亚临床甲状腺功能减退与冠心病相关性
2016-10-24阿力木江阿不来提徐海蓉
阿力木江·阿不来提,李 渤,张 莉,陈 洋,徐海蓉
亚临床甲状腺功能减退与冠心病相关性
阿力木江·阿不来提1,李渤2,张莉1,陈洋1,徐海蓉1
目的探索亚临床甲状腺功能减退与冠心病相关性。方法选择2013-07至2015-04在我科住院,拟诊冠心病并接受选择性冠状动脉造影患者136例,按甲状腺功能分为甲状腺功能正常组(正常组)和亚临床甲状腺功能减退组(subclinical hypothyroidism, SCH)(减退组)。再根据冠状动脉造影结果分别列入冠状动脉造影阴性组,冠状动脉1支病变、2支病变、3支病变或左主干病变组。比较各组患者的基本资料、生化指标、红细胞总数、红细胞分布宽度、冠状动脉病变数量和Gensini评分,以及超声心动图等资料。结果减退组TC、肌酐水平高于正常组,TG水平低于正常组,差异有统计学意义(P<0.05),而血压、LDL-C、HDL-C、尿素氮、胱抑素、尿酸、FT3、FT4、红细胞总数、红细胞分布宽度等指标间差异无统计学意义。减退组冠心病患者比例与正常组相同,但冠状动脉Gensini评分(18.90±26.07)高于正常组(11.66±15.34),差异有统计学意义(P<0.05)。两组超声指标间未发现差异。结论SCH可能影响冠状动脉病变严重程度。
甲状腺功能减退;亚临床;冠心病
临床上将促甲状腺激素(thyroid stimulating hormone,TSH)水平增高,但游离T3(FT3)、游离T4(FT4)水平正常,且无明显相关症状称为亚临床甲状腺功能减退症(subclinical hypothyroidism, SCH)。SCH在人群中的患病率可达到5%~15%,且随着年龄的增长逐渐上升,在60岁以上女性可达到20%[1,2]。横断面研究证实SCH患者有较高的动脉粥样硬化风险[3]。本研究通过分析SCH和甲状腺功能正常患者的临床资料、冠状动脉造影结果及超声心动图特点,旨在发现冠心病与SCH之间的相关性。
1 对象与方法
1.1对象选择2013-07至2015-04在武警新疆总队医院心内科初诊为冠心病并接受选择性冠状动脉造影患者136例,根据甲状腺功能分为甲状腺功能正常组(正常组)和亚临床甲状腺功能减退组(减退组)。正常组71例,男27例,女44例,其中高血压病35例;减退组65例,男34例,女31例,其中高血压29例。在完善基础临床资料后均接受选择性冠状动脉造影,并根据冠状动脉造影结果分别列入冠状动脉造影阴性组,1支病变、2支病变和3支或左主干病变组并计算Gensini评分。入选标准:(1)年龄大于50岁;(2)排除甲状腺功能减退症(甲减)、糖尿病、痛风等影响糖脂代谢的代谢性疾病;(3)排除了急性冠脉综合征、急性脑卒中等急性心血管疾病和肥厚性心肌病、扩张性心肌病、心脏瓣膜病、先天性心脏病等其他结构性心血管系统疾病。两组患者一般情况对比,差异无统计学意义,除减退组TSH水平高于正常组(P<0.05),其余甲状腺功能指标间无差异,符合分组条件。见表1。

表1 两组患者基本情况比较
1.2方法
1.2.1采样患者清晨空腹抽取静脉血9 ml,分装3个试管。分别进行:(1)采用全自动免疫分析系统检测游离三碘甲状腺原氨酸(FT3)、游离甲状腺素(FT4)、促甲状腺激素(TSH),参考值范围,FT33.06~6.73 pmol/L、FT411.99~21.91 pmol/L、TSH 0.27~4.2 mU/L;(2)血脂分析,包括三酰甘油(TG)、总胆固醇(TC)、低密度脂蛋白胆固醇(LDL-C)、高密度脂蛋白胆固醇(HDL-C))、血糖、肌酐、尿素氮、尿酸等指标检测;(3)进行血常规检测,比较红细胞总数、红细胞分布宽度等指标。
