Effect of hormonal contraception on lacrimal gland function
2016-11-04MohamedYasserSayedSaifMohamedAbdelGhafarSayedAhmedTamerSayedSaif
Mohamed Yasser Sayed Saif, Mohamed Abd el Ghafar Sayed, Ahmed Tamer Sayed Saif
·Original article·
Effect of hormonal contraception on lacrimal gland function
Mohamed Yasser Sayed Saif1, Mohamed Abd el Ghafar Sayed2, Ahmed Tamer Sayed Saif3
1Department of Ophthalmology, Beni-Suef University, Beni Suef 62513, Egypt2Obstetrics and Gynecology Department, Beni-Suef University, Beni Suef 62513, Egypt3Department of Ophthalmology, Fayoum University, Fayoum 63514, Egypt
方法:前瞻性随机对照试验。选取60位来自马来西亚贝尼苏夫大学与法尤姆大学医学院的患者随机分为6组(每组10位患者)。第一组:口服复合避孕药;第二组:每月注射复合避孕剂(Mesocept);第三组:注射甲羟孕酮(Depo-Provera);第四组:仅服用黄体酮药片;第五组:皮下埋植(Implanon);第六组:对照组。所有患者均进行全面妇科和眼科检查,包括Schirmer试验和泪膜破裂时间,随访至少3mo。
结果:所有患者的平均年龄为31.03±6.97岁。年龄和孕产次各组之间差异无统计学意义。结果显示:口服复合避孕药干眼患病率最高,其次是每月注射复合避孕剂、注射甲羟孕酮、仅服用黄体酮药片和皮下埋植。对照组无干眼患者。
结论:与仅含有孕激素的避孕方法相比,同时含有雌激素和孕激素的避孕方法导致干眼的可能性更大。
•AIM: To determine the effect of different types of hormonal contraceptives on lacrimal gland function and tear film.
•METHODS: Prospective randomized study was carried out in Faculty of medicine, Beni Suef University and Fayoum University. Sixty patients were divided into 6 groups (each group contain 10 patients): 1) combined oral pills; 2) combined monthly injection; 3) Depo-Provera injection; 4) progesterone only pills; 5) sub dermal Implanon; 6) control. All cases underwent full gynecological and ophthalmological examinations including Schirmer test and tear film break-up time (BUT) and followed up for at least 3mo.
•RESULTS: The mean age of all the patients was 31.03±6.97y. There was no statistical significance between the groups in relation to age, parity and gravidity. The combined pills showed the highest percentage for dry eye followed by Mesocept then Depo-Provera then progesterone only pills then Implanon and no dry eyes in the control group.
•CONCLUSION: Contraceptive methods containing both estrogen and progesterone are more likely to have dry eye than those who used progesterone only contraceptive methods.
dry eyes; hormonal contraceptives; Depo-Provera injection; sub dermal Implanon
INTRODUCTION
There are two types of hormonal contraceptive used: the progestogen-only methods that contain only progesterone or progestin (a synthetic analogue), and the combined methods that contain both estrogen and progestin[1].
While the mechanism of action of progestogen-only contraceptives depends on the progestogen activity and dose, reduce the frequency of ovulation, most of them rely more heavily on changes in cervical mucus[2].
Dry eye disease is a multifactorial disorder involving multiple interacting mechanisms. Dysfunction of any lacrimal functional unit component can lead to the dry eye by causing alterations in the volume, composition, distribution, and clearance of the tear film. Two mutually reinforcing global mechanisms tear hyperosmolarity and tear film instability, have been identified[3].
Tear physiology is affected by hormones from the hypothalamic pituitary gonadal axis, mainly as a result of the influence of sex steroids (androgens, estrogens, and progestins) as well as pituitary hormones. Somewhat dependent on species, the effect of androgen administration is to increase the volume of tears produced by the lacrimal gland and to increase tear protein levels. Estrogen has been shown to diminish tear output whereas progestins have been found to both increase and decrease Schirmer test values and tear film break-up time(BUT) in patients with dry eye[4]. Androgen, estrogen and progesterone receptors mRNAs were reported to be present in the epithelial cells of the lacrimal gland, meibomian gland, lid, palpebral and bulbar conjunctivae, cornea, uveal body, lens, and retina of humans[5].
