The mechanism of electro-acupuncture at Shu and Mu acupoints of lung and large intestine meridians for relieving acute gastrointestinal injury in rats with acute pancreatitis
2016-09-14ZhenYanLiuJunWuSiChengLiHangSuLingYuanHuiGuoMeiHuaWanWenFuTang
Zhen-Yan Liu , Jun Wu, Si-Cheng Li, Hang Su , Ling Yuan , Hui Guo Mei-Hua Wan Wen-Fu Tang*
1 Pancreatic Diseases Research Group, Department of Integrative Medicine, West China Hospital, Sichuan University, Chengdu, 610041, PR China; 2 School of Acupuncture and Moxibustion, Chengdu University of Traditional Chinese Medicine, Chengdu, 610075, PR China; 3 Rehabilitation Department, Hubei provincial Hospital of integrated Chinese and Western Medicine, Wuhan, 430015, PR China.
Introduction
Acute pancreatitis (AP) is a common acute abdomen,and severe acute pancreatitis (SAP) is dangerous with complications which causing high fatality rate. So,early diagnosis and treatment are very important for prognosis [1-2]. In terms of integrated Chinese and Western medicines, modified DaChengqi Decoction(DCQD) is a common treatment for AP and it can obviously decrease the incidence of complications and fatality rate [3].
Acupuncture is an important part of Traditional Chinese Medicine which now is used to treat AP.Miraculous Pivot recorded that exterior-interior relationship between the lung and the large intestine and the large intestine is removing waste. The lung and the large intestine influence with each other in physiology and pathology. Nanjing said that Mu acupoints of five organs belongs to yin and Shu acupoints belongs to yang. Yin disease flows in yang and yang disease flows in yin. The combination of Back Shu acupoints and Front-Mu acupoints is an effective treatment in clinical practices.
This study aims to study the mechanism of gastrointestinal injury of AP rats treated by electro-acupuncture at Shu and Mu acupoints of lung and large intestine meridians based on the theory of‘exterior-interior relationship between the lung and the large intestine’.
Materials and Methods
Animals and division
The 40 male SD rats at the age of 1 month were purchased in the laboratory animal center of Sichuan University(No. 0003974).The weight of rats remained in 280±10g. After all rats were fed adaptively for 1 week, the 40 male rats were randomly divided into 5 groups: group A (Intragastric infusion with DCQD,n=8), group B [electro-acupuncture at Back Shu acupoints of lung and large intestine meridians (BL13,BL25), and DCQD, n=8], group C[electro-acupuncture at Front Mu acupoints of lung and large intestine meridians (LU1,ST25),and DCQD,n=8], group D [electro-acupuncture at Front Mu acupoints and Back Shu acupoints of lung and large intestine meridians (BL13, BL25, LU1, ST25), and DCQD, n=8], and group E (the rat model of AP, n=8).
The main reagent and instruments
Sodium taurocholate (America Sigma Company),Chloralic hydras (Chengdu kelon Chemical Reagent Factory), Methylthioninium Chloride Injection(JiShuan Pharmaceutical Company Limited),Microinfusion pump WZS-50F6 (ZheJiang University Medical Instrument co. Ltd), Magnetic stirrer (C-MAG MS 7, Germany IKA Company), SDZ-type II electro-acupuncture apparatus (Shanghai Huayi Medical Instrument Factory), Potter-Elvehjem Tissue Grinders (T10 basic ULTRA-TURRAX, Germany IKA company), Refrigerated centrifuge (Bekman,America Coulter Company), Analytical balance (BSA-224S-CW,Germany Sartorius Company), TNF-α, IL-4, DAO,CCK and VIP test paper (Rat cytokine/chemokine magnetic bead panel kit 96-well plate assay, America Millipore Company), Testing platform (Luminex 200,USA), Conventional surgical instruments, Rats fixator, etc.
AP Model Establishment
The rat model of AP was established by retrograde infusion of 3% sodium taurocholate into biliary pancreatic duct. The rats were forbidden to eat food 12h before operation, but they could drink. Under 10%chloral hydrateanesthesia, 3% sodium taurocholate was injected into biliary pancreatic duct (the mount:1ml/Kg. BW, rate:0.1ml/min) to establish the rat model of AP. It was not limited to drink water but no food was offered after operation [4].
