Revaluation of Xihuang Pill on tumor treatment: from ancient literatures to modern studies
2016-09-14XueYangXiongZhiWu
Xue Yang, Xiong-Zhi Wu*
1 Huan-Hu-Xi Road, He-Xi District, Tianjin Medical University Cancer Institute and Hospital, National Clinical Research Center for Cancer, Key Laboratory of Cancer Prevention and Therapy, Tianjin, China.
Introduction
Xihuang Pill (XHP), also called Xihuang Wan or Xihuang Capsule, is a complementary and alternative medicine used for tumor treatment in traditional Chinese medicine (TCM) since the 18th c entury. XHP was originally developed by Wang Weide and was recorded in the Wai Ke Quan Sheng Ji, which was written according to the combination of 40 years clinical experience and ancestral secret recipe, during the Qing dynasty. XHP consists of Calculus Bovis,Moschus, Olibanum and Myrrha, serving to disintegrate scleroma, detoxify toxic heat, and promote blood circulation. It is recorded that XHP was used to treat breast cancer, heng, scrofula, phlegm node, deep multiple abscess, pulmonary abscess, and small intestinal abscess (Chinese, supplement 1) in Wai Ke Quan Sheng Ji [1].
Nowadays, XHP is approved by China food and drug administration to treat various tumors alone or in combination with chemotherapy and/or radiotherapy.XHP was recorded to have effects on treating lymphomas, breast cancer, liver cancer, intestinal cancer, and brain tumor [2].
Here, we aimed to put forward a new method to revaluating XHP on its application on tumor therapy from ancient literatures to modern studies and from pharmacy to medicine. In this review, we firstly introduced the application of XHP on tumor therapy from ancient literatures. Then, the antitumor studies of XHP in both clinical and basic aspects were summarized and we also discussed the antitumor material basis and mechanisms of Calculus Bovis,Moschus, Olibanum and Myrrha. In addition, with the development of time, the dosage form of XHP, source and dose of herbs and processing methods of Olibanum and Myrrha have been changed and we also evaluated the advantage and disadvantage of these changes of XHP.
Ancient literature
XHP is an old prescription from Wai Ke Quan Sheng Ji in 1740. Since then, XHP was used by many physicians in ancient China to treat various diseases,especially breast cancer and carbuncle. The clinical efficacy of XHP is significant according to recordation in ancient literatures. XHP combined with cooked rhubarb and realgar was recorded to treat acute mastitis and scrofula in Wai Ke Chuan Xin Ji written by Ma Peizhi (Chinese, Supplement 2) [3]. XHP was mainly recorded to treat breast cancer in old literatures. Xu Ming Yi Lei An recorded one medical notes, in which XHP and Wu Tong Wan (Radix Aucklandiae, Herba Ephedrae, Myrrha, Olibanum, Faeces Togopteri) were taken in the morning and evening alternately to treat breast cancer (Chinese, Supplement 3) [4]. In addition,XHP was recorded to combine with Yanghe decoction(Radix Rehmanniae Preparata, Cortex Cinnamomi,Herba Ephedrae, Colla Corni Cervi, Semen Sinapis Albae, charcoal of ginger, Radix Glycyrrhizae) to treat early breast cancer in Yan Fang Xin Bian (Chinese,Supplement 4) [5]. In Wai Ke Zheng Zhi Quan Shu,XHP combined with Shiquan Dabu decoction was used to treat advanced breast cancer (Chinese, Supplement 5)[6]. Moreover, XHP also can be used to relieve cancer pain in Chong Lou Yu Yao (Chinese, Supplement 6)[7].

Table 1 The action mechanisms of XHP on tumor
Modern research
Basic study
XHP, a classical anti-cancer prescription of traditional Chinese medicine, plays a vital role in treating various malignant tumors (Table 1). Modern pharmacological study confirmed that XHP behaves as a metastasis cell line LoVo cells by regulating ZEB1-SCRIB Loop resulting in inhibition of epithelial-mesenchymal matrix damage [8]. Another study indicated that XHP suppressor by means of preventing angiogenesis and suppressed the ability of proliferation, invasion and migration of highly metastatic human colorectal cancer transition (EMT) [9]. Chen et al. reported that XHP could inhibit zebrafish angiogenesis [10]. The extract of artificial musk and myrrh had no effect on zebrafish angiogenesis, while frankincense and artificial Bovis Calculus could inhibit angiogenesis. These results indicated that frankincense and Bovis Calculus were the main herbs in the XH to play anti-tumor angiogenesis role [11]. XHP inhibited L7212 leukemic cells proliferation in vivo, and arrest cells in S stage.Moreover, XHP could relieve the infiltration of leukemic cells in the liver and spleen of L7212 mice and obviously prolong the survival time of the mice[12].
XHP has been shown to affect breast neoplasms.XHP significantly inhibited Walker256 tumor cells growth in vivo, and XH high dose group showed significantly up-regulated IL-2, IFN-gamma, B7-1 level, and increase CD3+CD4+ T cells in peripheral blood, which indicated that the anti-tumor effect of XHP maybe attribute to its immune clearance function[13]. In addition, XHP can affect breast cells viability and cause apoptosis. XHP had growth-inhibitory effects on MCF-7 and MDA-MB231 cells with a half-maximal inhibitory concentration (IC50) of 10.14 mg/mL (MCF-7) and 8.98 mg/mL (MDA-MB231)[14].
Breast hyperplasia, especially of the columnar cells,is the earliest histologically identifiable lesion linked to cancer progression [15]. Aside from the tumor, XH can treat benign lesions such as breast hyperplasia and prevent transformation into malignancies [16].
Calculus bovis
Calculus Bovis, commonly known as Niuhuang in China, is the dried gallstone of Bos taurus domesticus Gmelin and one of the most important and precious traditional Chinese medicines. Calculus bovis has been used in TCM for thousands years to treat high fever,convulsion, inflammation, and tumor [17]. Calculus bovis contains bilirubin, bile acids, amino acids, and other compounds [18]. Bilirubin and bile acids are primary active constituents in Calculus Bovis.
Bile acids
Bile acids, as one of the main active constituents in Calculus bovis, are important indicator for evaluating the quality of Calculus bovis and the substitutes, which have the effects of diminishing inflammation,antianaphylaxis and antidote [19]. Unique biologic activities have been identified for the four different bile acids: cholic acid (CA), deoxycholic acid (DCA),chenodeoxycholic acid (CDCA), and ursodeoxycholic acid (UDCA) (Figure 1). Among four bile acids, DCA is the major active constituent of Calculus bovis. One study suggested that blockade of fMLP receptors may contribute to the anti-inflammatory effects of traditional medicine containing DCA [20].
Different bile acids exhibit distinct biological activities toward tumor cells. CA and UDCA had only minimal cytotoxic effect on ovarian cancer cell lines A2780 and A2780-CP-R (cisplatin-resistant) even at maximum concentrations. In contrast, CDCA and DCA have significant cytotoxic activity in both platinum sensitive and platinum-resistant ovarian cancer cell lines via induction of apoptosis. The mechanism of apoptosis appears to be mediated by alternative kinases distinct from protein kinase C (PKC) [21]. Another study found that incubating cells with CDCA or DCA caused colon cancer cells morphological changes,which were characteristics of apoptosis, whereas incubating cells with UDCA inhibited cell proliferation but did not induce apoptosis. CA had no discernible effect on cells. Notably, the cytotoxicity reported for DCA may be due to its capacity to induce apoptosis via a PKC-dependent signaling pathway [22].