In addition to the glands responsible for tear production and secretion, it is likely that sex hormones have a direct effect on the tissues of the ocular surface, including the cornea, conjunctiva, and the tear film. Some researchers have demonstrated the key role of the mucin layer, derived primarily from the conjunctival goblet cells is to stabilize the tear film and thus lubricate, hydrate and protect the ocular surface[6]. Moreover, hormonal contraception pregnancy and menopause may be risk factors for dry eye disease due to hormonal changes. Women who receive postmenopausal estrogen replacement therapy are at increased risk of experiencing dry eye disease symptoms[7].
The aim of this study is to determine the effect of different types of hormonal contraceptives on tear film as a cause of dry eye.
SUBJECTS AND METHODS
A prospective randomized study was carried out in Faculty of Medicine; Beni Suef University and Fayoum University included fifty cases taking different types of hormonal contraception for three months and ten case-control.
The Beni Suef University institutional review board approved the study and an informed consents was signed by each individual included in this study.
Inclusion CriteriaFemale between 18y and 50y old accepts taking hormonal method.
Exclusion Criteria1) thromboembolic disease; 2) cerebrovascular disease; 3) breast cancer; 4) pregnancy; 5) hepatic tumor; 6) undiagnosed gynecological bleeding; 7) hypertension; 8) diabetes mellitus; 9) patients with previous ocular surgeries; 10) patients with previous dry eye symptoms or signs; 11) patients with any rheumatological or autoimmune disease; 12) previous ocular trauma or chemical injury.
Cases are divided into: Group 1: ten cases combined oral pills; Group 2: ten cases combined monthly injection; Group 3: ten cases Depo-Provera injection; Group 4: ten cases progesterone only pills; Group 5: ten cases subdermal implants; Group 6: ten cases controls.
Pretreatment EvaluationAll selected patients were submitted to the following before the use of the hormonal contraception. 1) clinical history; 2) general, abdominal and pelvic examination; 3) all cases undergo a full gynecological examination; 4) breast examination; 5) full ophthalmological examinations including visual acuity, intraocular pressure, slit lamp examination and fundus examination using the indirect ophthalmoscope.
Investigations1) pelvic ultrasound to assess: uterine size and dimensions; endometrial thickness; the presence of foci of adenomyosis or fibroids; ovarian size, texture and presence of follicles; 2) hematological investigations: all cases were subjected to the pregnancy test in serum; 3) ophthalmological examination: all cases were subjected to Schirmer test and BUT test in the baseline and follow-up visits during three months.
Tear Film Break-up TimeIn testing for BUT, sodium fluorescein dye is added to the eye and the tear film is observed under the slit lamp while the patient avoids blinking until tiny dry spots develop. Generally, >10s is thought to be normal, 5 to 10s marginal, and <5s low (with high likelihood of dry eye symptoms).
Schirmer TestSchirmer test consists of placing a small strip of filter paper inside the lower eyelid (inferior fornix). The eyes are closed for 5min. The paper is then removed and the amount of moisture is measured. Sometimes a topical anesthetic is placed into the eye before the filter paper to prevent tearing due to the irritation from the paper. The use of the anesthetic ensures that only basal tear secretion is being measured.
Results of the Schirmer test: 1) normal which is ≥15 mm wetting of the paper after 5min; 2) mild which is 14-9 mm wetting of the paper after 5min; 3) moderate which is 8-4 mm wetting of the paper after 5min; 4) severe which is <4 mm wetting of the paper after 5min.
Follow up of the PatientsThe patients were seen 3mo after hormonal contraception use. All cases were subjected to Schirmer test and BUT.
RESULTS
Sixty female subjects were enrolled in the study. The subjects were selected randomly after categorizing the studied females on contraceptive methods into six groups. Ten females represented each group.
