颅内微创穿刺血肿引流术治疗老年高血压脑出血的效果及对NT-proBNP、HMGB-1 和GM-CSF水平的影响
2016-09-07伟重庆市第五人民医院神经外科重庆400062
陈 果 董 伟重庆市第五人民医院神经外科,重庆 400062
颅内微创穿刺血肿引流术治疗老年高血压脑出血的效果及对NT-proBNP、HMGB-1 和GM-CSF水平的影响
陈果董伟
重庆市第五人民医院神经外科,重庆400062
目的 探讨颅内微创穿刺血肿引流术治疗老年高血压脑出血的效果及其对N末端脑钠肽前体 (NT-proBNP)、高迁移率族蛋白1(HMGB-1)和血浆粒细胞巨噬细胞集落刺激因子(GM-CSF)水平的影响。方法 选取2009年2月~2015年6月重庆市第五人民医院神经外科诊治的82例急性老年高血压脑出血患者为研究对象,根据手术方式的不同将患者分为颅内微创穿刺血肿引流术组(微创组)和小骨窗血肿清除术/去骨瓣减压血肿清除术(常规组),每组各41例,分别比较两组患者的临床疗效及其NT-proBNP、HMGB-1和GM-CSF的变化水平。结果 术后7 d和14 d,两组出血量均较术前显著下降(P<0.05),但两组组间比较差异无统计学意义(P>0.05)。术后14 d常规组格拉斯哥昏迷评分(GCS)和Barthel指数均较术前明显升高,而美国国立卫生研究院卒中量表(NIHSS)评分显著降低(P<0.05);微创组上述三项指标术后7 d即出现明显改善(P<0.05),且术后14 d GCS评分和Barthel指数明显高于常规组,而NIHSS评分则显著低于常规组 (P<0.05)。术后微创组治疗有效率为75.61%(31/41),显著高于常规组的41.46%(17/41)(P<0.05),但两组并发症发生率比较差异无统计学意义(P>0.05)。术后7 d和14 d,微创组NT-proBNP、HMGB-1和GM-CSF水平均较术前显著下降(P<0.05);常规组仅在术后14 d上述指标水平才出现明显降低(P<0.05);而且,微创组患者NT-proBNP、HMGB-1和GM-CSF水平均显著低于常规组(P<0.05)。结论 颅内微创穿刺血肿引流术可以有效清除老年高血压脑出血患者的出血病灶,调节脑内NT-proBNP、HMGB-1和GM-CSF水平,促进神经功能的恢复和生活质量的提高。
颅内微创穿刺血肿引流术;高血压脑出血;N末端脑钠肽前体;高迁移率族蛋白1;粒细胞巨噬细胞集落刺激因子
高血压脑出血是神经系统常见的老年性疾病,占全部脑卒中的20%~30%,具有较高的病死率和致残率,严重威胁患者的生命健康[1]。传统的内科保守治疗和开颅清除血肿的外科治疗方式虽然能在一定程度上降低患者的病死率,但疾病预后并不理想,绝大多数患者治疗后无法正常自理生活或神经功能受到严重损害[2-3]。颅内微创穿刺血肿引流术是国内外较为认可的治疗高血压脑出血的微创手术方法,但该术式对老年患者是否也有较好的疗效尚未明确[4]。据此,本研究以82例老年高血压脑出血患者为研究对象,探讨颅内微创穿刺血肿引流术的治疗效果及其对N末端脑钠肽前体(NT-proBNP)、高迁移率族蛋白1(HMGB-1)和血浆粒细胞巨噬细胞集落刺激因子(GM-CSF)等潜在脑出血标志物水平的影响。现总结报道如下:
1 资料与方法
1.1一般资料