Figure 1 The molecular structure of four different bile acids: cholic acid (CA, A),deoxycholic acid (DCA, B), chenodeoxycholic acid (CDCA, C), and ursodeoxycholic acid(UDCA, D).
Although the ingredients in bile acid exhibit anti-tumor effects, there are studies reporting the opposite directions toward gastrointestinal cancer including colon cancer, esophageal cancer [23-25].More recent reports confirmed that DCA directly stimulates proliferation of human colonic mucosa [26]and human colon cancer cells in culture [27, 28]. It has been reported that exposure to DCA can lead to the induction of a variety of growth regulatory genes including cyclooxygenase-2 [29], as well as stimulate the activity of AP-1 and NF-kB transcription factors[30, 31]. Recent evidence suggests that bile acids promote tumor growth by stimulating several kinase signaling pathways, in part by activating epidermal growth factor receptor (EGFR) signaling pathway [32].The controversial effects of bile acids on gastrointestinal cancer may be related to its concentration. > 100 µmol L–1 DCA induces apoptosis in colon cancer cells, whereas, low-dose DCA stimulates colon cancer cell proliferation by a mechanism that is mediated by PKC [33]. Further studies are needed to clarify the action mechanism of bile acids on gastrointestinal cancer, especially colon cancer.
Taurine
Taurine (Figure 2A), also called 2-aminoethanesulfonate, is ubiquitous and is the most abundant intracellular free amino acids present in mammalian tissues, including those exposed to high concentrations of oxidants, such as heart, retina,skeletal muscle, brain, and leukocytes [34-36]. Taurine has been shown to be tissue-protective in many models of oxidant-induced injury [37]. One study evaluated a possible role of serum taurine level as an early marker for breast cancer patients. The most impressive observation in this work showed significant decreases in serum taurine levels in both breast cancer and high risk groups when compared to normal control group[38]. Taurine was investigated to the enhanced permeability of doxorubicin on the M5076 ovarian sarcoma cells in vitro, which elucidated the novel effect of taurine to increase doxorubicin-induced antitumor activity [39]. In addition, taurine can partly attenuate the harmful actions of bile acids [40].

Figure 2 The molecular structure of taurine (A)and taurolidine (B).
Taurolidine
Taurolidine [bis(1,1-dioxoperhydro-1,2,4-thiadiazinyl-4)-methane (TRD)] (Figure 2B), a derivative of the amino acid taurine, was first described as an anti-bacterial substance [41]. Recently, taurolidine has been shown to possess anti-neoplastic properties in vitro and in vivo against a variety of cancers including colorectal cancer, ovarian cancer, brain tumor and melanoma [42-45]. It has been shown to enhance apoptosis, inhibit angiogenesis, reduce tumor adherence [46]. Previous study reported that TRD selectively inhibited the growth of human ovarian tumor cell lines in vitro through the induction of apoptosis in tumor cells, instead of regulating cell cycle distribution. Furthermore, administration of TRD to nude mice bearing human ovarian tumor xenografts significantly inhibited both tumor formation and growth [43]. Moreover, one study indicated that TRD significantly attenuated murine melanoma tumor growth in vitro and in vivo, which may result from TRD-induced apoptosis by modulation of the Bcl-2 family proteins [45]. Besides, one review reported that TRD additionally inhibited tumor angiogenesis [47].Treatment with TRD inhibited the growth of all ten osteosarcoma cell lines and TRD-induced growth inhibition was found to be associated with a dose dependent increase in the number of apoptotic cells.And apoptosis was shown to be caspase-dependent. In addition to apoptosis induction action, TRD also inhibited adhesion of osteosarcoma cell [48].Subsequent to these experimental observations, TRD has shown encouraging clinical results after intravenous administration in patients with gastrointestinal malignancies and tumors of the central nerve system [47].
Moschus
Moschus, also called Musk, is a rare Chinese medicine,which is dry secretions and origins from mature male moschus deer including Moschus berezovskii Flerov,Moschus sifanicus Przewalski, and Moschus moschiferus Linnaeus [49]. As a highly valued ingredient of Chinese medicinal remedies, musk is used as a detoxification agent and for treating fever,inflammation and swelling, and pain. Mouschus consists of muscone (3-methylcyclopentadecanone-1),androstane alkaloids, androstanoids and cholestanoidsan [50-52]. A small amount of muscopyridine is also found in the secretion from the ventral glands of male musk deer [53].
Recent study indicated that the decoction of Moschus, and Toona sinensis exhibited the strongest anticancer effects, compared to two single decoctions.The combined decoction arrested HeLa cell cycle progression in S-phase and RB pathway is partially responsible for the cell cycle arrest [54].
The antitumor activity was first observed in musks secreted by the mammalian genital gland. These musks consist of low-molecular-weight macrocyclic ketones(MCKs) of low molecular weight (224-250 Da).Carcinostatic activity was detected in diverse natural MCKs by the inhibition of mitochondrial dehydrogenase activity in Ehrlich ascites tumor cells.In addition, MCKs inhibited the invasive action of human fibrosarcoma HT1080 cells even after the short-term exposure of 3 h at 25 µM, without reducing cell viability [55].
Muscone
Muscone (Figure 3A) is believed to be the main active ingredient of Mouschus [53]. Previous study showed that muscone has protective effects on the neural system and cardiac myocytes [56-60]. However, it remains unclear whether muscone is also effective in tumor therapy. Further studies are in urgent need to verify the anti-tumor effects of muscone.

Figure 3 The molecular structure of muscone(A), musk ketone (B), and musk xylene (C).
Synthetic musk
Musk ketone (MK, Figure 3B) and Musk xylene (MX,Figure 3C), two types of synthetic musk, are often used in fragrances and soaps to substitute the natural musk.In China, synthetic musk is not approved in the application of medicine at present. One study explored the effect of MK treatment on breast cancer. MK can significantly inhibit the expression of angiogenic factors, such as VEGF and bFGF in MDA-MB-231 breast tumor tissue, which offers broad prospects for application in inhibition of tumor angiogenesis [61].
Frankincense
Boswellia serrata Roxb. et Colebr. and Boswellia carterii Birdw. (syn. B. sacra) are deciduous trees growing in China, India, the Arab peninsula, and some African countries (Somalia, Ethiopia). The resin gum of these trees is called frankincense or Olibanum and is used not only for religious rituals, but also for medicinal purposes in different civilizations [62].Frankincense is reported to contain 60-85% resins(mixtures of terpenes), 6-30% gums (mixture of polysaccharides) and 5-9% essential oil [63]. It has been used to alleviate pain and inflammation, to invigorate the circulation of blood in China and as an antiarthritic in Ayuredic medicine in India for thousands of years (Boswellic acids: novel, specific,nonredox inhibitors of 5-lipoxygenase [64].