ImplanonThe age of the participants ranged from 22 to 43y with a mean 31.30±6.86. The mean parity of this group was 3.5±1.9, and the mean gravidity stood at 3.9±2.96. Schirmer test values of this group of studied females ranged from 4 to 20 mm (16±4.88mm) and BUT values were between 6 to 31s (18.5±7.08s).
Progesterone Only PillsThe age of the participants ranged from 18 to 32y with a mean 24±4.34. The mean parity of this group was 2.5±1.08, and the mean gravidity stood at 2.8±1.03. Schirmer test values of this group of studied females ranged from 3 to 20 mm (12.7±6.27mm) and BUT values were between 2 to 20s (14±5.77s).
Combined PillsThe age of the participants ranged from 19 to 42y with a mean 33.20±7.43. The mean parity of these females was 3.40±1.42 and the mean gravidity stood at 4±1.69. Schirmer test values of this group of studied females ranged from 1 to 18 mm (9.1±6.92 mm) and BUT values were between 2 to 20s (10.6±6.95s).
MesoceptThe age of the participants ranged from 19 to 39y with a mean 28.10±6.64. The mean parity of these females was 2.30±1.15 and the mean gravidity stood at 2.9±1.19. Schirmer test values of this group of studied females ranged from 1 to 20 mm (11.4±7.82 mm) and BUT values were between 3 to 20s (11.4±6.22s).
Table 1The effect of different contraceptive methods on dryness of eye

ParameterContraceptiveMethodsImplanonProgesteroneonlypillsCombinedpillsMesoceptDepo-ProveraControlPTotalSchirmer16.0±4.8812.7±6.279.1±6.9211.4±7.8210.9±6.4219.1±6.350.013BUT18.5±7.0814.0±5.7710.6±6.9511.4±6.2212.2±5.2718.8±6.230.012Dryeye ±ve1(6.7%)a2(13.3%)a5(33.3%)a4(26.7%)a3(20.0%)a0(0.0%)a15(100.0%)a -ve9(20.0%)b8(17.8%)b5(11.1%)b6(13.3%)b7(15.6%)b10(22.2%)b45(100.0%)Total10a,b10a,b10a,b10a,b10a,b10a,b60a,bP0.5a,b0.29a,b0.15a,b0.7a,b0.5a,b
P=0.096;χ2=9.33;aPositive dry eye values;bNegative dry eye values.
Depo-ProveraThe age of the participants ranged from 24 to 44y with a mean 34.3±6.41. The mean parity of these females was 3.30±1.05 and the mean gravidity stood at 3.70±1.15. Schirmer test values of this group of studied females ranged from 1 to 19 mm (10.9±6.42 mm) and BUT values were between 2 to 19s (12.2±5.27s).
Control groupThe age of the participants ranged from 30 to 40y with a mean 35.30±3.16. The mean parity of these females was 2.90±1.19 and the mean gravidity stood at 3.70±1.15. Schirmer test values of this group of studied females ranged from 6 to 30 mm (19.1±6.35 mm) and BUT values were between 6 to 30s (18.8±6.23s).
Precisely, 30 females (50.0%) were using progesterone-only methods (10 Implanon, ten progesterone only pills and 10 Depo-Provera). Twenty females (33.3%) reported using combined estrogen and progesterone methods (10 combined pills and ten Mesocept). Only ten females (16.7%) were using non-hormonal contraceptives.
The distribution of dry eye amongst the studied subjects by the method of contraceptionis shown in Table 1. It is clear that combined pills showed the highest values for dry eye followed by Mesocept and Depo-Provera. On the other hand, of the ten control subjects, none of them had dry eye.
After categorizing the studied females into six different groups according to the contraceptive method, the relation between the different groups and dryness of eye was tested by Chi-square test. None of the studied contraceptive methods were found to be statistically significantly related to dryness of eye (P>0.05). However, those who used combined contraceptive pills showed higher results for dryness of eye followed by Mesocept users then Depo-Provera then Progesterone only pills and Implanon.
