed, with a high frequency (120-160 times/min) with small amplitude turns (less than 90°) of the needle for 1 minute, twice daily, until the throat felt sore and distended. Needles were maintained in place for 30 minutes.
The patient was told to open their mouth and their tongue was pressed down using a spatula to fully expose the posterior pharyngeal wall. A 0.3-mm × 75.0-mm needle was used to prick both sides of the posterior pharyngeal wall. This was performed once daily.
Efficacy assessments
The Kubota Water Test, Fujishima Ichiro rating scale and the Standard Swallowing Assessment were used to evaluate swallowing function after 28 days of treatment. The Barthel index was used to evaluate the quality of life.
The Kubota Water Test (Tetsuji, 1997): Patients are asked to drink 30 mL of warm water, and the required time and any choking coughs are observed. Swallowing function is assessed as a score having five levels: level 1 (optimal), can swallow water smoothly; level 2 (good), can swallow more than twice, and does not appear to choke/cough when swallowing; level 3 (medium), swallowing action can be done once, but is accompanied by choke/cough; level 4 (fair), need two or more attempts to complete a swallow, and choke/cough occurs; level 5 (poor), frequent choking coughs and cannot swallow.
The Fujishima Ichiro Rating Scale (Kunieda et al., 2013): This rating scale is used for evaluating swallowing disorders and food nutrition. The scale evaluates swallowing function and recommends the rating of swallowing training required according to whether the patient is ingesting food through the mouth, and whether nutrition supplementation is necessary.
Standard Swallowing Assessment (Ellul and Barer, 1996): This test method was first proposed by Ellul and Barer in 1996. It is a simple and convenient method for clinical screening and evaluation of dysphagia. The assessment consists of three primary steps. Step 1: general examination of consciousness, independent cough, phonation, and the ability to swallow saliva. Step 2: if the patient does not exhibit choking cough or other difficulty swallowing, the patient’s ability to drink from a teaspoon or cup is assessed. If there are two or three normal swallows observed, the following third step is performed. Step 3: the patient drinks a glass of water (approximately 60 mL) and is observed for coughing, choking, and sound quality. A review is carried out within 24 hours to ensure that the diagnosis is correct.
Barthel Index (Mahoney and Barthel, 1965): This index assesses basic activities of daily living or physical ability. A normal total score is 100 points. A “good” score is ≥ 60 points, and indicates that the patient is capable of basic self-care. Moderate dysfunction is defined as a score between 40 and 60, and indicates that the patient needs help in daily life. Severe dysfunction is defined as a score between 20 and 40, and indicates that the patient is significantly dependent on help in daily living. A score below 20 indicates a total disability in which the patient depends on help for all aspects of daily living.
Assessment of results
Results were analyzed using the Kubota Water Test as the standard for assessment. Dysphagia was considered cured if symptoms disappeared and if results from the water test were negative. Treatment was considered significantly effective if a significant improvement in dysphagia was observed along with improvement on the water test by at least two levels. Treatment was considered effective if dysphagia improved and if results on the water test improved by one level. Treatment was considered ineffective if dysphagia did not improve significantly and if no improvement was observed on the water test.
Statistical analysis
All data were statistically analyzed using SPSS 19.0 software(IBM Corp., Armonk, NY, USA). Continuous outcomes are described using the mean ± SD. Dichotomous outcomes are presented as number and percentages of events. Measurements of baseline characteristics were tested using Student’s t-test or the Mann-Whitney U test, depending on the normality of the sampling distribution. Comparison of dichotomous outcomes was performed using chi-square test where appropriate. Results of Kubota Water Test and Fujishima Ichiro rating scale that followed a normal distribution were compared using paired t-test (scores before and after treatment). An independent-samples t-test was used to compare the difference between groups. Results of the Standard Swallowing Assessment and the Barthel Index that were not normally distributed were analyzed using a Wilcoxon test. A two-tailed P < 0.05 was considered statistically significant.

