When gastroenteritis isn't: a case report of a 20-yearold male with Boerhaave's syndrome complicated by intra-abdomimal hemorrhage
2016-11-23JamesBairdAlexanderNorinsky
James Baird, Alexander B. Norinsky
1Department of Emergency Medicine, Rowan University SOM Kennedy University Hospital, Stratford, New Jersey, USA
2Department of Emergency Medicine, Rowan University SOM Kennedy University Hospital, Stratford, New Jersey, USA
Corresponding Author: Alexander B. Norinsky, Email: alexnorinsky@gmail.com
When gastroenteritis isn't: a case report of a 20-yearold male with Boerhaave's syndrome complicated by intra-abdomimal hemorrhage
James Baird1, Alexander B. Norinsky2
1Department of Emergency Medicine, Rowan University SOM Kennedy University Hospital, Stratford, New Jersey, USA
2Department of Emergency Medicine, Rowan University SOM Kennedy University Hospital, Stratford, New Jersey, USA
Corresponding Author: Alexander B. Norinsky, Email: alexnorinsky@gmail.com
World J Emerg Med 2016;7(4):303–306
Here we present the case of a 20-year-old male with a known history of an artificial mechanical aortic valve replacement at ages four and twelve, on chronic warfarin therapy, who presented to our community emergency department for the evaluation of vomiting, diarrhea, generalized malaise and abdominal pain. He was seen at a local urgent care for similar symptoms earlier in the day, subsequently discharged with a diagnosis of mild gastroenteritis; however, according to the patient's sister, upon his return home he looked very unwell and she called an ambulance immediately. He stated the vomiting was nonbloody, nonbilious and without a coffee-ground appearance; the diarrhea likewise was nonbloody, nonmelenic, but mucousy. He had chills, but denies recent fevers, urinary complaints, back pain, chest pain, cough, or dyspnea. No recent illnesses, sick contacts, or travel. The patient denied any other medical or surgical history. Importantly, the patient reported no recent adjustments in his warfarin dose, admitted compliance, with last INR 2.1 two days prior to presentation.
He was immediately brought to an examination room for evaluation (ESI level 1) and upon initial presentation was found to be toxic-appearing. Initial vital signs were as follows: blood pressure 88/52 mmHg, pulse rate 138 beats/minute, breathing 32 respirations/minute, a rectal temperature of 94.2 degrees Fahrenheit, and saturating 91% on ambient air. He was ashen, with sunken eyes and dry mucous membranes. Conjunctivae were pale. Cardiopulmonary exam was significant for tachypnea, tachycardia, and a systolic murmur consistent with his history of aortic valve replacement. Abdomen was soft, nondistended, diffusely tender without particular focal tenderness in any quadrant, and hypoactive bowel sounds, without peritoneal signs of guarding, rebound, or rigidity. Rectal examination revealed no gross or microscopic blood. Peripheral pulses were weak but palpable in the radial and femoral arteries. The remaining physical examination was unremarkable.
Given his significant presentation and past medical history, an extensive work-up was immediately undertaken specifically focusing on inflammatory markers, bleeding studies, and imaging of the abdomen. The patient was mentating, had no signs of impending airway or breathing decompensation. Nursing staff was instructed to place two large-bore intravenous lines, with two boluses of warmed normal saline and to cover the patient with a Bair hugger. An emergent bedside ultrasound of the abdomen via RUSH protocol (rapid ultrasound for shock/hypotension) was performed by the emergency physicians, revealing a moderateto-large amount of intra-abdominal free fluid in the splenorenal, hepatorenal, and perivesicular spaces; the inferior vena cava was fully collapsed; the left ventricle was hyperdynamic; there was no evidence of pericardial effusion, abdominal aortic aneurysm or dissection. A bedside chest radiograph revealed no evidence of infi ltrates or pleural effusions, subdiaphragmatic free air, pneumothorax, or any other cardiopulmonary process.