1.2.2选择性冠状动脉造影采用荷兰Philip 公司生产的血管造影机,经桡动脉途径用TIG多功能造影导管选择多体位行左、右冠状动脉造影。造影结果由2名介入医师独立诊断。根据1984年美国心脏病协会规定的冠状动脉血管图像分段评价标准和Gensini评分系统对每支血管狭窄程度进行定量评价:狭窄程度<50% 或显示正常者为阴性,≥50% 者列入冠心病组。根据狭窄累及血管数量分为1支、2支和3支或左主干病变。Gensini评分系统:狭窄程度﹤25%为1分,26%~50%为2分,51%~75%为4分,76%~90%为8分,91%~99%为16分,100%闭塞为32分。不同节段冠状动脉评分系数:左主干病变计分×5,左前降支近段×2.5,中段×1.5,远段×1,第一对角支×1,第二对角支×0.5,左回旋支近段×2.5,远段×1,右冠状动脉近段,中段,远段均×1,后降支×1,后侧支×0.5。将各分支积分相加得出冠状动脉病变程度的Gensini评分。所用对比剂均为非离子型对比剂(碘帕醇)。
1.2.3超声心动图检查采用西门子Acuson Sequoia 512彩色多普勒超声心动图仪,探头频率3~8 MHz,对136例患者进行常规超声心动图检查。由一名技师负责操作,以减少操作者误差。

2 结 果
2.1生化指标及Gensini评分由表2可见,减退组TC高于正常组,TG水平低于正常组,差异有统计学意义(P<0.05),LDL-C和HDL-C水平差异无统计学意义,提示减退组血脂异常。减退组肌酐水平高于正常组(P<0.05),提示减退组肾功能损害比较明显。减退组Gensini评分高于正常组(P<0.05),提示减退组冠状动脉病变严重程度高于正常组。

表2 两组冠心病患者生化指标及Gensini评分比较 ±s)
2.2冠状动脉造影结果比较甲状腺功能正常组和减退组患者冠状动脉造影结果,无论是1支、2支、3支还是左主干病变,两组患者比例相同,差异无统计学意义(表3)。
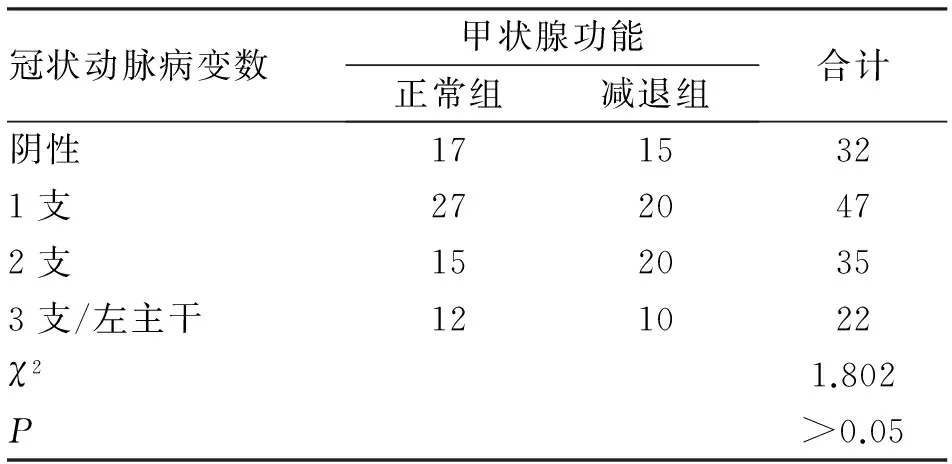
表3 两组冠心病患者冠状动脉造影结果比较 (例)
2.3超声心动图指标两组患者超声资料,无论是心脏结构参数还是心脏功能参数之间无统计学差异(表4)。

表4 两组冠心病患者超声心动图指标比较 ±s)
3 讨 论
心血管系统是甲状腺激素的特定靶器官之一。SCH与冠心病相关性研究报道存在矛盾[4-7]。Rotterdam[3]发现,SCH是老年女性发生动脉粥样硬化和心肌梗死的独立危险因素。Kvetny等[5]提出,SCH可以预测50岁以下男性心血管疾病发病风险。但Hyland等[6]随访5888例年龄≥65岁的SCH患者,10年后发现由冠心病、心力衰竭和心血管疾病引起的死亡并没有增加。Pearce等[7]甚至提出,SCH患者全因病死率低于甲状腺功能正常者。虽然存在争议,但更多的学者认为SCH与冠心病有一定相关性。SCH通过多种途径增加冠心病发病危险。SCH患者胆固醇、低密度脂蛋白水平、血压、胰岛素抵抗程度等高于甲状腺功能正常者[8-10]。Tseng等[10]发现,TSH水平在5.0~9.9 mU/L的SCH患者心血管病死亡风险明显增加,特别是在老年患者中这种关联更强。血脂异常、舒张压升高、周围血管阻力增加、内皮依赖性血管舒张因子减少、凝血功能异常、高C反应蛋白和高同型半胱氨酸水平等因素可能与SCH增加心血管疾病风险有关[11]。本研究采用了诊断冠心病金标准的冠状动脉造影检查,严格入选标准,特别排除了可能成为混杂因素的临床甲减和糖尿病等患者,平衡了性别、年龄等指标,结果提示SCH患者冠状动脉狭窄程度较甲状腺功能正常者明显,与以上研究一致。