前庭阵发症的临床特征及其误诊原因分析
2016-09-05孔卫国
孔卫国
·诊治分析·
前庭阵发症的临床特征及其误诊原因分析
孔卫国
目的分析前庭阵发症的临床特征及其误诊原因。方法选取2012年1月—2015年8月宣城市人民医院门诊及住院患者中最终确诊为前庭阵发症的患者11例,回顾性分析其临床资料,总结其临床特征及误诊原因。结果(1)临床症状:发作性眩晕、头晕10例,耳鸣4例,步态不稳3例,听力减退2例;伴恶心、呕吐、上腹部不适症状10例。自述症状持续时间:6例患者症状持续时间<10 min,3例患者症状持续时间为10 min~1 h,2例患者症状持续时间>1 h。症状发作频率:10~50次/月。发作时体格检查:眼震11例,以水平眼震为主,无其他神经系统异常体征。磁共振检查:前庭蜗神经与血管交互压迫6例。电测听检查:听力减退5例,其中单耳听力减退4例,双耳听力减退1例;轻度减退3例,明显减退2例。脑干听觉诱发电位(BAEP)检查:Ⅰ~Ⅲ波峰间期延长6例。(2)诊治及误诊情况:11例患者入院后首次诊断为良性阵发性位置性眩晕(BPPV)者5例,予以手法复位治疗;首次诊断为焦虑状态2例,予以抗焦虑治疗;首次诊断为后循环缺血(PCI)、脑供血不足各1例,予以预防卒中、改善循环治疗;首次诊断为突发性耳聋1例,予以扩张血管、营养神经治疗;首次诊断为梅尼埃病1例,予以脱水、营养神经治疗。首次诊断至最终明确诊断为前庭阵发症时间为3~10 d,平均(7.2±2.1)d。3例患者依据临床症状、实验室检查明确诊断,其余8例患者均在抗癫痫药物治疗有效后结合病史明确诊断;11例患者经治疗后临床症状均有不同程度缓解。结论前庭阵发症的临床症状以发作性眩晕、头晕为主,磁共振检查多显示前庭蜗神经与血管交互压迫,BAEP检查结果多显示Ⅰ~Ⅲ波峰间期延长;前庭阵发症的临床误诊率较高的原因与临床医生认识不足、患者病史提供不准确、临床症状缺乏特异性及缺少特异性实验室检查手段有关。
前庭疾病;眩晕;误诊
孔卫国.前庭阵发症的临床特征及其误诊原因分析[J].实用心脑肺血管病杂志,2016,24(2):106-108.[www.syxnf.net]
Kong WG.Clinical features and causes of misdiagnosis of vestibular paroxysmia[J].Practical Journal of Cardiac Cerebral Pneumal and Vascular Disease,2016,24(2):106-108.