Table 1 Baseline characteristics of 64 patients
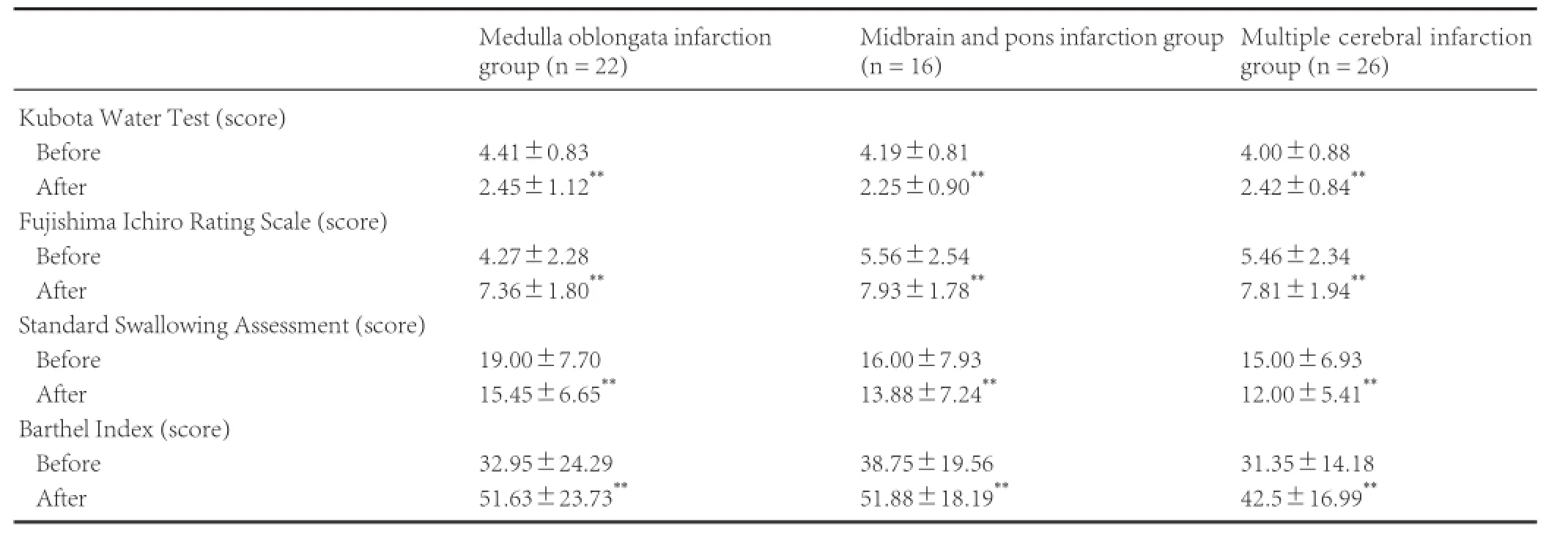
Table 2 Comparison of therapeutic effects in the medulla oblongata infarction, midbrain and pons infarction, and multiple cerebral infarction groups before and after treatment
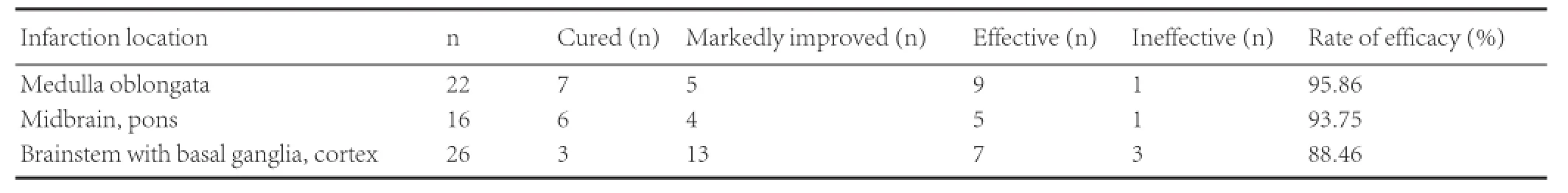
Table 3 Comparison of the Kubota Water Test results in the medulla oblongata infarction, midbrain and pons infarction, and multiple cerebral infarction groups

Figure 1 Head MRI images of a 55-year-old patient.
Results
Tongguan Liqiao acupuncture therapy improved dysphagia in patients with brainstem infarction
Table 1 shows that significant differences in baseline characteristics were not detectable among the three groups (P > 0.05).