The mean age was 31.03±6.97 ranged from 18 to 44y old in the study groups.
Table 2 points to the effect of females’ age, parity and gravidity on the dryness of the eye. As shown, none of these variables was related to dryness of eye (P>0.05). Although subjects with dry eye were older, of lower parity and higher gravidity, these differences were statistically insignificant (P>0.05).
Table 3 shows that the age of subjects, their parity and gravidity constituted have no difference among the 3 mentioned contraceptive methods (estrogen and progesterone, progesterone only and control) (P>0.05). There was a significant difference in BUT and Schirmer test in the combined and progesterone only group from the control group; the combined method shows more dryness than the other group (P<0.05).
Table 2The effect of age, parity and gravidity on dryness of eye
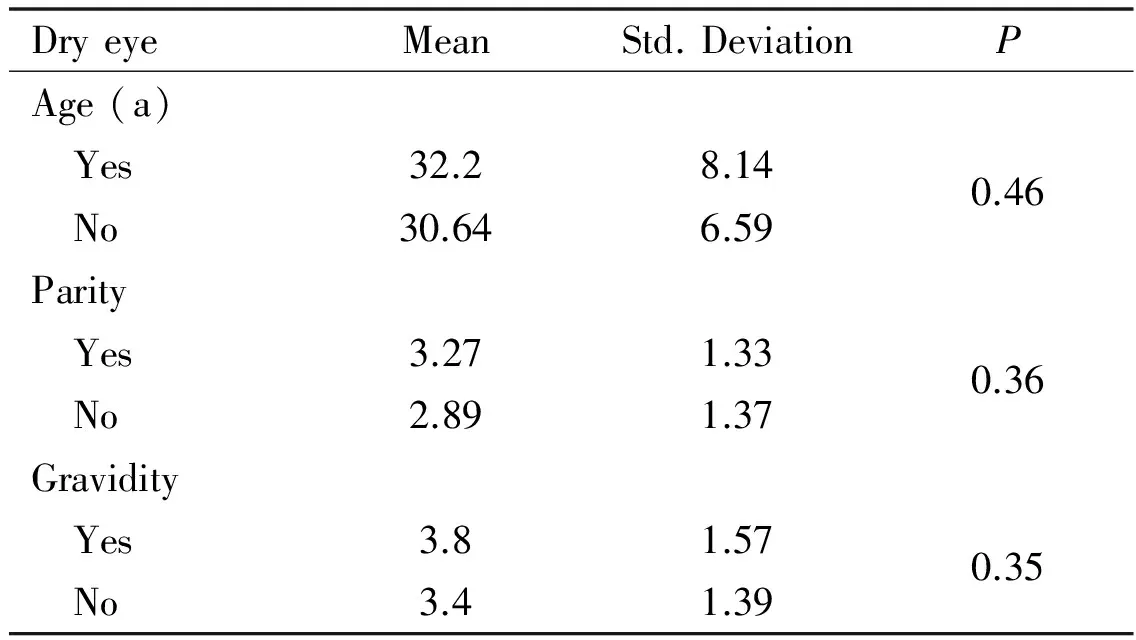
DryeyeMeanStd.DeviationPAge(a) Yes32.28.140.46 No30.646.59Parity Yes3.271.330.36 No2.891.37Gravidity Yes3.81.570.35 No3.41.39
There was a significant difference between the results of Schirmer test and BUT (P<0.05) for eye dryness as shown in Table 4.
DISCUSSION
Dry eye disease is a common multifactorial disease of tears and the ocular surface that can significantly diminish visual function and quality of life. It is one of the leading causes of patient visits to ophthalmologists and optometrists in the United States and affects 5% to 35% of the population[8].
Meibomian gland function is crucial in maintaining the health and integrity of the ocular surface[9]. This gland, through its production and secretion of lipids, promotes the stability and prevents the evaporation of the tear film. Conversely, meibomian gland dysfunction and the resultant lipid insufficiency lead to a decreased stability and an increased evaporation of the tear film[10].