Frankincense essential oil
Frankincense essential oilprepared from hydrodistillation of Boswellia sacra gum resins and is frequently used in aromatherapy practices. According to previous studies, the constituents of frankincense oil vary according to the climate, harvest conditions and geographical sources of the frankincense resin [65].Recent studies indicate that frankincense essential oil has tumor inhibition effects. A review reported that Boswellia essential oil could suppress transformation,proliferation, and metastasis of tumors by regulating cell cycle arrest, apoptosis induction, and various growth signals [66].
Frankincense essential oil elicited selective cancer cell death on human bladder cancer J82 cells via NRF-2-mediated oxidative stress [67]. Microarray and bioinformatics analysis proposed multiple pathways that can be activated by frankincense oil to induce bladder cancer cell death [68]. It also induces human pancreatic cancer cell death in cultures and in a xenograft murine model. The anti-tumor activity of frankincense essential oil on pancreatic cancer cells is mediated through multiple signaling pathways and cell cycle regulators, and is dependent upon caspase pathway mediated apoptosis [69]. In addition,Boswellia sacra essential oil has tumor cell-specific cytotoxicity in multiple breast cancer cell types through suppresses Akt and ERK1/2 activation and G1 phase arrest of cell cycle by suppressing cyclin D1 and cdk4 expression [70].
Boswellic acids
The active compounds of frankincense are the boswellic acids, which are pentacyclic triterpenic acids in Boswellia sacra essential oils. Recent investigations have shown that boswellic acids exert potent anticancer activities through their anti-proliferative and pro-apoptotic effects in multiple human cancer cell lines and in mice [71, 72]. Boswellic acids have anti-proliferation and anti-cancer effects on HepG2 cells. The apoptotic effect is mediated by a pathway dependent on caspase-8 activation [73]. Boswellic acids also induce malignant glioma cells apoptosis at low micromolar concentrations by via a p53-independent pathway [74]. Furthermore, boswellic acids can inhibit glioma growth in vivo and prolong survival time of experimental rats [75].

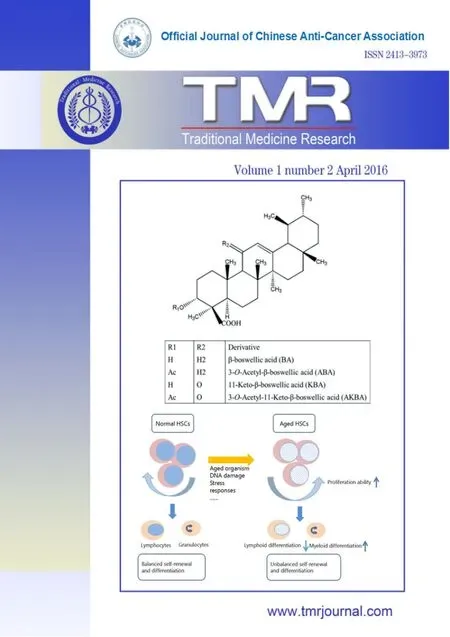
Figure 4 The molecular structure of four major boswellic acids found in frankincense.
There are four major boswellic acids (Figure 4) found in frankincense: β-boswellic acid (BA),acetyl-β-boswellic acid (ABA), 11-keto-β-boswellic(KBA) acid and 3-O-acetyl-11-Ke-to-β boswellic acid

Table 2 The main action mechanism of four boswellic acids on tumor
(AKBA) [76]. Among these boswellic acids, AKBK is the main anti-tumor active constituent (Table 2).Park and coworkers showed that treatment of pancreatic cancer cells and breast cancer MDA-MB-231 cells with AKBA suppressed the CXCL12-induced invasion of these cells and down-regulated CXCR4. It has also been found that the AKBA-mediated down-regulation of CXCR4 occurred at both the mRNA and protein levels [77].However, another study indicated that prostate cancer cells were most sensitive to boswellic acids, while breast cancer and leukemia cell lines were the most resistant [72]. Consistently, ABA and AKBA inhibit proliferation and elicit cell death in chemoresistant androgen-independent PC-3 prostate cancer cells in vitro and in vivo. At the molecular level, these compounds inhibit constitutively activated NF-kappaB signaling by intercepting the IkappaB kinase (IKK)activity promoting apoptosis of PC-3 prostate cancer cells [78]. Another study also showed that AKBA suppressed tumor growth in the human prostate tumor xenograft mice treated daily (10 mg/kg AKBA). The inhibitory effect of AKBA on tumor growth was well correlated with suppression of angiogenesis. The molecular mechanism of angiogenic inhibition of AKBA induced by VEGFR2 signaling pathways [79].Treatment of meningioma cells by AKBA revealed a potent cytotoxic activity by the inhibition of the Erk signal transduction pathway [80]. Boswellic acids,particularly AKBA and KBA have anti-proliferative and apoptotic effects in human HT-29 cells. The apoptotic effect is mediated via a pathway dependent on caspase-8 activation but independent of Fas/FasL interaction [81]. Besides, the anti-cancer effect of AKBA may in part be due to its ability to demethylate and reactivate methylation-silenced tumor suppressor genes of colorectal cancer cells [82].
In addition to solid tumors, boswellic acid also exerts anti-tumor to hematological malignancies. BA,ABA, KBA and AKBA all inhibited the synthesis of DNA, RNA and protein in human leukemia HL-60 cells in a dose dependent manner and AKBA has the most pronounced inhibitory effects. AKBA significantly inhibited the cellular growth of HL-60 cells, but did not affect cell viability [83]. The inhibition of leukemic cells by AKBA may be due to induction of apoptosis by inhibiting topoisomerase I[84].
One compound, containing alpha- and beta-boswellic acid acetate in 1:1, could induce differentiation of B16F10 mouse melanoma cells,blocked the cell population in G1 phase, inhibited migration and topoisomerase II activity. In addition,this compound induced apoptosis of HT-1080 cells and inhibited the secretion of MMPs from HT-1080 cells[64].
Tetracyclic triterpenes
In addition to boswellic acids, tetracyclic triterpenes such as 3-beta-acetoxy-tirucallic acid and 3-beta-acetoxy-tirucallic acid, also isolated from Boswellia species, showed potent anticancer activity against prostate cancer cells [85].
Myrrha
Myrrha, also called myrrh, is an aromatic gum resin,which was the plant stem resinous exudate of different Commiphora species and has been used for centuries to treat various diseases. Myrrha is used in traditional Chinese medicine for the treatment of trauma, arthritis,fractures and diseases caused by blood stagnation.Myrrha has also been used in the Ayurvedic medical system because of its therapeutic effects against inflammatory diseases, coronary artery diseases,gynecological disease, obesity, etc [85-87]. Especially,Myrrha was a common analgesic and has been used to clean wounds and sores for more than 2000 years, until the European discovered the morphine [88]. Previous study also indicated that the crude aqueous extracts of Myrrha exhibit anti-tumor toward various human and murine cell lines including lung cancer, breast cancer,pancreatic cancer [89]. Myrrha has been found to have cytotoxic and antitumor activity equivalent to that of the standard cytotoxic drug cyclophosphamide [90].