The successful criteria of model establishing: taking pathological slices of pancreatic tissue after killing rats with hematein eosin for pathological examination.
Acupoint location and electro-acupuncture method
Acupoint location on rats was based on Experimental Acupuncture [5] and the Development of the Rat acupoint Ma [6]. Lung Shu (BL13): 5mm Lateral to the lower border of the spinous process of the third thoracic vertebra. Large Intestine Shu (BL25): 5mm lateral to the lower border of the spinous process of the fourth thoracic vertebra. Zhong Fu (LU1): in the depression below the clavicle, under the acromioscapula, on the lateral side of the first intercostal’s space. Tian Shu (ST25): 5mm lateral to the navel.
Electro-acupuncture methods: 2h after operation, the bilateral acupoints were needled at the depth of 5mm with 0.5 inches needle in group B,C,D, and then the needles were connected to the electric acupuncture apparatus after arrival of qi. Rats in group B,C,D were stimulated in the first gear and the stimulation strength was proper when the muscles were trembling (GroupB:bilateral BL13 and BL25 for 40min; Group C: bilateral LU1and ST25 for 40min; Group D: bilateral BL13 and BL25 for 20min, and bilateral LU1and ST25 for 20min). Group A, E were given 40 minutes fixation.The same procedures were repeated three times in 24h.
Preparation of DCQD
The Chinese medicine granular decoction pieces of DCQD is composed of Dahuang (Rhizoma Rhei)12g,Houpo (Cortex Magnoliae Officinalis) 24g, Zhishi(Fructus Aurantii Immaturus) 12g and Mangxiao(Natrii Sulphas) 9g according to Formulation [7]written by ZhongJia Deng, which purchased from Chengdu Green Herbal Pharmaceutical Co. Ltd(Chengdu, China). These components were mixed with sterile distilled water at the concentration of 1g/L. The dosage of DCQD was 10g/kg. BW for every rat. All other groups were offered DQCD 24h after model establishing except group E.
Specimen collection and processing
All rats were killed 12h after medication and their heart blood, pancreatic tissue and large intestine tissue were collected for the measurement of TNF-α, IL-4,DAO, CCK, VIP and pathological examination.
Observation indexes
TNF-α, IL-4, DAO, CCK and VIP in serum, pancreas and intestine were assessed by ELISA and the pathological scores of pancreas and intestine were evaluated according to the pathological criteria from Schmidt [8].
Statistical analysis
Statistical analysis was carried out by SPSS 13.0. All data were expressed as the mean±standard errors(M±SD). One-way analysis of variance (ANOVA) and least signification difference (LSD) were used for statistical analysis among five groups. The level of statistical significance was set at P<0.05.
Results
Compared with group A, TNF-α in group D was significantly lower and IL-4 in group B, C were much higher. The results were shown as table1.
CCK in group B,C,D were higher than in group A while that in group D was obvious (P<0.05). VIP in group B,D were higher than in group A but that in group C was lower and VIP in group D was significantly higher than in group C (P<0.05). DAO in group B,C,D were all higher than in group A while that in group B,D were obviously higher (P<0.05). The results were seen as table 2.
Pathological scores of pancreas and large intestine in group A-D were significantly lower than in group E(P<0.05). The results were seen as table 3.
Table 1 Comparison of TNF-α、IL-4 among groups in serum (pg/m L,

Table 1 Comparison of TNF-α、IL-4 among groups in serum (pg/m L,
*Compared with group A, P<0.05; #Compared with group C, P<0.05.