选取2009年2月~2015年6月重庆市第五人民医院神经外科诊治的82例急性老年高血压脑出血患者为研究对象,其中男49例,女33例,年龄60~79岁,平均(63.12±5.85)岁。所有患者均经头颅CT或核共振成像(MRI)影像学证实,诊断标准严格依据全国第4届脑血管病学术会议制订的高血压脑出血标准[5]执行。血肿部分:基底节52例,丘脑16例,脑叶14例;格拉斯哥昏迷评分(GCS):>12分 20例,8~12分45例,<8分17例;出血量(以多田氏公式计算):30~<50 mL 44例,50~<70 mL 29例,≥70 mL 9例;纳入标准:①首次发病,入院时间24 h以内;②未罹患有血管畸形、出血破入脑室、蛛网膜下腔出血、凝血功能障碍和其他严重慢性疾病等;③心、肺、肝、肾功能检查未发现显著异常;④发病前无明显的神经认知功能障碍;⑤无明显手术禁忌,愿意参与本研究,且依从性良好。本研究方案通过医院伦理委员会批准,所有患者及家属均知情本研究且签署知情同意书。根据手术方式的不同,将患者分为颅内微创穿刺血肿引流术组(微创组)和小骨窗血肿清除术/去骨瓣减压血肿清除术 (常规组),每组各41例。两组患者年龄、性别、入院时间、GCS评分、出血部位、出血量等一般资料比较,差异均无统计学意义(P>0.05),具有可比性。见表1。

表1 两组一般资料比较
1.2手术方法
所有患者入院后给予常规脱水降低颅内压、控制血压、营养神经、控制感染、维持水电解质平衡和防治上消化道出血等对症处理治疗。其中,微创组患者予以剃光头发,常规消毒,局部麻醉,采用开颅电钻钻孔,在电钻的驱动下将适当的穿刺针长度的YL-1型一次性颅内血肿碎吸针垂直插入,穿过颅骨和硬脑膜,当穿刺针有明显下降感时卸下电钻和钻头,取下针芯,改用钝圆头针芯边抽边转动针头,充分抽吸瘀血并慢慢伸入血肿的中心位置,退出针芯,可见陈旧性血液流出,盖上螺帽,接上引流管,用注射器轻柔地抽出颅内液化部分的血肿,插入针型血肿粉碎器,利用生理盐水和肝素反复冲洗至流出液变清,加入尿激酶,夹闭引流管4~6 h后开放引流,复查头颅CT或MRI,待血肿基本消失后拔除穿刺针。常规组患者则在全麻插管下采用去骨瓣减压或小骨窗血肿清除术对血肿进行清除,其余治疗方式与微创组保持一致。
1.3观察指标及检测方法
1.3.1临床疗效评估①分别于术前、术后7 d和14 d行头颅CT或MRI检查患者,依据多田公式计算血肿大小。②应用GCS评分检测患者的临床状态、并发症发生和术后再出血情况。③利用格拉斯哥结局量表(GOS)评价患者的预后情况:恢复良好:能独立生活、工作,但仍有缺陷;轻度残疾:有思维、言语障碍等,残疾,但尚能独立生活、工作;重度残疾:有意识,残疾,日常生活需要照料;植物生存或死亡:仅有最小反应,如随着睡眠/清醒周期,眼睛能睁开。治疗有效=恢复良好+轻度残疾。④采用Barthel指数测量患者术后日常生活能力。⑤采用美国国立卫生研究院卒中量表(national institute of health stroke scale,NIHSS)评价患者神经功能的损伤程度。
1.3.2血浆NT-p roBNP、HMGB-1和GM-CSF的检测分别于术前、术后7 d和14 d三个时间点采集所有患者的清晨空腹静脉血液,利用免疫层析法测定NT-proBNP的水平,试剂盒购于武汉明德生物科技有限公司;采用酶联免疫吸附测定(ELISA)法测定HMGB-1 和GM-CSF的变化水平,试剂盒分别购自于厦门慧嘉生物科技有限公司和美国Invitrogen公司。
1.4统计学方法