Previous investigations have revealed that the chemical substances from Myrrha contained about 3–8% essential oil, 30–60% water-soluble gum and 25–40% alcohol-soluble resins [91]. Phytochemical investigation of this genus has resulted in identification of more than 300 secondary metabolites which include terpenoids, steroids, flavonoids and ligans, etc. [92].
Myrrha Essential oil
Essential oils are secondary metabolite of plants whose constituents are basically a complex mixture of terpenic hydrocarbons and oxygenated derivatives such as aldehydes, ketones, epoxides, alcohols and esters.Monoterpenes, diterpenes, and even sesquiterpenes constitute the composition of many essential oils. High contents of oxygenated sesquiterpenes (36.1%) and aliphatic acids (22.8%) were found in Commiphora parvifolia Engl., in which caryophyllene oxide (14.2%),beta-eudesmol (7.7%), bulnesol (5.7%), T-cadinol(3.7%) and hexadecanoic acid (18.4%) predominated[93]. Sesquiterpenoids are the primary chemical compositions of the Myrrha essential oil [94].
Sesquiterpenoids
Recent studies have shown that sesquiterpenoids,nonsteroidal compounds, found in myrrh possess anti-tumorigenic effects [87, 95]. Two sesquiterpenoids isolated from myrrh, 1(10)E,2R,4R-2-methoxy-8,12-ep-oxygermacra-1(10),7,11-trien-6-one (ST1) and 2-meth-oxy-5-acetoxy-furanogermacr-1(10)-en-6-one (ST2),inhibited the proliferation of prostate cancer LNCaP and PC3 cells through reduction of AR expression,inhibition of AR translocation into the nucleus,reduction of the expression of ARA70 and SRC-1, and interference with the interaction between AR and ARA70 and SRC-1, leading to the inhibition of AR transactivity [96].
β-bisabolene, a sesquiterpene from the essential oil extract of opoponax (Commiphora guidottii), also exhibits cytotoxicity in mouse and human breast cancer cell lines in vivo and in vitro by inducing apoptosis [97].
α-bisabolol is a small, oily sesquiterpene alcohol with some anti-inflammatory and even anti-microbial properties [98]. Previous studies discovered that α-bisabolol exerts a selective pro-apoptotic action towards human malignant cells, both nonhematological and leukemic. α-bisabolol selectively induced glioma cells apoptosis through an intrinsic pathway, while, the viability of normal rat glial cells was not affected by treatment with alpha-bisabolol at the same concentrations [99]. α-Bisabolol also induces doseand time-dependent apoptosis in HepG2 cells via a Fas- and mitochondrial-related pathway, involves p53 and NFκB [100, 101]. α-bisabolol can suppress the proliferation and survival of pancreatic cancer cells by inhibiting Akt activity and upregulating EGR1 in pancreatic cancer [102]. In an in vitro model of glioblastoma cell lines α-bisabolol induced apoptosis through the mitochondrial pathway, by abolishing the mitochondrial transmembrane potential (DYm) and inducing the release of cytochrome c [99]. In addition,α-bisabolol exerted a pro-apoptotic activity in an ex vivo leukemic model through a similar mechanism[103]. α-bisabolol may induce preferential toxicity against tumor cells because it enters the cells through lipid rafts [104], that are more represented in tumor cells than their normal counterparts [105]. Another study indicated that α-bisabolol may act as a candidate for treatment of BCR-ABL+ leukemias to overcome resistance to TKI alone and to target leukemic cells through BCR-ABL independent pathways [106].
Cycloartane triterpenoids
Cycloartan-24-ene-1α,2α,3β-triol (MY-1), isolated from Commiphora myrrha, has cytotoxic and apoptotic effects of MY-1 on human prostatic cancer PC-3 cells by regulating the expression levels of Bcl-2, Bax, p53 and caspase-3 [107].
Myrrh and frankincense are often used for their combination on clinic in order to obtain a synergistic effect with relieving pain and activating blood circulation, and especially to treat blood stasis syndrome of gynecology diseases, for example dysmenorrhea. According to the traditional Chinese medicinal theory, myrrh and frankincense were commonly used with combination and it was considered that the combination with enhanced effects on clinic [108, 109]. The combination of frankincense and myrrh oils exhibited synergistic effects on Cryptococcus neoformans and Pseudomonas aeruginosa [108]. One study indicated that the MCF-7 and HS-1 cell lines showed increased sensitivity to the myrrh and frankincense essential oils compared with the remaining cell lines. In addition, the anticancer effects of myrrh were markedly increased compared with those of frankincense, however, no significant synergistic effects were identified. The flow cytometry results indicated that apoptosis may be a major contributor to the biological efficacy of MCF-7 cells[110].
Clinical observation research
Previous clinical observation studies reported that XHP have clinical efficacy either in its anti-cancer effects or in adjuvant therapeutic effects. Hong et al. explored the possibility of XHP application in assistant therapy in patients with breast cancer, short- and long-term clinical efficacy were assessed in this study [111]. This study investigated the application of XHP with TEC(taxotere, epirubicin, and cyclophosphamide) in patients with breast cancer and found that XHP could significantly enhance the two-year survival rate and overall response rate in the treatment group. However,XHP did not alter the side effects of TEC. Furthermore,XHP regulated T-lymphocyte subsets and improved the immunity of breast cancer patients taking CEF(cyclophosphamide, epirubicin, and fluorouracil) [112].In addition, XHP has selective effect on estrogen-dependent breast cancer. XHP had synergistic effect on symptoms improvement and quality of life in estrogen-dependent breast cancer patients combined with Letrozole. And the curative effect of XHP group was also better than that of non-estrogen-dependent breast cancer [113]. In addition to breast cancer, XHP can also improve the quality of life (QOL) in patients with advanced primary hepatic cancer, advanced esophageal cancer, and advanced pancreatic cancer[114-116].
Dosage form improvement
With the development of time, some changes of XHP have happened, such as the dosage form of XHP,source and dose of herbs and processing methods of frankincense and myrrh. Here, we aim to describe the reasons of these changes and objectively discuss the influence of these changes on efficacy of XHP.
XHP was recorded to be shaped by yellow rice,which is inconvenient to store. The modern manufacturing method of generating XHP is beta-cyclodextrin inclusion. The period of validity of XHP produced using modern craftsmanship is 48 months.
In addition, as the natural occurrence is very rare,natural Calculus bovis and natural Moschus are difficult to get. Besides, Forest musk deer (Moschus berezovskii), a rare wild medicinal animal, is listed under the category of the state key protected wildlife list of China. Natural Moschus, secreted by the musk glands, is so precious that it is rare in clinical practice and illegally collection of it is criminal behavior in China. Under this circumstance, great attempts have been made to obtain artificial Calculus bovis and artificial Moschus to meet the demand of the medical use.
Substitutes for Calculus Bovis are now available in clinical and medicinal preparations through simply mixing bilirubin, taurine, bile acids and other trace constituents [117]. Two artificial substitutes for Bos Taurus have been introduced in China: artificial Calculus Bovis and in vitro cultured Calculus Bovis.Nowadays, XHP used in clinical practice also take artificial Calculus Bovis or in vitro cultured Calculus Bovis instead of natural Calculus Bovis. By means of comparative pharmacological study, the main pharmacodynamics and toxicity of cultured calculus bovis and natural calculus bovis were compared. The results show that both drugs possess sedative,antispasmodic, antipyretic, anti-inflammatory,cardiotonic and hypotensive effects, the strength of effect and toxicity being similar [118].