Group TNF-α A IL-4 631.40±81.74 B 343.01±75.67 571.28±82.09 C 406.51±26.80*485.72±108.20*D 419.35±56.68*641.17±72.86#381.55±63.92
Table 2 Comparison of CCK 、VIP、DAO among groups in serum(pg/m L,
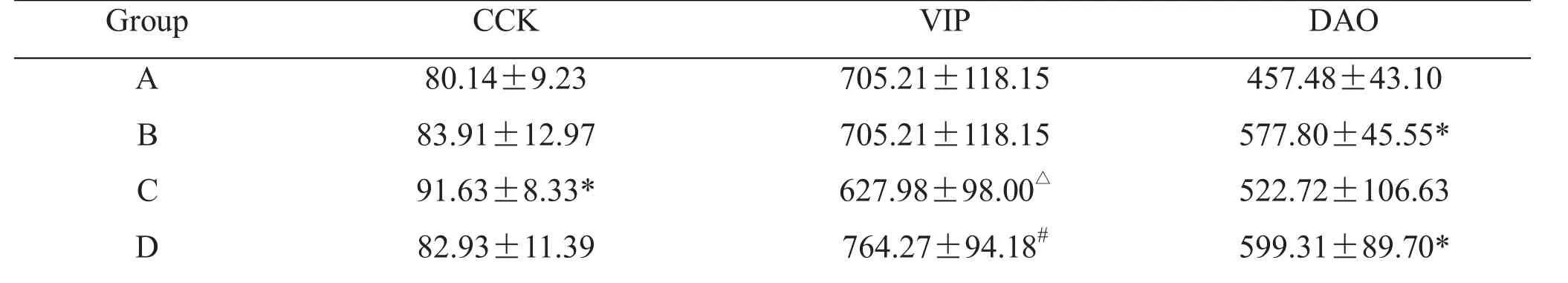
Table 2 Comparison of CCK 、VIP、DAO among groups in serum(pg/m L,
*Compared with group A, P<0.05; △Compared with group B, P<0.05; #Compared with group C, P<0.05.
Group CCK A 80.14±9.23 B 83.91±12.97 C 91.63±8.33*D 82.93±11.39 VIP DAO 705.21±118.15457.48±43.10 705.21±118.15577.80±45.55*627.98±98.00△522.72±106.63 764.27±94.18#599.31±89.70*
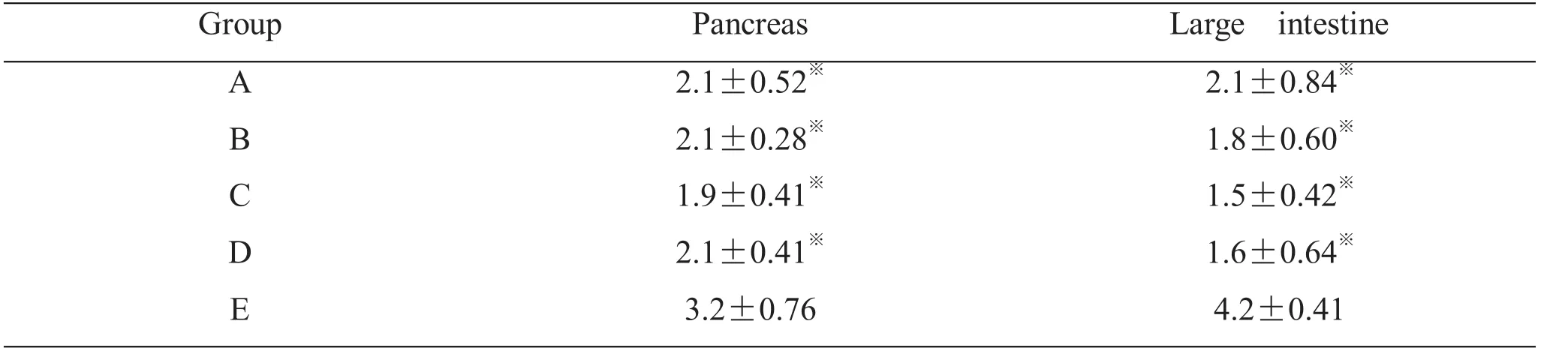
Table 3 Comparison of pancreas and intestine pathological score among groups
Discussions
In recent years, treatingpancreatitis with integrated Chinese and Western medicines has been a hot point of research [9]. Orally taken, external application and enema taking herbs for qi regulation and purgation can ameliorate the gastrointestinal disorders and accelerate the inflammation absorption in AP, which are recommended by The Chinese Medical Guidelines of Acute Pancreatitis in 2014 [10]. Modified DCQD is often accepted to treat AP for relieving disease in clinical practices. SAP is commonly complicated with gastrointestinal disorders which give us challenges for treatment. Composed of Dahuang (Rhizoma Rhei),Houpo (Cortex Magnoliae Officinalis), Zhishi (Fructus Aurantii Immaturus) and Mangxiao (Natrii Sulphas),DCQD traced back to Treaties on Febrile Diseases written by Ji Zhang. It has the function of regulating qi,purging, resolving amass and renewing in TCM and it can ameliorate gastrointestinal ischemia and inhibit bacteria translocation. Moreover, it can reduce the absorption of endotoxin and regulate immune in western medicine [11].