所有数据均采用SPSS 18.0软件予以整理和分析。其中,计量资料以均数±标准差(±s)表示,两组间比较采用独立样本Student-t检验,治疗前后比较应用配对Student-t检验;多个时间点的比较采用重复测量的方差分析,两组间比较利用LSD-t检验;计数资料以构成比或率比较,两组间比较采用χ2检验或Fisher确切概率法。以P<0.05为差异有统计学意义。
2 结果
2.1两组临床疗效比较
术后7 d和14 d,两组出血量均较术前显著下降(P<0.05),但两组组间比较差异无统计学意义(P>0.05)。术后14 d常规组GCS评分和Barthel指数均较术前明显升高,而NIHSS评分显著降低(P<0.05);微创组上述三项指标术后7 d即出现明显改善(P<0.05),且术后14 d微创组GCS评分和Barthel指数明显高于常规组,而NIHSS评分则显著低于常规组(P<0.05)。见表2。
表2 两组临床疗效比较(±s)

表2 两组临床疗效比较(±s)
注:与本组术前比较,*P<0.05;与常规组比较,#P<0.05;GCS:格拉斯哥昏迷评分;NIHSS:美国国立卫生研究院卒中量表
组别 出血量(mL)GCS评分(分)NIHSS评分(分)Barthel指数(分)微创组(n=41)术前术后7 d术后14 d常规组(n=41)术前术后7 d术后14 d F值P值52.94±10.58 5.59±1.45*1.42±0.63*8.38±1.48 10.52±1.65*12.89±1.80*#12.58±3.76 8.49±2.64*4.11±1.40*#34.89±5.68 46.18±6.37*60.74±8.19*#53.21±11.61 7.98±1.96*2.15±0.89*0.753 <0.01 8.49±1.51 9.22±1.76 10.84±1.81*12.520 <0.01 12.74±3.10 10.28±2.59 6.50±1.24*6.304 <0.01 35.01±5.43 38.28±5.62 45.93±6.90*9.854 <0.01
2.2两组预后评价比较
手术结束后,微创组治疗有效率为75.61%(31/41),显著高于常规组的41.46%(17/41),差异有统计学意义(P<0.05)。见表3。
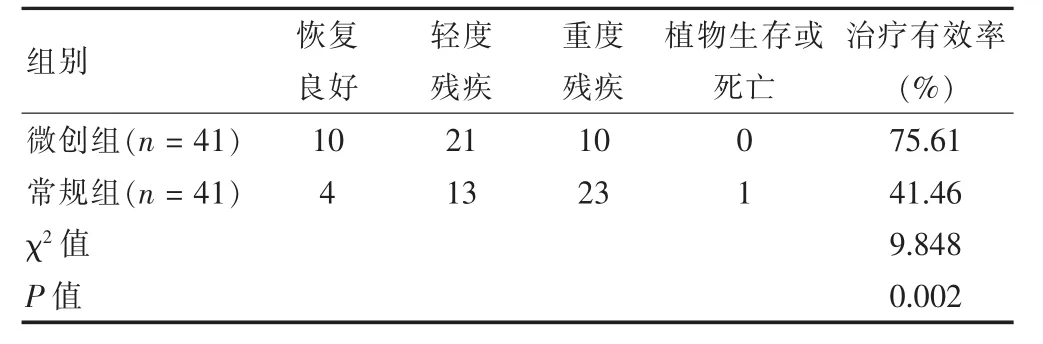
表3 两组预后评价比较(例)
2.3两组并发症发生情况比较
微创组并发症发生率虽略低于常规组,但两组组间比较差异无统计学意义(P>0.05)。见表4。

表4 两组并发症发生情况比较(例)
2.4两组血浆NT-proBNP、HMGB-1和GM-CSF水平比较
术后7 d和14 d,微创组NT-proBNP、HMGB-1和GM-CSF水平均较术前显著下降(P<0.05);常规组仅在术后14 d上述指标水平才出现明显降低(P<0.05);而且,微创组患者NT-proBNP、HMGB-1和GM-CSF水平均显著低于常规组(P<0.05)。见表5。
表5 两组血浆NT-proBNP、HMGB-1和GM-CSF平比较(±s)

表5 两组血浆NT-proBNP、HMGB-1和GM-CSF平比较(±s)
注:与本组术前比较,*P<0.05;与常规组比较,#P<0.05;NT-proBNP:N末端脑钠肽前体;HMGB-1:高迁移率族蛋白1;GM-CSF:血浆粒细胞巨噬细胞集落刺激因子