Notably, the composition formula of artificial musk remains unknown, because it is national level of confidentiality in China. The artificial Moschus can be used the same as natural Moschus. The use of artificial Calculus bovis and artificial Moschus to replace natural Calculus bovis and natural Moschus is not affect the curative effect of XHP. Besides, the dose of artificial Calculus bovis and artificial Moschus is 3-fold higher in XHP compared to the prescription in Wai Ke Quan Sheng Ji.
Thirdly, processing method of frankincense and myrrh is also different compared to the prescription in Wai Ke Quan Sheng Ji. The essential oil of frankincense and myrrh was removed in Wai Ke Quan Sheng Ji, while, frankincense and myrrh were treated with vinegar and reserved the essential oil. Modern pharmacological research has revealed that essential oils are the primary effective components in xxxxxxxxx frankincense and myrrh oil that exhibit a broad oils are the primary effective components in spectrum of biological activities such as antimicrobial,anti-inflammatory, and antitumor activities [119].Therefore, further studies are needed to clarify these differences.
Grade of references
In the present study, we evaluated the level of references to make our conclusion more objective(Table 3).
Conclusion and perspective
Here, we put forward a new method to revaluate XHP on its application on tumor therapy from ancient literatures to modern studies and from pharmacy to medicine. As a multi-compound medicine, XHP has multiple targets in tumor treatment and it is needed to further study how these compounds work together and whether they have synergistic effects with each other.In addition, the changes in the dosage form of XHP,source and dose of herbs and processing methods of Frankincense and Myrrha also deserve our in-depth study. It is well known that traditional Chinese medicine is based on a set of theories and Zheng(syndrome). Therefore, XHP application may be more effective for certain syndromes according to TCM theory.
Appendix A. Supporting information
Additional supporting information associated with this article can be found in the online version at http://tmrjournal.faisco.cn/nd.jsp?id=41&_np=125_447

Table 3 Hierarchy of evidences
1. Wang HX, Wai Ke Zheng Zhi Quan Sheng Ji.Shanghai: Shanghai Scientific and Technical Publishers, 2009. 王洪绪. 《外科证治全生集》.上海: 上海科学技术出版社, 2009.
2. Guo Q, Lin J, Liu R, et al. Review on the Applications and Molecular Mechanisms of Xihuang Pill in Tumor Treatment. Evid Based Complement Alternat Med 2015, 2015:854307.
3. Ma PZ, Wai Ke Chuan Xin Ji, Xihuang Wan Beijing: People's Medical Publishing House, 1959.马培之.《外科传薪集》. 北京:人民卫生出版社,1959.
4. Wei ZX, Xu Ming Yi Lei An. Beijing: People's Medical Publishing House, 2000. 魏之琇.《续名医类案》. 北京:人民卫生出版社,2000.
5. Bao XG, Yan Fang Xin Bian. Beijing: People's Medical Publishing House, 2007. 鲍相璈.《验方新编》. 北京:人民卫生出版社,2007.
6. Xu KC, Wai Ke Zheng Zhi Quan Shu. Beijing:People's Medical Publishing House, 1961. 许克昌.《外科证治全书》. 北京:人民卫生出版社,1961.
7. Zheng MJ, Chong Lou Yu Yao. Beijing: China Medical Science Press, 2011. 郑梅涧.《重楼玉钥》.中国医药科技出版社,2011.
8. Chen XY, Wang J, Zhang YY, et al. Analysis of anti-tumor effects of Xihuang Pill based on pharmacodynamic studies review. Chin J Tradit Chin Med Pharm 2010, 25(3): 409-412.
9. Wang M, Meng JY, He SF. Xihuang Pill induces mesenchymal-epithelial transition and inhibits loss of apical-basal polarity in colorectal cancer cell through regulating ZEB1-SCRIB loop. Chin J Integr Med 2014, 20(10): 751-757.
10. Wang SF, Liu KC, Wang XM, et al. Effect of Xihuang pill on angiogenesis in zebrafish embryo.Chin J Hosp Pharm 2010, 30 (10): 821-823.
11. Chen XQ, Hou HR, Liu KC, et al. Effect of Xihuang Pills and its decomposed formula on zebrafish embryonic angiogenesis. Drugs Clinic 2011, 26(1): 50-53.
12. Tang YJ, Chen G. Experimental study on anti-acute leukemia with Chinese traditional drugs.Chin J Integr Med 1990,10(12): 734-736.
13. Ma J, Wang YY, Yang W, et al. Experimental study on anti-tumor effect of xihuang pill and its immune clearance function. Chin J Chin Mat Med 2014, 39(8): 1499-1501.
14. Pan G, Wang W, Wang L, et al. Anti-breast cancer effects and mechanisms of Xihuang pill on human breast cancer cell lines. J Tradit Chin Med 2013,33(6): 770-778.
15. Bjorner S, Fitzpatrick PA, Li Y, et al. Epithelial and stromal microRNA signatures of columnar cell hyperplasia linking Let-7c to precancerous and cancerous breast cancer cell proliferation. PLoS One 2014, 9(8): e105099.
16. Sui YB. Clinical study of Xihuang Pills in treating cyclomastopathy. Chin J Tradit Chin Med Pharm 2010, 25(4): 618-619.
17. Zhao YH, Xiu RJ. Pharmacology and clinical application of calculus bovis and its substitute.Bull Acad Mil Med Sci 2007, 31(2): 175-178.
18. Wan TC, Cheng FY, Liu YT, et al. Study on bioactive compounds of in vitro cultured Calculus Suis and natural Calculus Bovis. Anim Sci J 2009,80(6): 697-704.
19. Liu Y, Tan P, Liu S, et al. A new method for identification of natural, artificial and in vitro cultured Calculus bovis using high-performance liquid chromatography-mass spectrometry.Pharmacogn Mag 2015,11(42): 304-310.
20. Chen X, Mellon RD, Yang L, et al. Regulatory effects of deoxycholic acid, a component of the anti-inflammatory traditional Chinese medicine Niuhuang, on human leukocyte response to chemoattractants. Biochem Pharmacol 2002, 63(3):533-541.
21. Horowitz NS, Hua J, Powell MA, et al. Novel cytotoxic agents from an unexpected source: bile acids and ovarian tumor apoptosis. Gynecol Oncol 2007, 107(2): 344-349.
22. Martinez JD, Stratagoules ED, LaRue JM, et al.Different bile acids exhibit distinct biological effects: the tumor promoter deoxycholic acid induces apoptosis and the chemopreventive agent ursodeoxycholic acid inhibits cell proliferation.Nutr Cancer 1998, 31(2): 111-118.
23. Weisburger JH, Reddy BS, Barnes WS, et al. Bile acids, but not neutral sterols, are tumor promoters in the colon in man and in rodents. Environ Health Perspect 1983, 50(4): 101-107.
24. Reddy BS, Wynder EL. Large-bowel carcinogenesis: fecal constituents of populations with diverse incidence rates of colon cancer. J Natl Cancer Inst 1973, 50(6): 1437-1442.