Hormonal contraception refers to birth control methods that act on the endocrine system. Almost all methods are composed of steroid hormones. Hormonal contraception is highly effective when taken on the prescribed schedule. Users of steroid hormone methods experience pregnancy rates of less than 1% per year[11].
There are two main types of hormonal contraceptive formulations. The combined methods that contain both an estrogen and progestin and progestogen-only methods that contain only progesterone or one of its synthetic analogs (progestins). Combined methods work by suppressing ovulation and thickening cervical mucus; while progestogen-only methods reduce the frequency of ovulation. Most of them rely more heavily on changes in cervical mucus[1].
Table 3Relation between age, parity, gravidity, BUT test and Schirmer test and different contraceptive methods
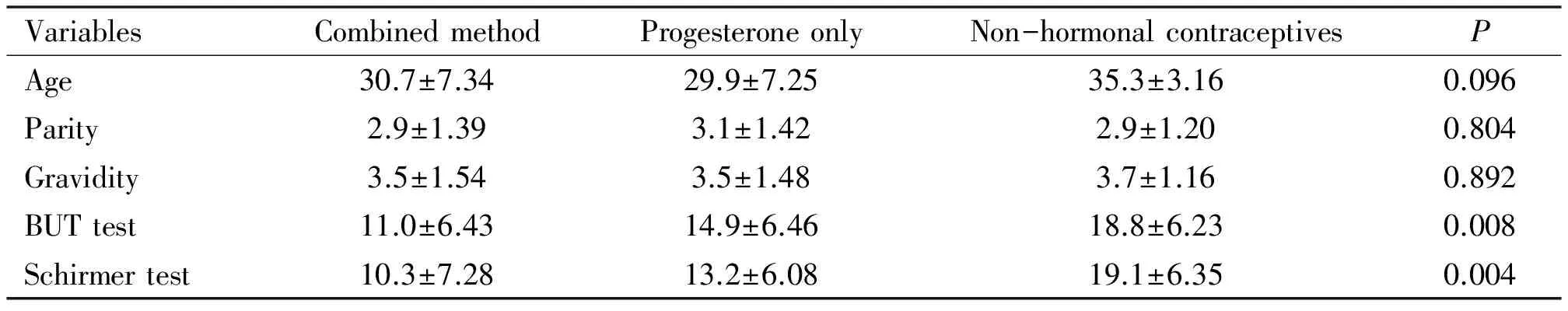
VariablesCombinedmethodProgesteroneonlyNon-hormonalcontraceptivesPAge30.7±7.3429.9±7.2535.3±3.160.096Parity2.9±1.393.1±1.422.9±1.200.804Gravidity3.5±1.543.5±1.483.7±1.160.892BUTtest11.0±6.4314.9±6.4618.8±6.230.008Schirmertest10.3±7.2813.2±6.0819.1±6.350.004
Table 4Schirmer and BUT values results among females with positive and negative dry eyes

DryeyeMeanStd.deviationPSchirmer(mm) Yes2.871.190.001 No16.644.29BUT(s) Yes4.802.110.001 No17.404.59
One of the most compelling features of dry eye syndromes is that they occur predominantly in women raising the inquiry regarding estrogen’s role in dry eye syndrome[8]. The female gender has been termed a risk factor for the development of the dry eye[4,12]. This sex related prevalence is not surprising, given that more than 90 % of the individuals with primary or secondary Sjögren’s syndrome are women[13].
Sex steroid hormones influence many physiological processes in humans, including reproduction, cardiovascular health, bone integrity, cognition, and behavior. Given the widespread role of estrogen in human physiology, it is not surprising that it is also implicated in numerous diseases. Until researchers assumed that the targets for sex hormones are reproductive organs. Investigators have proposed that estrogens play an important role in the anatomy, physiology of the lacrimal gland[14].
The endocrine system exerts significant influences on the physiology and pathophysiology of the lacrimal gland. Androgens, estrogens, and progestin have been identified in the tear film, and their levels in the tears appeared to correlate with those of the serum[15].