组别 NT-proBNP (pg/mL)HMGB-1 (ng/mL)GM-CSF (pg/mL)微创组(n=41)术前术后7 d术后14 d常规组(n=41)术前术后7 d术后14 d F值P值321.52±34.05 240.58±21.68*166.25±18.23*#21.85±3.97 10.57±1.89*6.29±1.12*#6.94±1.87 2.58±1.02*1.49±0.45*#319.82±31.96 270.58±28.12 205.75±19.07*20.753 <0.01 21.67±3.65 19.28±3.05 14.68±2.84*14.484 <0.01 7.16±1.95 5.28±1.76 4.11±1.59*5.591 <0.05
3 讨论
手术治疗是高血压脑出血患者的首选治疗方法,尤其是以微创钻孔引流为代表的微创外科手术方式,具有低侵袭性、高清除率和术后康复快等优势,正逐步受到认可,操作技术也日臻完善[6-8]。传统的开颅脑内血肿清除术虽然可以较为彻底地清除血肿,降低颅内高压,缓解病情,但对周围正常脑组织的损害仍较大,多数患者预后生存质量并不佳[9-10]。加之,老年高血压脑出血患者相比其他年龄段患者而言具有一定的特殊性,其体质和免疫力较低下,多器官功能衰退导致病情进展的不确定性和反复性更大,因此,手术方式的选择被认为是影响老年高血压脑出血患者预后的重要因素[11-13]。微创颅内血肿清除术在局麻的条件下定向穿刺,可以有效避免颅内正常脑组织再损伤和出血,也能够有效遏制感染的发生[14-16]。本研究采用颅内微创穿刺血肿引流术进行脑内的血肿清除,结果发现,微创组老年患者术后出血量明显少于常规组,而且GCS评分和NIHSS评分恢复速度也明显优于常规组,表明微创穿刺血肿引流术可显著减轻患者术后的临床症状,改善神经功能,促进疾病的康复。而且,微创组患者术后14 d的Barthel指数也显著高于常规组,由于本研究的观测随访时间偏短,因此在术后14 d的Barthel指数检测值相对较低,但该结果仍充分提示,微创穿刺血肿引流术能够减少患者致残率,提高术后生活自理的能力。GOS量表检测显示,微创组恢复良好+轻度残疾的患者数量明显高于常规组,说明微创手术不仅临床疗效较佳,对改善老年高血压脑出血的预后也具有积极作用。
NT-proBNP被认为是与蛛网膜下腔出血、高血压脑出血和心源性脑栓塞等多种脑血管事件密切相关的分子[17-18]。本研究结果显示,治疗后两组患者的NT-proBNP水平均明显降低,而且微创组术后14 d NT-proBNP水平显著低于常规组,表明NT-proBNP含量的增加可在一定程度上反映颅内缺血缺氧性损伤的严重程度,NT-proBNP水平越高,患者的预后和疗效也相对越差。HMGB-1和GM-CSF均是反映颅内免疫-炎性反应水平的关键指标,对指示患者体内炎症蛋白和相关因子的水平具有重要的意义[19-20]。本研究结果显示,术后两组患者HMGB-1和GM-CSF的水平均明显下降,而微创组患者术后7 d即显著改善,并且在术后14 d时较常规组更低,提示患者体内的免疫-炎症级联反应水平得到明显抑制,这一方面表明微创手术对控制和降低感染风险有积极作用,另一方面也说明临床上可以借助检测特异性炎症因子的水平判定疾病的疗效或预后。
[1]Mirsen T.Acute treatment of hypertensive intracerebral hemorrhage[J].Curr Treat Options Neurol,2010,12(6):504-517.