25. Narisawa T, Magadia NE, Weisburger JH, et al.Promoting effect of bile acids on colon carcinogenesis after intrarectal instillation of N-methyl-N'-nitro-N-nitrosoguanidine in rats. J Natl Cancer Inst 1974, 53(4): 1093-1097.
26. Bartram HP, Scheppach W, Schmid H, et al.Proliferation of human colonic mucosa as an intermediate biomarker of carcinogenesis: effects of butyrate, deoxycholate, calcium, ammonia, and pH. Cancer Res 1993, 53(14): 3283-3288.
27. Peiffer LP, Peters DJ, McGarrity TJ. Differential effects of deoxycholic acid on proliferation of neoplastic and differentiated colonocytes in vitro.Dig Dis Sci 1997, 42(11): 2234-2240.
28. Milovic V, Stein J, Odera G, et al. Low-dose deoxycholic acid stimulates putrescine uptake in colon cancer cells (Caco-2). Cancer Lett 2000,154(2): 195-200.
29. Zhang F, Subbaramaiah K, Altorki N, et al.Dihydroxy bile acids activate the transcription of cyclooxygenase-2. J Biol Chem 1998, 273(4):2424-2428.
30. Qiao D, Chen W, Stratagoules ED, et al. Bile acid-induced activation of activator protein-1 requires both extracellular signal-regulated kinase and protein kinase C signaling. J Biol Chem 2000,275(20): 15090-15098.
31. Payne CM, Crowley C, Washo-Stultz D, et al. The stress-response proteins poly (ADP-ribose)polymerase and NF-kappaB protect against bile salt-induced apoptosis. Cell Death Differ 1998,5(7): 623-636.
32. Qiao L, Studer E, Leach K, et al. Deoxycholic acid(DCA) causes ligand-independent activation of epidermal growth factor receptor (EGFR) and FAS receptor in primary hepatocytes: inhibition of EGFR/mitogen-activated protein kinase-signaling module enhances DCA-induced apoptosis. Mol Biol Cell 2001, 12(9): 2629-2645.
33. Milovic V, Teller IC, Faust D, et al. Effects of deoxycholate on human colon cancer cells:apoptosis or proliferation. Eur J Clin Invest 2002,32(1): 29-34.
34. Wright CE, Lin TT, Lin YY, et al. Taurine scavenges oxidized chlorine in biological systems.Prog Clin Biol Res 1985, 179: 137-147.
35. Fukuda K, Hirai Y, Yoshida H, et al. Free amino acid content of lymphocytes nd granulocytes compared. Clin Chem 1982, 28(8): 1758-1761.
36. Green TR, Fellman JH, Eicher AL, et al.Antioxidant role and subcellular location of hypotaurine and taurine in human neutrophils.Biochim Biophys Acta 1991, 1073(1): 91-97.
37. Schuller-Levis GB, Park E. Taurine: new implications for an old amino acid. Fems Microbiol Lett 2003, 226(2): 195-202.
38. El Agouza IM, Eissa SS, El Houseini MM, et al.Taurine: a novel tumor marker for enhanced detection of breast cancer among female patients.Angiogenesis 2011, 14(3): 321-330.
39. Sadzuka Y, Matsuura M, Sonobe T. The effect of taurine, a novel biochemical modulator, on the antitumor activity of doxorubicin. Biol Pharm Bull 2009, 32(9): 1584-1587.
40. Takahashi K, Azuma Y, Shimada K, et al. Quality and safety issues related to traditional animal medicine: role of taurine. J Biomed Sci 2010,17(24) Suppl 1: S44.
41. Traub WH, Leonhard B, Bauer D. Taurolidine: in vitro activity against multiple-antibiotic-resistant,nosocomially significant clinical isolates of Staphylococcus aureus, Enterococcus faecium, and diverse Enterobacteriaceae. Chemotherapy 1993,39(5): 322-330.
42. McCourt M, Wang JH, Sookhai S, et al.Taurolidine inhibits tumor cell growth in vitro and in vivo. Ann Surg Oncol 2000, 7(9): 685-691.
43. Calabresi P, Goulette FA, Darnowski JW.Taurolidine: cytotoxic and mechanistic evaluation of a novel antineoplastic agent. Cancer Res 2001,61(18): 6816-6821.
44. Stendel R, Stoltenburg-Didinger G, Al Keikh CL,et al. The effect of taurolidine on brain tumor cells.Anticancer Res 2002, 22(2A): 809-814.
45. Sun BS, Wang JH, Liu LL, et al. Taurolidine induces apoptosis of murine melanoma cells in vitro and in vivo by modulation of the Bcl-2 family proteins. J Surg Oncol 2007, 96(3):241-248.
46. Neary PM, Hallihan P, Wang JH, et al. The evolving role of taurolidine in cancer therapy. Ann Surg Oncol 2010, 17(4): 1135-1143.
47. Jacobi CA, Menenakos C, Braumann C.Taurolidine--a new drug with anti-tumor and anti-angiogenic effects. Anticancer Drugs 2005,16(9): 917-921.
48. Walters DK, Muff R, Langsam B, et al.Taurolidine: a novel anti-neoplastic agent induces apoptosis of osteosarcoma cell lines. Invest New Drugs 2007, 25(4): 305-312.
49. Xia XH, Li Q, Liu M. Neuroprotective effect of a formula, moschus combined with borneolum synthcticum, from traditional chinese medicine on ischemia stroke in rats. Evid Based Complement Alternat Med 2014, 2014:157938.
50. Fujimoto S, Yoshikawa K, Itoh M, et al. Synthesis of (R)- and (S)- muscone. Biosci Biotechnol Biochem 2002, 66(6): 1389-1392.
51. Oh SR, Lee JP, Chang SY, et al. Androstane alkaloids from musk of Moschus moschiferus.Chem Pharm Bull 2002, 50(5): 663-664.
52. Sokolov VE, Kagan MZ, Vasilieva VS, et al. Musk deer (Moschus moschiferus): Reinvestigation of main lipid components from preputial gland secretion. J Chem Ecol 1987, 13(1): 71-83.
53. Lin DL, Chang HC, Huang SH. Characterization of allegedly musk-containing medicinal products in Taiwan. J Forensic Sci 2004, 49(6): 1187-1193.
54. Zhen H, Zhang Y, Fang Z, et al. Toona Sinensis and Moschus Decoction Induced Cell Cycle Arrest in Human Cervical Carcinoma HeLa Cells. Evid Based Complement Alternat Med 2014,2014:121276.
55. Asada R, Kageyama K, Tanaka H, et al. Antitumor and anti-invasive effects of diverse musk-fragrant macrocyclic ketones and their enhancement by hyperthermia. Mol Med Rep 2012, 5(1): 148-152.
56. Si YC, Li Q, Xie CE, et al. Chinese herbs and their active ingredients for activating xue (blood)promote the proliferation and differentiation of neural stem cells and mesenchymal stem cells.Chin Med 2014, 9(1) :13.
57. Yu L, Wang N, Zhang Y, et al. Neuroprotective effect of muscone on glutamate-induced apoptosis in PC12 cells via antioxidant and Ca(2+)antagonism. Neurochem Int 2014, 70(4): 10-21.