前庭阵发症(vestibular paroxysmia)最早于1975年由Jannetta医生首次发现[1],于1994年被正式命名并确定诊断标准[2]。前庭阵发症发病率较低,且缺乏特异性临床症状,又无明确的实验室检查以明确诊断,因此导致该病的确诊较困难,误诊率较高。本文对宣城市人民医院门诊及住院患者中最终确诊为前庭阵发症的患者进行临床特征及其误诊原因分析,以期为前庭阵发症的早期诊断和治疗提供资料参考,现报道如下。
1 资料与方法
1.1一般资料选取2012年1月—2015年8月宣城市人民医院门诊及住院患者中最终确诊为前庭阵发症的患者11例,其中男4例,女7例;年龄25~70岁,平均年龄(49.2±13.0)岁。
1.2诊断标准参照2008年Hüfner等[3]提出的前庭阵发症的诊断标准,具体如下:至少发生5次眩晕,且发作时具有以下特点:(1)未经治疗,眩晕发作持续数秒至数分钟;(2)眩晕在静息时或某种体位时发作;(3)眩晕发作时至少具备以下1项:①无伴随症状,②姿势不稳,③步态不稳,④单侧耳鸣,⑤单侧耳闷或耳周麻木感,⑥单侧听力下降;(4)以下项目至少具备1项:①桥小脑角区磁共振成像(MRI)平扫提示神经血管交互压迫,②过度换气试验诱发眼震,③眼震电图发现前庭功能不足加重,④抗癫痫药物治疗有效;(5)排除其他疾病或无法应用其他疾病解释上述症状。
1.3方法回顾性分析患者的临床资料。患者入院后均进行问诊、体格检查;均完成1.5T MRI+磁共振血管造影(MRA)检查,观察是否存在前庭蜗神经与血管交互压迫;均完善纯音电测听仪和脑干听觉诱发电位(BAEP)检查,观察是否存在听力改变和BAEP异常。明确诊断后均使用抗癫痫药物(卡马西平、奥卡西平)治疗,并观察药物治疗效果。
2 结果
2.1临床特征临床症状:发作性眩晕、头晕10例,耳鸣4例,步态不稳3例,听力减退2例;伴恶心、呕吐、上腹部不适症状10例。自述症状持续时间:6例患者持续时间<10 min,3例患者持续时间为10 min~1 h,2例患者持续时间>1 h(症状持续时间均为患者自述,可能不准确)。症状发作频率:10~50次/月。发作时体格检查:眼震11例,以水平眼震为主,无其他神经系统异常体征。磁共振检查:前庭蜗神经与血管交互压迫6例。电测听检查:听力减退5例,其中单耳听力减退4例,双耳听力减退1例;轻度减退3例,明显减退2例。BAEP检查:Ⅰ~Ⅲ波峰间期延长6例。具体见表1。
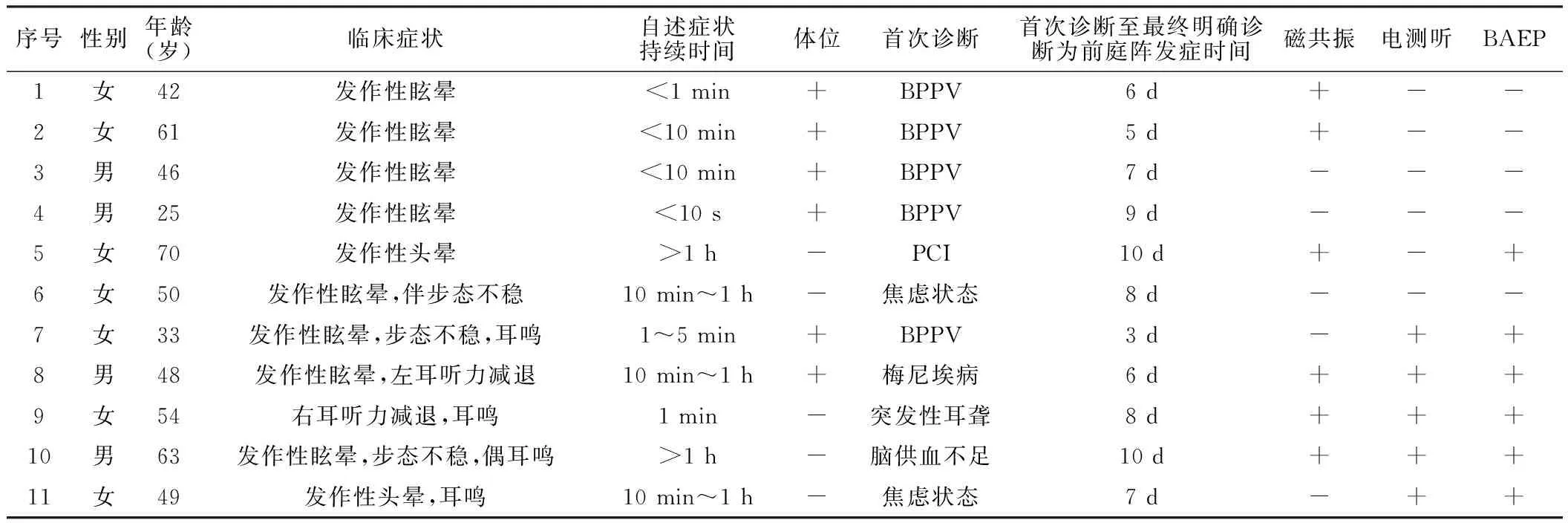
表1 11例前庭阵发症患者临床特征
注:体位“+”表示体位变化诱发症状,“-”表示体位变化不诱发症状;磁共振“+”表示前庭蜗神经与血管交互压迫,“-”表示无前庭蜗神经与血管交互压迫;电测听“+”表示出现听力减退,“-”表示未出现听力减退;BAEP“+”表示发现异常,“-”表示未发现异常;BAEP=脑干听觉神经诱发电位,BPPV=良性阵发性位置性眩晕,PCI=后循环缺血