As seen in Table 2, we observed significant differences in scores before and after the treatment (P < 0.01). Tongguan Liqiao acupuncture therapy was effective in improving swallowing ability and hastened the recovery of standards of living. We observed no significant differences across the three groups in any of the efficacy assessment tests either before or after Tongguan Liqiao acupuncture therapy.
Table 3 gives the total efficacy rates for the three groups. We found no significant differences across the three groups (P >0.05), but improvement in the medulla oblongata infarction group was the highest (bulbar paralysis). The combined total efficacy rate of the three groups was 92.2%.
Typical case
A 55-year-old male patient was admitted to the hospital because of disability on his right side. He also had had difficulty in speaking and swallowing for the past 18 days. At around 4 a.m. on March 15, 2013, he suddenly experienced a disability on his right side and had difficulty in speaking and swallowing during sleep. At that time, his consciousness was still clear, without headaches, dizziness, chest tightness, breathlessness, or incontinence. He was admitted to Tianjin Huanhu Hospital of China. His MR images (Figure 1) showed a pedunculus cerebellaris medius and medulla oblongata infarction. He was given diuretics, anti-inflammatory drugs, and drugs to improve cranial circulation and to reduce phlegm. He was also given treatment to reduce inter-cranial pressure and hypertension and to remove free radicals. When his condition stabilized, he was admitted to the First Teaching Hospital of Tianjin University of Traditional Chinese Medicine in China on April 2, 2013.
During his admission, the patient’s consciousness was clear and his spirit was good, but his speech was slurred and he had a continuous disability on his right side: his right arm had no voluntary movement and his right leg slid off the surface of the bed. Furthermore, he experienced coughing when drinking water along with difficulty in swallowing. His feeding and urine tubes were clear. Additionally, he had bowel movements once every 2-3 days and the stool was hard. His sleep was normal. He had a 4-year history of hypertension and was taking one Nifedipine Controlled Release Tablet on a daily basis with his blood pressure maintained at approximately 140/100 mmHg (1 mmHg = 0.133 kPa).
During his stay, the patient was given Tongguan Liqiao acupuncture therapy twice a day, at Neiguan (PC6), Renzhong (DU26), Sanyinjiao (SP6), Fengchi (GB20), Wangu (GB12), and Yifeng (SJ17). At the same time, the posterior pharyngeal wall and tongue surface were pricked once a day. After 2 weeks of treatment, the patient was able to ingest lotus-root paste and milk, drank small sips of water using a straw, and spoke more clearly than before. On April 25, 2013, the patient drank water without coughing and could intake as much as 3,000 mL of water. He was able to satisfy his daily energy requirement and his feeding tube was removed on April 26, 2013. His dysphagia was considered clinically cured.
Adverse events
Before the patients were enrolled into acupuncture groups, researchers warned them that subcutaneous bleeding, hematoma, and fainting may occur during acupuncture, and asked the patients to describe any changes after treatment. No adverse events occurred during the course of the study.
Discussion
The pathological changes of dysphagia after stroke, including edema and softening of the ischemic brain region, could cause damage to the cranial nerve motor nuclei that originate in the medulla oblongata, resulting in a bilateral motor-neuron disorder. The medulla oblongata harbors the origin of the hypoglossal nerve (cranial nerve XII) and the glossopharyngeal nerve (cranial nerve IX). Thus, damage can cause central paralysis of the tongue, palate, pharynx, larynx, cheek, and masticatory muscles. These symptoms can present as dysarthria, dysphagia, and emotional disorders (Du et al., 2007).