However, the relationship between dry eyes and estrogen is complex because it is associated with both low and high estrogen states. So the investigators consider that influence is not only related to estrogen but also related to androgen and other sex hormones in the pathophysiology of dry eye syndrome[16]. Although the influence of androgens may account for most of the sex-related differences found in the lacrimal tissue. The effects of estrogen are still unclear, and the evidence regarding its role is often conflicting[15]. The presence of oestrogen and progesterone receptors in the meibomian glands of human and various animal species suggests that this tissue is predisposed to the influence of female sex hormones[10]. The influence of oestrogen on the meibomian gland appears to antagonise the actions of androgen, with resultant effects on suppression of lipid synthesis and promotion of meibomian gland dysfunction and thus evaporative dry eye[17].
Some studies support observations that dry eye may be associated with estrogen supplementation. In one report, asymptomatic post-menopausal women developed dry eye symptoms after three months of estrogen/progesterone replacement therapy, while symptomatic women were not relieved of dry eye by hormone replacement therapy[18].
Hormonal influences on tear physiology maybe manifested with the use of oral contraceptives, or during menopause when significant changes from the normal hormonal state occur. There are some reports of dry eye symptomatology and intolerance to contact lens wear by women using oral contraceptives[13].
Oral contraceptives containing estrogen might decrease tear volume and reduce BUT. It was also suspected that estrogen oral contraceptives might attenuate mucous production, increase foreign body sensation, decrease visual acuity and increase the risk of dry eyes in women using the drugs[4].
There are controversies about the effects of the hormonal contraceptives on tear physiology and tear production of women. Schaumbergetal[16]reported that the hormone increases the risk of dry eyes in women. Contrary to these investigations, clinical evidence appears to suggest that postmenopausal women with dry eye may benefit from hormone replacement therapy. An improvement in ocular symptoms has been reported with oral and transdermal supplementation with estrogen and estrogen /progesterone[19]. Research found that sex steroids (i.e. androgens, estrogens and progestin) modulate the structural characteristics, functional attributes and pathological features of ocular tissues. These observations had accounted for the gender-related differences in dry eyes[20-21]. Supporting this proposition are the reports that anti-estrogen treatment leads to acinar cell disruption and necrosis, DNA degradation, irritated, reddish and inflamed eyes, loss of tissue in the region where glands are located, dryness of the eye, as well as the correction of such symptoms after the administration of estrogen[22]. In pre-menopausal women, exogenous synthetic estrogen and progesterone for contraceptive use have not been found to affect ocular symptoms, tear volume, BUT or osmolality[20].
Moreover, there were researchers who found that neither estrogen insufficiency nor estrogen treatment has any effect on the morphology, total protein content, specific enzyme activity or secretion of the lacrimal gland[15]
Our prospective randomized study was carried out in Faculty of Medicine, Beni Suef University after approval by internal ethical committee. An informed consent was taken from all patients before the start of the study. We evaluate the effect of hormonal contraception on eye dryness; the study included fifty women using different types of hormonal contraception and ten cases as the control group not using any hormonal method.
Our study found that when we compared each group of hormonal contraception alone to the control group none of the studied contraceptive methods were found to be statistically significantly related to dryness of eye (P>0.05). However, those who used combined contraceptive pills showed higher figures for dryness of the eye. Similarly, Mesocept users showed high rates of dryness of eye of the total subjects with dry eye. Chenetal[20]who carried out a similar study on tear osmolality and dry eye symptoms in women using oral contraception and contact lenses, they reported that neither oral contraceptive pills use nor estrogen dose of the pills appeared to have a meaningful effect on tear osmolality and dry eye symptoms. Frankel and Ellis[23]reported no difference in Schirmer test and BUT between pill users and age-matched controls not taking contraceptives. Tomlinsonetal[24]carried out a similar study on the effects of oral hormonal contraceptives on tear physiology they reported that the oral contraceptives had no effect on normal tear physiology. Iduetal[5]revealed that there were no significant differences in the tear secretion and tear stability between women on injectable hormonal contraceptives and women not using hormonal contraceptives.