The blood bank was called immediately to initiate massive transfusion protocol, vitamin K was administered intravenously, and prothrombin complex concentrate was ordered. The general surgery service wasconsulted emergently in expectation for an exploratory laparotomy and hemostasis control.
Pertinent laboratory results revealed, amongst other findings, a metabolic acidosis (lactate 10.5 mmol/L), severe anemia (hematocrit 17.8%), and coagulopathy (INR 14.1).
Once the patient was stabilized, computed axial tomography of the chest, abdomen and pelvis with intravenous contrast enhancement was performed (Figures 1 to 5): posterior pneumomediastinum with free fluid seen adjacent to the distal esophagus, a large amount of complex free fluid throughout the abdomen and pelvis (hemoperitoneum), a large hematoma in the left upper quadrant between the stomach and spleen, and thickened small bowel concerning for shock bowel; there was no free air, aneurysm or evidence of blushing to signify an active bleed. Notably, there was no pleural effusion.
The patient was diagnosed with Boerhaave's syndrome.

Figure 1. Axial slices, computed axial tomography of the chest at the level of the upper-lung fi elds (formatted to lung windows). Extrapulmonary air is seen tracking along the right (white arrow) and posterior aspects of the trachea.
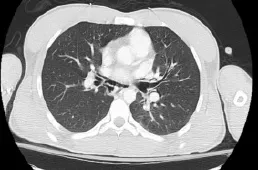
Figure 2. Axial slices, computed axial tomography of the chest at the level of the mid-lung fields (formatted to lung windows). Extrapulmonary air is seen tracking along the bronchiolar tree (white arrow).

Figure 3. Axial slices, computed axial tomography of the abdomen in the upper-abdomen (formatted to mediastinal windows). A large amount of intra-abdominal free fluid around the liver, spleen, and peritoneal cavity.
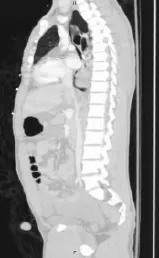
Figure 4. Sagittal slices, computed axial tomography of the chest and abdomen (formatted to lung windows). Posterior pneumomediastinum and pneumoperitoneum extending along the esophagus and stomach walls (black arrow).

Figure 5. Coronal slices, computed axial tomography of the chest and abdomen (formatted to mediastinal windows). A large amount of complex intra-abdominal free fl uid is demonstrated throughout the abdomen and pelvis, with thickened small bowel concerning for shock bowel.
DISCUSSION
Boerhaave's syndrome, as initially described by the namesake physician, is a trans-mural tear of the esophagus secondary to a severe, acute increase in intraluminal pressure. Although it is a rather uncommondiagnosis in the emergency department, the signifi cantly high rate of morbidity and mortality associated with this disease mandates the emergency physician retain a very high index of suspicion in the appropriate clinical context. Immediate intervention must focus on resuscitation as well as minimizing the potentially lifethreatening complications that are often accompanied, including mediastinitis, septic shock, and multi-organ dysfunction. There has been a paucity of literature thus far in the emergency department setting. As yet, there is no unified diagnostic or treatment consensus; the bulk of research focuses on small studies with case and center-specific practices, often with very different patient demographics and illness severity, making statistical analysis and real-world application diffi cult to extrapolate.
Historically, this disease was described in alcoholic patients experiencing bouts of violent emesis; more recently, cases describe patients with a history of peptic ulcer disease or spontaneous ruptures in otherwise healthy people. Our patient would fall in the latter of this group. Pain is retrosternal and excruciating, at times associated with dyspnea or fevers. On examination, they are usually in the shock or peri-shock stage, and with severe distress. Hamman's sign (mediastinal “crackling“) may be present, though not sensitive, specific, or predictive. Mackler's triad (vomiting, lower chest pain, and subcutaneous emphysema) is also unreliable and usually seen late in the disease process.
The most common misdiagnoses are perforated peptic ulcers, myocardial infarction, pancreatitis, pulmonary emboli, and aortic dissection.