Dysphagia can be categorized into two types: bulbar and pseudobulbar paralysis. Modern science believes that bulbar paralysis results from demyelination of motor neurons and has a poor prognosis and is irreversible (Huang et al., 2002). However, our study found that acupuncture in the case of bulbar paralysis had some curative effect, with an efficiency that was even higher than the other two groups. This study primarily included patients with brainstem infarction, especially bulbar paralysis after ischemic stroke. According to our results, the total efficacy rate was 95.86% in patients with medullary infarction, 93.75% in those with infarction at the midbrain and pons, and 88.46% in patients with brainstem, basal ganglia, and cortical infarction. All 59 patients showed marked improvement in swallowing ability and quality of life after undergoing the Tongguan Liqiao acupuncture therapy. This acupuncture therapy was effective in treating dysphagia caused by post-stroke bulbar paralysis. The prognosis of stroke patients was associated with the location and size of the lesion. All patients in this study suffered from different levelsof dysphagia due to brainstem infarction. Comparison among the three groups showed that for bulbar paralysis patients, the Kubota Water Test results were higher (i.e., a greater disability) when conditions before the treatment were more serious. After treatment however, they showed a better trend in their recovery. In reference to their radiographic reports, lesions in these patients were at the medulla oblongata, and often pressed against the glossopharyngeal and hypoglossal nerves, thus causing dysphagia. However, the lesion was usually small, so acupuncture effectively improved blood circulation in the brain, helped to swiftly initiate compensatory mechanisms, and achieved good clinical results. Out of the 64 patients, 5 did not show any response to this treatment, possibly because of their multiple lesions, which resulted in larger areas of damage to the brain and poorer prognoses. The other two patients who did not respond to treatment were older, and had a combination of aphasia, pneumonia, malnutrition, and poor overall functional status. In these cases, it was difficult to guarantee enough energy for participation in the recovery of neural function, which might have led to the poorer prognosis, and is consistent with a previous study (Muhle et al., 2015). Our previous study (Shen et al., 2009) showed that Tongguan Liqiao acupuncture therapy improved blood circulation, blood rheology, and arterial blood flow in the base of the skull in patients with strokebased pseudobulbar paralysis.
Renzhong (DU26) is where the meridians of Hand-Yang Ming, Foot-Yang Ming, and Du (GV) converge. It awakens the brain and opens orifices. As a painful stimulus, acupuncture at Renzhong (DU26) can make the body sympathetically contract, thereby increasing cerebral perfusion pressure (Fan et al., 2008), cerebral blood flow, and carotid artery blood flow (Kagstrom et al., 1983). Many people do not understand why we needed to perform the manipulation until the patients’eyes teared. Was it painful for the patients? For this question, we refer to the anatomic location and related Chinese medical literature regarding Renzhong (DU26). We found that Renzhong (DU26) is in the orbicularisoris muscles, surrounded by a branch of the facial nerve and the trigeminal nerve. Stimulating the facial and trigeminal nerves naturally causes the tear reflex. The SuWen·KongGu mentioned that the DU and Ren (GV and CV) meridian branches intersect in the eye. Combined with the Chinese medical theory that “Body fluid is produced when Yang is added to Yin,” the tearing eyes indicates that the Ren meridian and Du (GV) meridian-Qi is motivated and harmonic, and also reflects the Traditional Chinese Medicine theory of “treating the root of disease” (Gao et al., 2012).
After needling Fengchi (GB20), the blood flow in the vertebral artery increased during systole and was sustained for a long period. Simultaneously, the peripheral arterial pressure decreased during diastole, and improved the blood supply in the vertebral artery and brain. Fengchi (GB20) also promoted the collateral building and compensatory mechanisms for dysphagia, and inhibited development of the disease.
Yifeng (SJ17) can stimulate the cerebellar fastigial nucleus, which has an excellent protective effect on the whole brain, increasing blood supply in the damaged region, regulating nitric oxide synthase, inhibiting cell apoptosis, promoting protein synthesis, inducing the swallowing reflex, stimulating the soft palate or posterior pharyngeal wall, strengthening the swallow-related muscle group, and thus improving the ability to swallow (Fu et al., 2002). During clinical trials, we used Tongguan Liqiao acupuncture therapy to treat post-stroke dysphagia. The results showed that Tongguan Liqiao acupuncture therapy was safe and did not have any side effects. Furthermore, Tongguan Liqiao acupuncture therapy improved poststroke dysphagia and blood oxygen saturation levels (Shi et al., 1999).