On the other hand, Brennan and Efron[25]found that hormonal contraceptives compromise tear physiology. Also Suzukietal[26]found that female sex steroids promote the development of dry eye syndromes and that these hormonal effects involve actions on both the lacrimal and meibomian glands. Liberatietal[27]found that hormonal changes induced by oral contraceptives reduce the peroxidase activity in tears, resulting in a decreased ant oxidative function of the eye, which increases the risk of ocular surface diseases. In fact, a reduced activity of ant oxidative enzymes was observed in patients suffering from dry eye. Sullivanetal[17]demonstrated that testosterone, 17β-estradiol, and progesterone exert multiple effects on the lacrimal and meibomian glands, and these sex steroid effects play a role in the pathogenesis of dry eye syndrome.
We conclude in this study contraceptive methods containing both estrogen and progesterone were more likely to have dry eye than those who used progesterone only contraceptive methods. Also we found that the age, parity, and gravidity were of no effect on the results of the study with no statistical significance between the methods of contaception used.
1 Nelson, Anita L and Cwiak, Carrie "Combined oral contraceptives (COCs)". In Hatcher, Robert A.; Trussell, James; Nelson, Anita L.; Cates, Willard Jr.; Kowal, Deborah; Policar, Michael S. (eds.).Contraceptivetechnology(20th revised ed.). New York: Ardent Media. 2011:249-341
2 Jameson JL, De Groot LJ. Glasier and Anna : "Contraception".Endocrinology(6th ed). Philadelphia: Saunders Elsevier. 2010:2417-2427
3 Askeroglu U, Alleyne B, Guyuron B. Pharmaceutical and herbal products that may contribute to dry eyes.PlastReconstrSurg2013;131(1):159-167
4 Versura P, Giannaccare G,Campos EC. Sex-steroid imbalance in females and dry eye.CurrEyeRes2015;40(2):162-175
5 Idu FK, Emina MO, Ubaru CO. Tear secretion and tear stability of women on hormonal contraceptives.JOptom2013;6(1):45-50
6 Millar TJ, Tragoulias ST, Anderton PJ, Ball MS,Miano F, Dennis GR, Mudgil P. The surface activity of purified ocular mucin at the air-liquid interface and interactions with meibomian lipids.Cornea2006;25(1):91-100
7 Jackson WB. Management of dysfunctional tear syndrome: a Canadian consensus.CanJOphthalmol2009;44(4):385-394
8 Galor A, Feuer W, Lee DJ, Florez H, Carter D, Pouyeh B, Prunty WJ, Perez VL. Prevalence and risk factors of dry eye syndrome in aUnited States veterans affairs population.AmJOphthalmol2011;152(3):377-384.e2
9 Bartlett AH, Bartlett JD. Ophthalmic Procedures for Treatment of Advanced Ocular Surface Diseases.OptomVisSci2015;92(9):939-947
10 Nichols KK, Foulks GN, Bron AJ,Glasgow BJ, Dogru M, Tsubota K, Lemp MA, Sullivan DA. The international workshop on meibomian gland dysfunction: executive summary.InvestOphthalmolVisSci2011;52(4):1922-1929
11 Singh A, Mishra B, Sharma N, Mishra K. Analytical Method Development and Validation for Simultaneous Estimation of Ethinyl Estradiol and Drospirenone By HPLC in Combined Dosage Form.InternatiionallJournallofChemicalandPharmaceuticalAnalysis2014;1(3):80-88