Miraculous Pivot recorded that the lung meridian starts from the middle Jiao downwards to connect with the large intestine. There is an exterior-interior relation between the lung and large intestine for they are yin and yang, zang and fu, exterior and interior respectively, so they have interaction effect on the physiology and pathology. It is effective to combine Backshu acupoints and front mu acupoint to treat the diseases related to corresponding zang and fu in clinical [12].
Therefore, we took DCQD as basic treatment to ameliorate AP and studied the mechanism of electro-acupuncture at back shu and front mu belonging to the lung and large intestine based on the theory of ‘exterior-interior relationship between the lung and the large intestine’ to increase the gastrointestinal motility under the condition.
And in this study, we found that compared with group A, group B had decreased TNF-α (P<0.05). As a pro-inflammatory factor, TNF-α had positive correlation with severity of SAP and decreased TNF-α could help the disease [13]. Group B,C had higher level of IL-4 (P<0.05) which meant electro-acupuncture at LU1 and ST25 could promote pro-inflammatory factor IL-4. Group C not only reduced the level of TNF-α, but also raised the level of IL-4. It has bidirectional effect in balancing inflammation factors to relieve local and whole body inflammation and to help the gastrointestinal injury.
Recent studies [14-17] show that CCK, VIP and DAO play an important role in gastrointestinal motility.As brain-gut peptides, CCK causes the gallbladder contraction and promotes pancreatic enzyme secretion[18]. DAO comes from upper intestinal mucosal villi and placenta villi, which is a kind of highly active diamine oxidase. Intestinal tissue trapped in ischemia,hypoxia or nutritional disorders can lead to intestinal mucosa DAO activity decline, which in turn causes the decrease of the serum DAO activity [17]. So the activity of serum DAO can manifest injury and repair condition of intestinal tract without wound. VIP is a neuropeptides which has function as neurotransmitter and neuromodulator. It can help to reduce pro-inflammatory cytokines and promote level of anti-inflammatory cytokines to relieve damage and keep normal function of intestinal tract [19].
Our study indicates AP treated by electro-acupuncture and DCQD has high level CCK and DAO comparing with treating by DCQD alone. It can improve the gastrointestinal disorders by promoting the pancreas secretion of digestive enzymes and gallbladder excretion of bile. Group C had the highest CCK (P<0.05) and group B,D had better DAO level (P<0.05). Comparing with group A, B, D had higher level of VIP, but group C had lower level of VIP.Group D had better VIP level than in group C (P<0.05).We have known that electro-acupuncture at BL13 and BL25 could efficiently promote VIP which could reduce inflammation and help intestinal tract disorder.
The pathological score results of pancreas and intestine told us that group A-D relieved pathological injury (P<0.05), and the combination of electro-acupuncture and DCQD had a trifle better score than DCQD alone.
Conclusion
It is effective to relieve disease for AP rats by electro-acupuncture at shu and mu acupoints of lung and large intestine meridians (BL13, BL25, LU1, ST25)based on the theory of exterior-interior relationship between the lung and the large intestine, which has relationship with the rebalance between inflammatory and anti-inflammatory cytokines, and higher level of DAO, VIP, CCK, and promoting gallbladder contraction, and promoting pancreatic enzyme secretion, and improving ischemia, hypoxia or nutritional disorders, etc.