血脂异常是公认的冠心病危险因素。与甲状腺功能正常患者相比,SCH患者血脂水平高于正常者[9,12],但是具体哪些血脂指标之间有差别报道不一。Liu等[9]荟萃分析发现,SCH患者TG、TC、LDL-C水平高,但HDL-C水平无差别。本研究发现,减退组TC水平(3.90±1.63)mmol/L高于甲状腺功能正常组(2.50±1.63)mmol/L,TG水平低于正常组,HDL-C和LDL-C水平无差异。研究方法和研究人群的不同可能是出现这种差异的原因。理论上认为,甲状腺功能减退引起的主动脉硬化、外周血管阻力增大,可能导致高血压,特别是舒张压的升高,但实际上这方面的研究结果存在矛盾[13,14]。本研究未发现两组患者血压水平存在差异,但不除外患者均已服用降压药物等因素的可能。
减退组患者肌酐水平高于甲状腺功能正常患者。慢性肾脏病患者中大约18%有SCH,且SCH与eGFR进行性下降独立相关[15]。慢性肾功能不全往往与高龄、高血压、糖尿病等冠心病危险因素伴发,同时存在炎性反应、内皮功能异常、凝血因子激活等冠状动脉粥样硬化的共同机制。肾功能不全也是冠心病的独立危险因素之一[16,17]。甲状腺功能减退时血液黏稠度增加,血流速度减慢、肾脏血流减少都有可能影响肾功能。SCH不仅与冠心病发生相关,而且与严重程度也有关。冠心病高危患者如果合并SCH则冠状动脉狭窄更严重[18],冠状动脉钙化积分更高[19]。Silva等[20]发现,Framingham危险评分≥10%的人群中SCH者冠状动脉钙化积分高于甲状腺功能正常者。本研究发现,减退组患者冠状动脉Gensini评分(18.90±26.07)分明显高于甲状腺功能正常组(11.66±15.34)分,提示SCH与冠心病严重程度有关。
有研究提示,SCH患者左室舒张功能、心室腔均受到影响[21,22]。但本研究比较两组心脏超声心动图,结果显示减退组超声指标与甲状腺功能正常组差异无统计学意义。可能与本研究不同的测量指标及样本量较少等因素有关。红细胞分布宽度是反映红细胞大小差异性的一项指标,反映红细胞体积的离散程度,既往主要用于贫血的诊断和鉴别诊断,以及形态学分类。目前,RDW与冠心病特别是急性冠脉综合征之间的相关性被广泛关注[23,24]。本研究发现两组患者红细胞分布宽度之间差异无统计学意义,可能与本研究排除了急性冠脉综合征的患者、样本量少,以及横断面研究的缺陷等因素有关。
综上所述,冠心病的发生、发展归因于高血压病、糖尿病、血脂异常及高尿酸血症等综合危险因素的共同作用。SCH患者往往存在三种以上代谢综合征危险因素[25],也有人认为,SCH可能是代谢综合征危险因素之一[26]。本研究认为,对有代谢综合征或冠心病危险因素的患者进行甲状腺功能筛查可能具有积极的治疗和预后意义。目前,对SCH与冠心病相关性证据逐渐增多,但争论依然未停息,特别是TSH水平低于10 mU/L的患者是否需要治疗方面争议颇大,仍需要大规模临床试验来回答、证实。
[1]Hollowell J G, Staehling N W, Flanders W D,etal. Serum TSH, T(4),and thyroid antibodies in the United States population (1988 to 1994):National Health and Nutrition Examination Survey (NHANES III)[J]. J Clin Endocrinol Metab, 2002, 87(2):489-499.