58. Wei G, Chen DF, Lai XP, et al. Muscone exerts neuroprotection in an experimental model of stroke via inhibition of the fas pathway. Nat Prod Commun 2012, 7(7): 1069-1074.
59. Meng Y, Xiao Q, Bai JY, et al. Resolution and chiral recognition of muscone as well as actions on neural system. J Asian Nat Prod Res 2014, 16(12):1166-1170.
60. Wu Q, Li H, Wu Y, et al. Protective effects of muscone on ischemia-reperfusion injury in cardiac myocytes. J Ethnopharmacol 2011, 138(1): 34-39.
61. School GSxLYhCJXaFAHoM, et al., Xi AJU.Expressions of Angiogenic Factors in Breast Cancer with Blood Stasis By Musk Ketone Intervention. Journal of Hebei Traditional Chinese Medicine & Pharmacology 2011, 26(2): 40-41.
62. Jaenicke L. Weihrauch und Myrrhe ? Angewandte Chemie 1990, 102(5):594-595.
63. Rijkers T, Ogbazghi W, Wessel M, Bongers F. The effect of tapping for frankincense on sexual reproduction in Boswellia papyrifera. Journal of Applied Ecology 2006, 43(6): 1188-1195.
64. Zhao W, Entschladen F, Liu H, Niggemann B,Fang Q, Zaenker KS, et al. Boswellic acid acetate induces differentiation and apoptosis in highly metastatic melanoma and fibrosarcoma cells.Cancer Detect Prev 2003, 27(1): 67-75.
65. O'Toole C, Price ZH, Ohnuki Y, et al.Ultrastructure, karyology and immunology of a cell line originated from a human transitional-cell carcinoma. Br J Cancer 1978, 38(1): 64-76.
66. Mohamed AKL, Sylvester PW. Anticancer Activity of Boswellia (Frankincense) Essential Oil.Studium Press, 2013, 43-58.
67. Dozmorov MG, Yang Q, Wu W, et al. Differential effects of selective frankincense (Ru Xiang)essential oil versus non-selective sandalwood (Tan Xiang) essential oil on cultured bladder cancer cells: a microarray and bioinformatics study. Chin Med 2014, 9(1): 18.
68. Frank MB, Yang Q, Osban J, et al. Frankincense oil derived from Boswellia carteri induces tumor cell specific cytotoxicity. BMC Complement Altern Med 2009, 9(4): 386-390.
69. Ni X, Suhail MM, Yang Q, et al. Frankincense essential oil prepared from hydrodistillation of Boswellia sacra gum resins induces human pancreatic cancer cell death in cultures and in a xenograft murine model. BMC Complement Altern Med 2012, 12(1): 1-14.
70. Suhail MM, Wu W, Cao A, et al. Boswellia sacra essential oil induces tumor cell-specific apoptosis and suppresses tumor aggressiveness in cultured human breast cancer cells. BMC Complement Altern Med 2011, 11(1): 129.
71. Huang M-T, Badmaev V, Ding Y,et al. Anti-tumor and anti-carcinogenic activities of triterpenoid,β-boswellic acid. Biofactors 2000, 13(1): 225-230.
72. Eichhorn T, Greten HJ, Efferth T. Molecular Determinants of the Response of Tumor Cells to Boswellic Acids. Pharmaceuticals 2011, 4(12):1171-1182.
73. Liu JJ, Nilsson A, Oredsson S, et al. Keto- and acetyl-keto-boswellic acids inhibit proliferation and induce apoptosis in Hep G2 cells via a caspase-8 dependent pathway. Int J Mol Med 2002,10(4): 501-505.
74. Glaser T, Winter S, Groscurth P, et al. Boswellic acids and malignant glioma: induction of apoptosis but no modulation of drug sensitivity. Br J Cancer 1999, 80(5): 756-765.
75. Winking M, Sarikaya S, Rahmanian A, et al.Boswellic acids inhibit glioma growth: a new treatment option? J Neurooncol 2000, 46(2):97-103.
76. Siddiqui MZ. Boswellia serrata, a potential antiinflammatory agent: an overview. Indian J Pharm Sci 2011, 73(3): 255-261.
77. Park B, Sung B, Yadav VR, et al.Acetyl-11-keto-beta-boswellic acid suppresses invasion of pancreatic cancer cells through the downregulation of CXCR4 chemokine receptor expression. Int J Cancer 2011, 129(1): 23-33.
78. Syrovets T, Gschwend JE, Buchele B, et al.Inhibition of IkappaB kinase activity by acetyl-boswellic acids promotes apoptosis in androgen-independent PC-3 prostate cancer cells in vitro and in vivo. J Biol Chem 2005, 280(7):6170-6180.
79. Pang X, Yi Z, Zhang X, et al.Acetyl-11-keto-beta-boswellic acid inhibits prostate tumor growth by suppressing vascular endothelial growth factor receptor 2-mediated angiogenesis. Cancer Res 2009, 69(12):5893-5900.
80. Park YS, Lee JH, Bondar J, et al. Cytotoxic action of acetyl-11-keto-beta-boswellic acid (AKBA) on meningioma cells. Planta Med 2002, 68(5):397-401.
81. Liu JJ, Nilsson A, Oredsson S, et al. Boswellic acids trigger apoptosis via a pathway dependent on caspase-8 activation but independent on Fas/Fas ligand interaction in colon cancer HT-29 cells.Carcinogenesis 2002, 23(12): 2087-2093.
82. Shen Y, Takahashi M, Byun HM, et al. Boswellic acid induces epigenetic alterations by modulating DNA methyla n in colorectal cancer cells. Cancer Biol Ther 2012, 13(7): 542-552.
83. Shao Y, Ho CT, Chin CK, et al. Inhibitory activity of boswellic acids from Boswellia serrata against human leukemia HL-60 cells in culture. Planta Med 1998, 64(4): 328-331.
84. Hoernlein RF, Orlikowsky T, Zehrer C, et al.Acetyl-11-keto-beta-boswellic acid induces apoptosis in HL-60 and CCRF-CEM cells and inhibits topoisomerase I. J Pharmacol Exp Ther 1999, 288(2): 613-619.
85. Estrada AC, Syrovets T, Pitterle K, et al. Tirucallic acids are novel pleckstrin homology domain-dependent Akt inhibitors inducing apoptosis in prostate cancer cells. Mol Pharmacol 2010, 77(3): 378-387.
86. Shishodia S, Harikumar KB, Dass S, et al. The guggul for chronic diseases: ancient medicine,modern targets. Anticancer Res 2008, 28(6A):3647-3664.
87. El Ashry ES, Rashed N, Salama OM, et al.Components, therapeutic value and uses of myrrh.Pharmazie 2003, 58(3): 163-168.
88. Su S, Wang T, Duan JA, et al. Anti-inflammatory and analgesic activity of different extracts of Commiphora myrrha. J Ethnopharmacol 2011,134(2): 251-258.
89. Shoemaker M, Hamilton B, Dairkee SH, et al. In vitro anticancer activity of twelve Chinese medicinal herbs. Phytother Res 2005, 19(7):649-651.
90. al-Harbi MM, Qureshi S, Raza M, et al. Gastric antiulcer and cytoprotective effect of Commiphora molmol in rats. J Ethnopharmacol 1997, 55(2):141-150.