Tongguan Liqiao acupuncture therapy is based on the principles of Xingnao Kaiqiao, and is especially used to treat poststroke dysphagia. The pathogenesis of stroke is “an obstruction of the brain orifice, hiding of vitality and spirit, and loss of spirit-guided Qi”, and dysphagia is one of the complications. Therefore, the treatment principle is to “regulate the spirit, direct the Qi, nourish the three Yin meridians, and unblock the channels.” Neiguan (PC6) belongs to the pericardium meridian, connects with the Yinwei meridian, calms the mind, and improves the circulation of Qi and blood. Renzhong (DU26) is a convergent point of the Yang Ming meridians, belongs to the Du (GV) meridian that starts from the uterus, and continues upwards to the brain and top of the head. The reducing manipulation method can regulate the Du (GV) meridian, open orifices, nourish the brain, and calm the mind. The meridians of the three-foot Yin connect with the tongue. Therefore, the reinforcing manipulation on these meridians may nourish the kidney, liver, and spleen, as well as invigorate the spleen to clear dampness. We selected Sanyinjiao (SP6), which is a convergent point of the three-foot Yin meridians. Fengchi (GB20) is an important acupoint to treat wind, is a convergent point of the gall bladder and Yangwei meridians, and belongs to the gall bladder meridian. Fengchi (GB20) can calm wind, suppress Yang, improve blood circulation, and clear the head. Fengchi (GB20), Wangu (GB12), and Yifeng (SJ17) belong to the Shao Yang meridians and have regulatory functions. Therefore, these three points together can nourish the brain, open the brain orifice, and regulate Qi. Lianquan (RN23) is where the Yinwei and Ren meridians converge, and is located in the pharynx. Lianquan (RN23) regulates the Qi of Yin meridians, nourishes Yin and the brain, and unblocks the orifices. All these points together might regulate Qi and the mind, balance Yin and Yang, and unblock any obstruction.
We only recorded the lesion locations, but did not evaluate the severity of stroke based on lesion observations. Additionally, the sample sizes were small. Therefore, we could not show any difference in stroke recovery across groups. These limitations could be resolved in future studies by enlarging the sample size, elaborating the observation index, and including a control group so as to better verify the clinical efficacy of Tongguan Liqiao acupuncture therapy for dysphagia after brainstem stroke.
In summary, Tongguan Liqiao acupuncture provides a new way to recover from dysphagia after stroke. This method is simple, safe, is easily accepted by patients, has exact curative effects, does not have side effects, and is worthy of clinical ap-plication.
Acknowledgments: We would like to thank Jin-ting Li from the First Teaching Hospital of Tianjin University of Traditional Chinese Medicine of China for excellent technical support and Professor Jun Li from the First Teaching Hospital of Tianjin University of Traditional Chinese Medicine of China for critically reviewing the paper.
Author contributions: CHZ performed experiments and wrote the paper. JLB provided technical support. ZHM was responsible for administration and supervision. XMS designed research, provided technical support and critical revision of the paper for intellectual content. LNM was responsible for data collection, analysis and interpretation of the data. XSR and XYG performed research and collected data. ZLW was responsible for the translation from Chinese to English. All authors approved the final version of the paper.
Conflicts of interest: None declared.
Plagiarism check: This paper was screened twice using Cross-Check to verify originality before publication.
Peer review: This paper was double-blinded, stringently reviewed by international expert reviewers.
Brandao DM, Nascimento JL, Vianna LG (2009) Evaluation of functional capacity and quality of life of the elderly after ischemic stroke with and without dysphagia. Rev Assoc Med Bras 55:738-743.
Ellul J, Barer D (1996) On behalf ESDB/COSTAR collaborative dysphagia study. Interobserver reliability of a standardized swallowing assessment (SSA) Cerebrovasc Dis 6:152-158.
Foley NC, Martin RE, Salter KL, Teasell RW (2009) A review of the relationship between dysphagia and malnutrition following stroke. J Rehabil Med 41:707-713.
Garcia JM, Chambers Et (2010) Managing dysphagia through diet modifications. Am J Nurs 110:26-33.
Geeganage C, Beavan J, Ellender S, Bath PM (2012) Interventions for dysphagia and nutritional support in acute and subacute stroke. Cochrane Database Syst Rev 10:Cd000323.
Heuschmann PU, Kolominsky-Rabas PL, Misselwitz B, Hermanek P, Leffmann C, Janzen RW, Rother J, Buecker-Nott HJ, Berger K (2004) Predictors of in-hospital mortality and attributable risks of death after ischemic stroke: the German Stroke Registers Study Group. Arch Int Med 164:1761-1768.
Kagstrom E, Smith ML, Siesjo BK (1983) Recirculation in the rat brain following incomplete ischemia. J Cereb Blood Flow Metab 3:183-192.