[2]Antihypertensive Treatment of Acute Cerebral Hemorrhage (ATACH)investigators.Antihypertensive treatment of acute cerebral hemorrhage[J].Crit Care Med,2010,38(2):637-648.
[3]Qureshi AI,Palesch YY.Antihypertensive treatment of acute cerebral hemorrhage(ATACH)Ⅱ:design,methods,and rationale[J].Neurocrit Care,2011,15(3):559-576.
[4]Keep RF,Hua Y,Xi G.Intracerebral haemorrhage:mechanisms of injury and therapeutic targets[J].Lancet Neurol,2012,11(8):720-731.
[5]全国第四届脑血管病学术会议.各类脑血管疾病诊断要点及临床功能缺损程度评分标准(1995)[J].中华神经科杂志,1996,29(6):379-383.
[6]Elliott J,Smith M.The acute management of intracerebral hemorrhage:a clinical review[J].Anesth Analg,2010,110 (5):1419-1427.
[7]Mould WA,Carhuapoma JR,Muschelli J,et al.Minimally invasive surgery plus recombinant tissue-type plasminogen activator for intracerebral hemorrhage evacuation decreases perihematomal edema[J].Stroke,2013,44(3):627-634.
[8]Mazya M,Egido JA,Ford GA,et al.Predicting the risk of symptomatic intracerebral hemorrhage in ischemic stroke treated with intravenous alteplase Safe Implementation of Treatments in Stroke(SITS)symptomatic intracerebral hemorrhage risk score[J].Stroke,2012,43(6):1524-1531.
[9]Adeoye O,Broderick JP.Advances in the management of intracerebral hemorrhage[J].NatRev Neurol,2010,6(11):593-601.
[10]Steiner T,Juvela S,Unterberg A,et al.European Stroke Organization guidelines for the management of intracranial aneurysms and subarachnoid haemorrhage[J].Cerebrovasc Dis,2013,35(2):93-112.
[11]Raposo N,Viguier A,Cuvinciuc V,et al.Cortical subarachnoid haemorrhage in the elderly:a recurrent event probably related to cerebral amyloid angiopathy[J].Eur JNeurol,2011,18(4):597-603.
[12]Skolarus LE,Morgenstern LB,Zahuranec DB,et al.Acute care and long-term mortality among elderly patients with intracerebral hemorrhage who undergo chronic life-sustaining procedures[J].JStroke Cerebrovasc Dis,2013,22 (1):15-21.
[13]Jüttler,E,Unterberg A,Woitzik J,et al.Hemicraniectomy in older patients with extensive middle-cerebral-artery stroke[J].New Eng JMed,2014,370(12):1091-1100.
[14]Pearce LA,McClure LA,Anderson DC,et al.Effects of long-term blood pressure lowering and dual antiplatelet treatment on cognitive function in patients with recent lacunar stroke:a secondary analysis from the SPS3 randomised trial[J].LancetNeurol,2014,13(12):1177-1185.
[15]Steiner T,Al-Shahi Salman R,Beer R,et al.European Stroke Organisation(ESO)guidelines for the management of spontaneous intracerebral hemorrhage[J].Int JStroke,2014,9(7):840-855.
[16]van Asch CJ,Luitse MJ,Rinkel GJ,et al.Incidence,case fatality,and functional outcome of intracerebral haemorrhage over time,according to age,sex,and ethnic origin:a systematic review andmeta-analysis[J].Lancet Neurol,2010,9(2):167-176.
[17]Chang L,Yan H,Li H,et al.N-terminal probrain natriuretic peptide levels as a predictor of functional outcomes in patients with ischemic stroke[J].Neuro Report,2014,25(13):985-990.
[18]Chaitanya M,Hassan A,Arihiro S,et al.Obesity and natriuretic peptides,BNPand NT-proBNP:Mechanisms and diagnostic implications for heart failure[J].Int J Cardiol,2014,176(3):611-617.