Acknowledgment
This study was supported by the National Natural Science Foundation of China (grant numbers 81374042 and 81573857).
Conflict of Interests
The authors declare that there is no conflict of interests regarding the publication of this paper.
1. Li BL. CT Feature and Severity Analysis of Acute Pancreatitis. Mod Dr of Chin 2009, 47(28): 93-94.
2. Ji YL, Sun BC, Kang JL. Surgical Treatment Experience of Severe Pancreatitis. J Regional Anat Operative Surg 2009, 18(1): 34.
3. Xia Q, Huang ZW, Jiang JM et al.Yi-Huo-Qing-Xia method as the main therapy in integrated traditional Chinese and western medicine on severe acute pancreatitis: a report of 1161 cases. Chin J Integr Tradit West Med Intensive Crit Care 2006, 13(3): 131-134.
4. Chen ZF, Chen QL. SAP Rats Model Making Method Improvement. J Xinjiang Med Univ 2008,31(4): 461-463.
5. Yu SG, Guo Y. Experimental acupuncture.Shanghai: Shanghai science and Technology Press 2009: 150-152.
6. Hua XB. The Development of the Rat acupoint Map. Exp Anim Anim Exp 1991, 2 (1): 1-5.
7. Deng ZJ, Li J, Lian JW, et al. Formulation.Shanghai: Shanghai science and Technology Press,2008: 60-61.
8. Schmidt J, Rattner DW, Lewandrowski K, et al. A better model of acute pancreatitis for evaluating therapy. Ann Surg 1992, 215(1): 44-56.
9. General operation Branch of China Society of Integrated Traditional Chinese and Western Medicine. Diagnosis and Treatment of SAP with Integrated Traditional Chinese and Western Medicine (draft). Chin J Surg Integr 2007, 13(3):232-237.
10. Pancreatic operation Group of Chinese Medical Association. Guide for diagnosis and treatment of AP. Chin J Pract Surg 2015, 53(1): 50-53.
11. Cui KL, Cao SH, Wang JD. Clinical Research of DCQD treating MODS. Chin J TCM West Med Crit Care 2003, 10(1): 12-15.
12. Jin YP. Acupuncture and moxibustion academic essence and analysis of NanJing. Chin Acupunct Moxibustion 2006, 26(2): 151-153.
13. Gulcubuk A, Altunatmaz K, Sonmez K et al.Effects of curcuniinon tumournecrosis factor-aplha and interleukin-6 in the late phase of experinenta 1 acute pancreatitis. J Vet Med A 2006, 53(1): 49-54.
14. Xu M, Wang XP, Yuan YZ et al. Gastrointestinal dynamic changes and mechanism of AP. Chin J Emerg Med 2002, 11(5): 327-330.
15. Cote F, Pare P, Friede J. Physiological effect of cholecystokinin on gastric emptying of liquid in functional dyspepsia. Am J Gastroenterol 1995,90(11): 2006-9.
16. Perdikis G, Wilson P, Hinder RA et al.Gastroesophageal reflux disease is associated with enteric hormone abnormalities. Am J Surg 1994,167(1): 186-192.
17. Wu CT, Li ZL. The Function of Diamine Oxidase in intestinal injury with AP, World Chin J Dig 1999, 7(1): 64-65.
18. Liu JZ, Li NL. The Mechanism and Application of cholecystokinine. Sci Technol Inform 2009, 25(1):83.
19. Zhang YC, Yang LP, Tang DH. VIP intestinal protect mechanism in endotoxin shock rats. Chin J Pediatr 2006, 44(5): 369-373.
杂志排行
Traditional Medicine Research的其它文章
- Intestinal obstruction after radical surgery of cervical cancer in a patient with situs inversus
- The regulation of method of tonifying Qi and activating blood circulation in the related gene expressions after spinal cord injury
- Epigenetic regulations of hematopoietic stem cells ageing and the regulation of traditional Chinese medicine
- Revaluation of Xihuang Pill on tumor treatment: from ancient literatures to modern studies
- Two Proved Recipes for Hemostasis
- Tradition and Modern: Public Debate between Traditional Medicine Researcher and Philosopher