[2]Surks M I, Ortiz E, Daniels G H,etal. Subclinical thyroid disease: scientific review and guidelines for diagnosis and management[J]. JAMA, 2004, 291(2):228-238.
[3]Monzani F, Caraccio N, Kozakowa M,etal. Effect of levothyroxine replacement on lipid profile and intima-media thickness in subclinical hypothyroidism: a double-blind, placebo- controlled study[J]. J Clin Endocrinol Metab, 2004, 89(5):2099-2106.
[4]Hak A E, Pols H A, Visser T J,etal. Subclinical hypothyroidism is an independent risk factor for atherosclerosis and myocardial infarction in elderly women: the Rotterdam Study[J]. Ann Intern Med, 2000, 132(4):270-278.
[5]Kvetny J, Heldgaard P E, Bladbjerg E M,etal. Subclinical hypothyroidism is associated with a low-grade inflammation, increased triglyceride levels and predicts cardiovascular disease in males below 50 years[J]. Clin Endocrinol, 2004, 61 (2):232-238.
[6]Hyland K A, Arnold A M, Lee J S,etal. Persistent Subclinical hypothyroidism and cardiovascular risk in the elderly: The Cardiovascular Health Study [J]. J Clin Endocrinol Metab, 2013,98(2): 533-540.
[7]Pearce E N, Selmer C, Olesen J B,etal. Overt and subclinical hyperthyroidism are associated with increased mortality whereas subclinical hypothyroidism is associated with decreased mortality[J]. Clin Thyroidol, 2014, 26(5):120-122.
[8]Luboshitzky R, Aviv A, Herer P,etal. Risk factors for cardiovascular disease in women with subclinical hypothyroidism[J]. Thyroid, 2002, 12(5):421-425.
[9]Liu X L, He S, Zhang S F,etal. Alteration of lipid profile in subclinical hypothyroidism: a meta-analysis[J]. Med Sci Monit, 2014, 20(20):1432-1441.
[10]Tseng F Y, Lin W Y, Lin C C,etal. Subclinical hypothyroidism is associated with increased risk for all-cause and cardiovascular mortality in adults [J]. J Am Coll Cardiol, 2012, 60(8):730-737.
[11]Biondi B, Cooper D S. The clinical significance of subclinical thyroid dysfunction[J]. Endocr Rev, 2008,29(1):76-131.
[12]Xu C, Yang X, Liu W,etal. Thyroid stimulating hormone, independent of thyroid hormone, can elevate the serum total cholesterol level in patients with coronary heart disease: a cross-sectional design[J]. Nutr Metab (Lond),2012,9(1):44.
[13]Liu D, Jiang F, Shan Z,etal. A cross-sectional survey of relationship between serum TSH level and blood pressure[J].J Hum Hyper, 2010, 24(2):134-138.
[14]Ferreira M M, Teixeira Pde F, Mansur V A. Ambulatory blood pressure monitoring in normotensive patients with subclinical hypothyroidism [J]. Arq Bras Cardiol, 2010, 94(6):806-812.
[15]Chonchol M, Lippi G, Salvagno G,etal. Prevalence of subclinical hypothyroidism in patients with chronic kidney disease[J]. Clin J Am Soc Nephrol, 2008, 3(5):1296-1300.
[16]Manjunath G, Tighiouart H, Ibrahim H,etal. Level of kidney function as a risk factor for atherosclerotic cardiovascular outcomes in the community[J]. J Am Coll Cardiol,2003,41(1):47-55.