91. Shen T, Lou HX. Bioactive Constituents of Myrrh and Frankincense, Two Simultaneously Prescribed Gum Resins in Chinese Traditional Medicine.Chem Biodivers 2008, 5(4):540-553.
92. Xu J, Guo Y, Zhao P, et al. Four new sesquiterpenes from Commiphora myrrha and their neuroprotective effects. Fitoterapia 2012, 83(4):801-805.
93. Mothana RA, Al-Rehaily AJ, Schultze W.Chemical analysis and biological activity of the essential oils of two endemic Soqotri Commiphora species. Molecules 2010, 15(2): 689-698.
94. Brieskorn CH, Noble P. Constituents of the essential oil of myrrh. Planta Med 1982, 44(2):87-90.
95. Tipton DA, Lyle B, Babich H, et al. In vitro cytotoxic and anti-inflammatory effects of myrrh oil on human gingival fibroblasts and epithelial cells. Toxicol In Vitro 2003, 17(7): 301-310.
96. Wang XL, Kong F, Shen T, et al. Sesquiterpenoids from myrrh inhibit androgen receptor expression and function in human prostate cancer cells. Acta Pharmacol Sin 2011, 32(3): 338-344.
97. Yeo SK, Ali AY, Hayward OA, et al.beta-Bisabolene, a Sesquiterpene from the Essential Oil Extract of Opoponax (Commiphora guidottii), Exhibits Cytotoxicity in Breast Cancer Cell Lines. Phytother Res 2016, 30(3): 418-425.
98. Jakovlev V, Isaac O, Thiemer K, et al.Pharmacological investigations with compounds of chamomile ii. new investigations on the antiphlogistic effects of (-)-alpha-bisabolol and bisabolol oxides (author's transl). Planta Med 1979,35(2): 125-140.
99. Cavalieri E, Mariotto S, Fabrizi C, et al.alpha-Bisabolol, a nontoxic natural compound,strongly induces apoptosis in glioma cells.Biochem Biophys Res Commun 2004, 315(3):589-594.
100. Chen W, Hou J, Yin Y, et al. alpha-Bisabolol induces dose- and time-dependent apoptosis in HepG2 cells via a Fas- and mitochondrial-related pathway, involves p53 and NFkappaB. Biochem Pharmacol 2010, 80(2):247-254.
101. Darra E, Lenaz G, Cavalieri E, et al.Alpha-bisabolol: unexpected plant-derived weapon in the struggle against tumour survival?Ital J Biochem 2007, 56(4): 323-328.
102. Seki T, Kokuryo T, Yokoyama Y, et al. Antitumor effects of alpha-bisabolol against pancreatic cancer. Cancer Sci 2011, 102(12): 2199-2205.
103. Cavalieri E, Rigo A, Bonifacio M, et al.Pro-apoptotic activity of alpha-bisabolol in preclinical models of primary human acute leukemia cells. J Transl Med 2011, 9(11): 45.
104. Darra E, Abdel-Azeim S, Manara A, et al. Insight into the apoptosis-inducing action of alpha-bisabolol towards malignant tumor cells:involvement of lipid rafts and Bid. Arch Biochem Biophys 2008, 476(2): 113-123.
105. Patra SK, Bettuzzi S. Epigenetic DNA-methylation regulation of genes coding for lipid raft-associated components: a role for raft proteins in cell transformation and cancer progression (review). Oncol Rep 2007, 17(6):1279-1290.
106. Bonifacio M, Rigo A, Guardalben E, et al.alpha-bisabolol is an effective proapoptotic agent against BCR-ABL(+) cells in synergism with Imatinib and Nilotinib. PLoS One 2012,7(10): e46674.
107. Gao W, Su X, Dong X, et al.Cycloartan-24-ene-1alpha,2alpha,3beta-triol, a cycloartane-type triterpenoid from the resinous exudates of Commiphora myrrha, induces apoptosis in human prostatic cancer PC-3 cells.Oncol Rep 2015, 33(3): 1107-1114.
108. de Rapper S, Van Vuuren SF, Kamatou GP, et al.The additive and synergistic antimicrobial effects of select frankincense and myrrh oils--a combination from the pharaonic pharmacopoeia.Lett Appl Microbiol 2012, 54(4): 352-358.
109. Shen T, Lou HX. Bioactive constituents of myrrh and frankincense, two simultaneously prescribed gum resins in chinese traditional medicine.Chem Biodivers 2008, 5(4): 540-553.
110. Chen Y, Zhou C, Ge Z, et al.Composition and potential anticancer activities of essential oils obtained from myrrh and frankincense. Oncol Lett 2013, 6(4): 1140-1146.
111. Hong R, Wu YQ, Wu Y. Effects of xihuangwan in assistanttreatment of patients with advanced breast cancer. Chin J Tradit Chin Med 2014,39(6): 1120-1123.
112. Jin J, Zhi HL. Integrated Xihuang Pills and chemotherapy in treating 30 patients with breast cancer. Chin J Tradit Chin Med Pharm 2010,25(5): 715-716.
113. Pan GF. Clinical Research and Experimental Study on Xihuang Pill Treating Breast Cancer based on Estrogen Receptor. Chin J Exp Tradit Med Formul 2012, 18(23): 330-333.
114. Cheng ZQ. Clinical observation on Xihuang Pill in treating 23 cases of advanced primary hepatic cancer. Chin J Tradit Chin Med Pharm 2010,25(1): 53-54.
115. Cheng ZQ, Zhu WT. Clinical observation on Xihuang Pill combined with chemotherapy in treating 18 cases of advanced esophageal cancer.Chin J Tradit Chin Med Pharm 2010,25(8):1302-1304.
116. Zhang Y, Jia YJ, Sun YY, et al. Xihuang Pill unites gemcitabine on the clinical benefit in advanced pancreatic carcinoma. Chin Tradit Patent Med 2010, 32(1): 13-15.
117. Peng C, Tian J, Lv M, et al. Development and validation of a sensitive LC-MS-MS method for the simultaneous determination of multicomponent contents in artificial Calculus Bovis. J Chromatogr Sci 2014, 52(2): 128-136.
118. Yuan H. Pharmacological action of cultured calculus bovis. Chin J Chin Mat Med 1991,16(2): 105-108,128.
119. Shi F, Zhao JH, Liu Y, et al. Preparation and characterization of solid lipid nanoparticles loaded with frankincense and myrrh oil. Int J Nanomedicine 2012, 2012(7): 2033-2043.
猜你喜欢
杂志排行
Traditional Medicine Research的其它文章
- Intestinal obstruction after radical surgery of cervical cancer in a patient with situs inversus
- The mechanism of electro-acupuncture at Shu and Mu acupoints of lung and large intestine meridians for relieving acute gastrointestinal injury in rats with acute pancreatitis
- The regulation of method of tonifying Qi and activating blood circulation in the related gene expressions after spinal cord injury
- Epigenetic regulations of hematopoietic stem cells ageing and the regulation of traditional Chinese medicine
- Two Proved Recipes for Hemostasis
- Tradition and Modern: Public Debate between Traditional Medicine Researcher and Philosopher