[19]Laird MD,Shields JS,Sukumari-Ramesh S,et al.High mobility group box protein-1 promotes cerebral edema after traumatic brain injury via activation of toll-like receptor 4[J].Glia,2014,62(1):26-38.
[20]Kallmünzer B,TauchiM,Schlachetzki JC,et al.Granulocyte colony-stimulating factor does not promote neurogenesis after experimental intracerebral haemorrhage[J]. Int JStroke,2014,9(6):783-788.
Clinical effect of minimally invasive hematoma drainage in the treatment of elderly patients with hypertensive cerebral hemorrhage and its effect on the levels of NT-proBNP,HMGB-1 and GM-CSF
CHEN Guo DONGWei
Department of Neurosurgery,the Fifth People's Hospital of Chongqing,Chongqing400062,China
Objective To investigate the clinical effect of minimally invasive hematoma drainage in the treatment of elderly patients with hypertension cerebral hemorrhage and its effect on the levels of N-terminal pro-B-type natriuretic peptide(NT-proBNP),highmobility group box-1 protein(HMGB-1)and granulocyte-macrophage colony-stimulating factor(GM-CSF).Methods Eighty two cases of elderly patients with acute hypertensive cerebral hemorrhage treated in Department of Neurosurgery of the Fifth People's Hospital of Chongqing from February 2009 to June 2015 were selected as research objects,and they were divided into minimally invasive intracranial hematoma puncture drainage surgery group(minimally invasive group)and small bone window hematoma/craniotomy hematoma surgery group(conventional group)according to different surgical procedures,each group had 41 cases.The clinical efficacy and the levels of NT-proBNP,HMGB-1 and GM-CSF were compared respectively between two groups.Results After operation for 7 days and 14 days,the bleeding volume of the two groups were significantly decreased compared with be-fore operation(P<0.05),but there were no significant differences between the two groups(P>0.05).After operation for 14 days,the Glasgow coma scale(GCS)and Barthel index in the conventional group were significantly increased compared with before operation,whereas the national institute of health stroke scale(NIHSS)was markedly decreased (P<0.05);the three indexes above in the minimally invasive group were significantly improved after operation for 7 days(P<0.05,and the GCS score and Barthel index at 14 days after operation of minimally invasive group were significantly higher than those of conventional group,while the NIHSS score was significantly lower than that of the conventional group(P<0.05).The effective rate of minimally invasive group was 75.61%(31/41),which was significantly higher than that of the conventional group[41.46%(17/41)](P<0.05),but there was no statistically significant difference of the incidence of complications between the two groups(P>0.05).After operation for 7 days and 14 days,the levels of NT-proBNP,HMGB-1 and GM-CSFwere significantly decreased compared with those before operation(P<0.05);however,the levels of these indicators above were significantly decreased only at 14 days after operation(P<0.05),and the levels of NT-proBNP,HMGB-1 and GM-CSF in the minimally invasive group were significantly lower than those of conventional group(P<0.05).Conclusion Intracranial hematoma drainage can effectively remove the bleeding lesions in elderly patients with hypertensive cerebral hemorrhage,adjust the level of NT-proBNP,HMGB-1 and GM-CSF,and thus promote the recovery of neurological function and improve the quality of life.
Intracranial hematoma drainage;Hypertensive cerebral hemorrhage;N-terminal pro-B-type natriuretic peptide;Highmobility group box-1 protein;Granulocyte-macrophage colony-stimulating factor
R743.2
A
1673-7210(2016)01(b)-0041-05
2015-10-15本文编辑:张瑜杰)
重庆市卫生和计划生育委员会医学科研计划项目(SZX2015187)。
陈果(1973.10-),男,硕士研究生;研究方向:微创血肿清除术治疗老年高血压脑出血的效果。
董伟(1969.3-),男,副主任医师;研究方向:微创血肿清除术治疗老年高血压脑出血的效果。