Laboratory tests are generally of little value in diagnostics, but nonetheless of important clinical utility in risk-stratifying disease severity and addressing potential complications. For example, our patient's underlying coagulopathy significantly complicated the case and was perhaps the most important driving force in destabilizing him while at the same time expediting his diagnosis and transfer to the operating theater.
Imaging is key. Plain chest radiography is the initial step, but may be normal or nonspecific (up to 15% of the time; this was evident in our case, perhaps given his hyperacute presentation). Relevant findings include extrapulmonary emphysema (e.g. in the mediastinal, intrathoracic or subcutaneous space), pulmonary infiltrates, and/or pleural effusions. One may note air tracking along the left lower mediastinal border and along the left hemidiaphragm, this is often referred to as the “v sign“ or the “Naclerio v sign“ after the physician who initially reported it in 1957.[1]Contrast esophagography with a water-based contrast medium remains the definitive imaging modality of choice, identifying about 90% of intra-thoracic esophageal perforations. However, given its widespread use and ease of access, computed axial tomography has become the initial imaging modality as it assesses the degree of the esophageal tear as well as closely examines the potential associated complications and surrounding structures. The most important fi ndings include peri-esophageal air collections and tracking; thickening of the esophageal wall; pleural effusions and/or infiltrates; peri-aortic air tracking; and, mediastinal fl uid collections.[2]Endoscopy should be approached with extreme caution as it may worsen the esophageal tear.
The majority of tears are found to be in the posterolateral esophageal wall in the lower third of the esophagus, most likely due to a functional weakness there. The average size of the tear is about 2 cm in length.
There remains a great degree of controversy regarding the optimal management of Boerhaave's syndrome.[3]An important determinant is the location of the tear: thoracic perforations usually fare worse and are associated with more systemic complications than intra-abdominal or cervical esophageal perforations. Conservative management, at the minimum, includes strict nil per os with parenteral nutrition supplementation and broadspectrum antibiotic coverage. This is often reserved for the most benign presentation with tiny, contained perforations or the sickest demographic unable to tolerate surgery. Endoscopy is an option as well, although again, must be done with extreme care given the risk of further tearing the esophagus. Some facilities show promising results with endoluminal stents.
For the time being, surgery remains the standard therapy.[4,5]This intervention allows primary repair and addresses the surrounding contamination, infl ammation, and potential necrosis to a better degree than conservative management or endoscopy. There are a number of surgical approaches available depending on the degree of contamination and extent of the tear.[6]Noninvasive procedures include drainage and debridement of the pleura and mediastinum; more extensive surgeries range from video-assisted thoracoscopy to an open thoracotomy. Operative interventions focus on repair, drainage, antibiotics, and an appropriate feeding strategy.[7]Historically a strong prognostic indicator was based on time-to-repair,[8]however newer studies suggest a delayed approach may be just as appropriate.
As yet, there is no standardized protocol for an all-encompassing approach. Spapen et al[9]and de Schipper et al[10]provide excellent algorithms; however, reiterated again is the emphasis for a case-by-case management approach.
Final disposition should be to a higher level of care, i.e. the intensive care unit. A multi-disciplinary approach should include Critical Care, General Surgery, Gastroenterology, and Infectious Disease services.
Our patient's vital signs were stabilized with intravenous fluids and transfusion of multiple blood products in a 1:1:1 ratio of resuscitation for hemorrhagic shock. He was emergently transferred to a tertiary care center for exploratory laparotomy, confirming Boerhaave's syndrome with the distal esophageal tear propagating to the anterior portion of the stomach resulting in laceration of the short gastric artery. The distal esophageal tear was left to heal with conservative management. Henceforth, he was treated with a conservative non-operative approach, and at this time doing well.