12 Saif MS, Saif AS, Saif PS, El Saftawy HS, Dabbous OA,Salem MN. Evaluation of large cupping in children with anemia.JEgyptOphthalmolSoc2015;108:167-172
13 Tan LL, Morgan P, Cai ZQ, Straughan RA. Prevalence of and risk factors for symptomatic dry eye disease in Singapore.ClinExpOptom2015;98(1):45-53
14 Truong S, Cole N, Stapleton F, Golebiowski B. Sex hormones and the dry eye.ClinExpOptom2014;97(4):324-336
15 Knop E, Knop N, Millar T, Obata H, Sullivan DA. The international workshop on meibomian gland dysfunction: report of the subcommittee on anatomy, physiology, and pathophysiology of the meibomian gland.InvestOphthalmolVisSci2011;52(4):1938-1978
16 Schaumberg DA, Buring JE, Sullivan DA, Dana MR. Hormone replacement therapy and dry eye syndrome.JAMA2001;286(17):2114-2119
17 Sullivan DA, Jensen RV, Suzuki T, Richards SM. Do sex steroids exert sex-specific and/or opposite effects on gene expression in lacrimal and meibomian glands?MolVis2009;15:1553-1572
18 Erdem U, Ozdegirmenci O, Sobaci E, Sobaci G, Göktolga U, Dagli S. Dry eye in post-menopausal women using hormone replacement therapy.Maturitas2007;56(3):257-262
19 Moon JH, Jung JW, Shin KH, Paik HJ. Effect of Hormone Replacement Therapy on Dry Eye Syndrome in Postmenopausal Women: A Prospective Study.JKoreanOphthalmolSoc2010;51(2): 175-179
20 Chen SP, Massaro-Giordano G, Pistilli M, Schreiber CA, Bunya VY. Tear osmolarity and dry eye symptoms in women using oral contraception and contact lenses.Cornea2013;32(4):423-428
21 Amer SAK, Saif MYS, Abd El-Khalek MO, Tawfik A. Prevalence of Dry Eye Syndrome in Beni-Suef Population.CataractandCornea2012;18:2-13
22 Suzuki T, Schirra F, Richards SM, Treister NS, Lombardi MJ, Rowley P, Jensen RV, Sullivan DA. Estrogen’s and progesterone’s impact on gene expression in the mouse lacrimal gland.InvestOphthalmolVisSci2006;47(1):158-168
23 Frankel SH, Ellis PP. Effect of oral contraceptives on tear production.AnnOphthalmol1978;10(11):1585-1588
24 Tomlinson A, Pearce EI, Simmons PA, Blades K. Effect of oral contraceptives on tear physiology.OphthalmicPhysiolOpt2001;21(1):9-16
25 Brennan NA, Efron N. Symptomatology of HEMA contact lens wear.OptomVisSci1989;66(12):834-838
26 Suzuki T, Schaumberg DA, Sullivan BD, Liu M, Richards SM, Sullivan RM, Dana MR, Sullivan DA. Do estrogen and progesterone play a role in the dry eye of Sjögren’s syndrome?AnnNYAcadSci2002;966:223-225
27 Liberati V, de Feo G, Madia F, Marcozzi G. Effect of oral contraceptives on lacrimal fluid peroxidase activity in women.OphthalmicRes2002;34(4):251-253
激素避孕剂对泪腺功能的影响
Mohamed Yasser Sayed Saif1, Mohamed Abd el Ghafar Sayed2, Ahmed Tamer Sayed Saif3
(作者单位:162513埃及贝尼苏夫贝尼苏夫大学眼科;262513埃及贝尼苏夫贝尼苏夫大学妇产科;363514埃及法尤姆法尤姆大学眼科)
Mohamed Yasser Saif. ysaif@sayedsaif.com
目的:探究不同类型的激素类避孕剂对于泪腺功能及泪膜的影响。
干眼;激素类避孕剂;甲羟孕酮注射;皮下埋植
Mohamed Yasser Saif. Department of Ophthalmology, Beni Suef University, 5 Sherif st Babel Louk sq, Cairo 11111, Egypt. ysaif@sayedsaif.com
2015-10-31Accepted: 2016-04-19
10.3980/j.issn.1672-5123.2016.7.02
Saif MYS, Sayed MA, Saif ATS. Effect of hormonal contraception on lacrimal gland function.GuojiYankeZazhi(IntEyeSci) 2016;16(7):1207-1211
引用:Saif MYS, Sayed MA, Saif ATS. 激素避孕剂对泪腺功能的影响.国际眼科杂志2016;16(7):1207-1211