Kumar S, Wagner CW, Frayne C, Zhu L, Selim M, Feng W, Schlaug G (2011) Noninvasive brain stimulation may improve stroke-related dysphagia: a pilot study. Stroke 42:1035-1040.
Mahoney FI, Barthel DW (1965) Functional evaluation: the barthel index. Maryland State Med J 14:61-65.
Martino R, Foley N, Bhogal S, Diamant N, Speechley M, Teasell R (2005) Dysphagia after stroke: incidence, diagnosis, and pulmonary complications. Stroke 36:2756-2763.
Muhle P, Wirth R, Glahn J, Dziewas R (2015) Age-related changes in swallowing: physiology and pathophysiology. Der Nervenarzt 86:440-451.
Neurology branch of Chinese medical association cardiovascular epidemiology group guidelines for writing of diagnosis and treatment of acute ischemic stroke (2010) Chinese guide of diagnosis and treatment of acute ischemic stroke 2010. Zhongguo Yixue Qianyan Zazhi 4:50-59.
Reza Shariatzadeh M, Huang JQ, Marrie TJ (2006) Differences in the features of aspiration pneumonia according to site of acquisition: community or continuing care facility. J Am Geriatr Soc 54:296-302.
Shi XM, Yang ZG, Zhou JZ, Han JX, Zhang CS, Bian JL, Li Y, Ma CY, Zhang HY (1999) Clinical and experimental studies on acupuncture treatment for 325 cases of false bulbar paralysis. Zhongguo Zhenjiu 19:491-493.
Shi YQ (2004) Practical Neurology. Shanghai: Shanghai Science and Technology Publishers.
Smithard DG, Smeeton NC, Wolfe CD (2007) Long-term outcome after stroke: does dysphagia matter? Age Ageing 36:90-94.
Sura L, Madhavan A, Carnaby G, Crary MA (2012) Dysphagia in the elderly: management and nutritional considerations. Clin Interv Aging 7:287-298.
Tetsuji Y (1997) Dynamic of the 2 stage of swallowing. Int Med 47:20-22.
The Encephalopathy Accident and Emergency Collaborative Group of State Administration of Traditional Chinese Medicine. Criteria of diagnoss and therapeutic effect evaluation for stroke. Beijing Zhongyiyao Daxue Xuebao 1:55-56.
Umapathi T, Venketasubramanian N, Leck KJ, Tan CB, Lee WL, Tjia H (2000) Tongue deviation in acute ischaemic stroke: a study of supranuclear twelfth cranial nerve palsy in 300 stroke patients. Cerebrovasc Dis 10:462-465.
Wang Y (1998) Beijing: China Press of Traditional Chinese Medicine.
Westergren A (2006) Detection of eating difficulties after stroke: a systematic review. Int Nurs Rev 53:143-149.
WHO (2014) World Health Statistics 2014. Geneva.
Zhang JL (2007) Acupuncture treatment on 89 cases of false bulbar paralysis dysphagia. Shanghai Zhongyiyao Daxue Xuebao 41:63.
Copyedited by Phillips A, Robens J, Wang J, Qiu Y, Li CH, Song LP, Zhao M
10.4103/1673-5374.177737 http://www.nrronline.org/
How to cite this article: Zhang CH, Bian JL, Meng ZH, Meng LN, Ren XS, Wang ZL, Guo XY, Shi XM (2016) Tongguan Liqiao acupuncture therapy improves dysphagia after brainstem stroke. Neural Regen Res 11(2):285-291.
Funding: This study was supported by a grant from the Construction of Traditional Chinese Medicine Prevention and Treatment of Apoplexy Comprehensive System, No. 201007002.
Accepted: 2015-11-25
*Correspondence to: Xue-min Shi, tjdrshi@msn.com.
杂志排行
中国神经再生研究(英文版)的其它文章
- Tissue-type plasminogen activator is a modulator of the synaptic vesicle cycle
- Impaired consciousness caused by injury of the lower ascending reticular activating system: evaluation by diffusion tensor tractography
- Considering calcium-binding proteins in invertebrates: multi-functional proteins that shape neuronal growth
- Cardiovascular dysfunction following spinal cord injury
- Practical application of the neuroregenerative properties of ketamine: real world treatment experience
- Exergames: neuroplastic hypothesis about cognitive improvement and biological effects on physical function of institutionalized older persons