[17]Sarnak M J, Levey A S, Schoolwerth A C,etal. Kidney disease as a risk factor for development of cardiovascular disease. A statement from the American Heart Association Councils on kidney in cardiovascular disease, high blood pressure research, clinical cardiology, and epidemiology and prevention[J]. Circulation,2003,108(17):2154-2169.
[18]Bai M F, Gao C Y, Yang C K,etal. Effects of thyroid dysfunction on the severity of coronary artery lesions and its prognosis [J]. J Cardiol,2014,64(6):496-500.
[19]Park Y J, Lee Y J, Choi S I,etal. Impact of subclinical hypothyroidism on the coronary artery disease in apparently healthy subjects[J]. Eur J Endocrinol, 2011, 165(1):115-121.
[20]Silva N, Santos O, Morais F,etal. Subclinical hypothyroidism represents an additional risk factor for coronary artery calcification, especially in subjects with intermediate and high cardiovascular risk scores[J]. Eur J Endocrinol, 2014,171(3):327-334.
[21]Tadic M, Ilic S, Kostic N,etal. Subclinical hypothyroidism and left ventricular mechanics: a three-dimensional speckle tracking study[J]. J Clin Endocrinol Metab, 2014, 99(1):307-314.
[22]Chen X, Zhang N, Cai Y,etal. Evaluation of left ventricular diastolic function using tissue Doppler echocardiography and conventional doppler echocardiography in patients with subclinical hypothyroidism aged <60 years: a meta-analysis[J]. J Cardiol, 2013,61(1):8-15.
[23]Dabbah S, Hammerman H, Markiewies W,etal. Relation between red cell distribution width and clinical outcomes after acute myocardial infarction[J]. Am J Cardiol, 2010,105(3):312-317.
[24]Lippi G, Filippozzi L, Motagnana M,etal. Clinical usefulness of measuring red blood cell distribution width on admission in patients with acute coronary syndromes[J]. Clin Chem Lab Med, 2009, 47(3):353-357.
[25]Ashizawa K, Imaizumi M, Usa T,etal. Metabolic cardiovascular disease risk factors and their clustering in subclinical hypothyroidism[J]. Clin Endocrinol (Oxf), 2010, 72(5):689-695.
[26]Nakajima Y, Yamada M, Akuzawa M,etal. Subclinical hypothyroidism and indices for metabolic syndrome in Japanese women: one-year follow-up study[J]. Endocrinol Metab, 2013,98(8):3280-3287.
(2015-08-10收稿2015-12-18修回)
(责任编辑郭青)
Relationship between subclinical hypothyroidism and coronary artery disease
ABULAITI Alimujiang1, LI Bo2, ZHANG Li1, CHEN Yang1, and XU Hairong1.
1.Department of Cardiology, Xinjiang Uigur Autonomous Region Corps Hospital, Chinese People’s Armed Police Force, Urumqi 830091, China;2. Health Team, 5th Detachment of Xinjiang Uigur Autonomous Region, Chinese People’s Armed Police Force, Hetian 844000, China
ObjectiveTo evaluate the relationship between subclinical hypothyroidism(SCH) and coronary artery disease. Methods136 patients admitted from July 2013 to April 2015 were recruited for the study. Clinical data including age, gender, blood pressure, thyroid function, blood sugar, lipid profiles,red blood cell counts, and red cell distribution width(RDW) were analyzed. All patients received selective coronary angiography. Based on results of coronary angiography, they were categorized into one, two, three or left main artery stenosis groups and angiographic normal group. Clinical characteristics, coronary angiography, Gensini scores and echocardiographic parameters were compared. ResultsTC, serum creatine levels were higher and TG were lower in SCH group(P<0.05);blood pressure, LDL-C,HDL-C, urea, cystatin-C, uric acid, FT3,FT4,red blood cells,and RDW levels were not different between the groups. Number of coronary artery disease patients and number of coronary arteries involved were not different, but the Gensini scores were higher in SCH group(P<0.05). ConclusionsSubclinical hypothyroidism might affect severity of coronary artery stenosis.
hypotyroidism;subclinical;coronary artery disease
阿力木江·阿不来提,博士,副主任医师。
1.830099乌鲁木齐,武警新疆总队医院心内科;2.844000乌鲁木齐,武警新疆总队第五支队卫生队
R540.4