This case is interesting in that it underlines several important considerations. Firstly, the use of emergency bedside ultrasonography was key in expediting the care of this patient. Within moments of arrival, a diagnosis was made (large amount of intra-abdominal free fluid) that allowed the prompt consultation of surgical services for defi nitive care. Waiting for advanced imaging studies prior to appropriate disposition in the context of a hemodynamically unstable patient may have disastrous consequences. Secondly, it is interesting to consider whether or not the diagnosis of Boerhaave's syndrome may have been made had the presentation of intraabdominal bleeding not been so significant. In a young man with vomiting and diarrhea for a day, and a benign chest radiograph (i.e. no infiltrate, pleural effusions, or extrapulmonary emphysema), would we have come to the final diagnosis so quickly? It seems as though his warfarin coagulopathy may have been at once his biggest complicating factor and at the same time most important clue leading to the diagnosis. Our review of the literature reveals no similar cases of this very complicated presentation of a young man with Boerhaave's syndrome complicated by a large amount of intra-abdominal hemorrhage secondary to warfarin coagulopathy and laceration of the short gastric artery.
Funding: None.
Ethical approval: Not needed.
Conflicts of interest: The authors declare there is no competing interest related to the study, authors, other individuals or organizations.
Contributors: Baird J proposed the study and wrote the fi rst draft. All authors read and approved the fi nal version of the paper.
REFERENCES
1 Naclerio EA. The “v sign“ in the diagnosis of spontaneous rupture of the esophagus (an early roentgen clue). Am J Surg 1957; 93: 291–298.
2 Ghanem N, Altehoefer C, Springer O, Furtwängler A, Kotter E, Schäfer O, et al. Radiological fi ndings in Boerhaave's syndrome. Emerg Radiol 2003; 10: 8–13.
3 Wolfson D, Barkin JS. Treatment of Boerhaave's Syndrome. Curr Treat Options Gastroenterol 2007; 10: 71–77.
4 Abbas G, Schuchert MJ, Pettiford BL, Pennathur A, Landreneau Ja, Landreneau Jo, et al. Contemporaneous management of esophageal perforation. Surgery 2009; 146: 749–756.
5 Shaker H, Elsayed H, Whittle I, Hussein S, Shackcloth M. The influence of the ‘golden 24-h rule' on the prognosis of oesophageal perforation in the modern era. Eur J Cardiothorac Surg 2010; 38: 216–222.
6 Minnich DJ, Yu P, Bryant AS, Jarrar D, Cerfolio RJ. Management of thoracic esophageal perforations. Eur J Cardiothorac Surg 2011; 40: 931–938.
7 Teh E, Edwards J, Duffy J, Beggs D. Boerhaave's syndrome: a review of management and outcome. Interact Cardiovasc Thorac Surg 2007; 6: 640–643.
8 Brauer RB, Liebermann-Meffert D, Stein HJ, Bartels H, Siewert JR. Boerhaave's syndrome: analysis of the literature and report of 18 new cases. Dis Esophagus 1997; 10: 64–68.
9 Spapen J, De Regt J, Nieboer K, Verfaillie G, Honoré PM, Spapen H. Boerhaave's Syndrome: Still a Diagnostic and Therapeutic Challenge in the 21st Century. Case Rep Crit Care 2013; 2013: 161286.
10 de Schipper JP, Pull ter Gunne AF, Oostvogel HJM, van Laarhoven CJHM. Spontaneous rupture of the oesophagus: Boerhaave's syndrome in 2008: literature review and treatment algorithm. Dig Surg 2009; 26: 1–6.
Accepted after revision August 8, 2016
10.5847/wjem.j.1920–8642.2016.04.012
Letter to the editor
March 22, 2016
杂志排行
World journal of emergency medicine的其它文章
- The state and future of emergency medicine in Macedonia
- Amiodaron in atrial fi brillation: post coronary artery bypass graft
- Short lessons in basic life support improve self-assurance in performing cardiopulmonary resuscitation
- Is current training in basic and advanced cardiac life support (BLS & ACLS) effective? A study of BLS & ACLS knowledge amongst healthcare professionals of North-Kerala
- Effects of a general practitioner cooperative co-located with an emergency department on patient throughput
- Acute Care/Trauma Surgeon's role in obstetrical/ gynecologic emergencies (The OBCAT Alert)