2.2诊治及误诊情况11例患者入院后首次诊断为良性阵发性位置性眩晕(BPPV)5例,予以手法复位治疗;首次诊断为焦虑状态2例,予以抗焦虑治疗;首次诊断为后循环缺血(PCI)、脑供血不足各1例,予以预防卒中、改善循环治疗;首次诊断为突发性耳聋1例,予以扩张血管、营养神经治疗;首次诊断为梅尼埃病1例,予以脱水、营养神经治疗。首次诊断至最终明确诊断前庭阵发症时间为3~10 d,平均(7.2±2.1)d。3例患者依据临床症状、实验室检查明确诊断,其余8例患者均在抗癫痫药物(卡马西平、奥卡西平)治疗有效后结合病史明确诊断;11例患者经治疗后临床症状均有不同程度缓解。
3 讨论
眩晕是临床常见症状,常见病因有BPPV、梅尼埃病、前庭神经炎、PCI、精神性眩晕等,其中前庭阵发症相对少见。有调查研究显示,前庭阵发症占头晕专病门诊就诊患者的3.2%[4]。临床医师接触前庭阵发症较少,对该病认识相对不足,因此误诊率较高,尤其在基层医院。本文报道的11例患者中,入院后首次诊断均不准确,明确诊断为前庭阵发症的时间平均>1周,其中8例为药物治疗好转后反推确诊。面对该病的诊疗现状,其误诊原因除临床医师对前庭阵发症认识不足之外,前庭阵发症的临床症状不典型、缺乏可以明确诊断的特异性实验室检查也是误诊原因之一。
前庭阵发症的常见临床表现为反复发作的短暂性眩晕,且体位变化可诱发症状发作,发作形式非常类似BPPV。本文中有5例患者初次诊断为BPPV,建议遇到体位诱发试验结果不典型、手法复位效果不佳的患者,需警惕前庭阵发症的可能。一般情况下,听力下降或耳鸣的患者易被误诊为梅尼埃病、突发性耳聋,可以结合电测听和BAEP检查进行鉴别诊断。李艳成等[5]对51例前庭阵发症患者的BAEP结果进行回顾性分析,发现前庭阵发症患者BAEP异常率较高,且以Ⅰ~Ⅲ波峰间期延长为主,Ⅰ~Ⅲ波峰间期延长或其耳间差延长均提示蜗神经受累,且病程越长,Ⅰ~Ⅲ波峰间期及其耳间差延长越明显,蜗神经损害越不可逆,并提出BAEP有助于诊断和评价前庭阵发症的严重程度。临床中多数疾病可引发患者听力损害,因此遇到听力损害的患者建议耳鼻喉科会诊以进行鉴别诊断。眩晕患者常伴焦虑情绪,而精神心理相关性眩晕、头晕临床较常见,故前庭阵发症易被误诊为焦虑状态。抗焦虑和镇静治疗亦能缓解部分患者的临床症状,因此易使临床医师坚持错误的诊断。笔者认为精神心理相关性眩晕应作为排他性诊断,临床诊断不能先入为主,尤其是抗焦虑治疗效果不佳时,应考虑诊断的准确性。患者在眩晕发作时不适感较强,因此不能准确自述,甚至对医师详细问诊有抵触和反感情绪,因此临床医生应注意安抚,使患者配合问诊。
前庭阵发症的发病机制尚未明确,可能由前庭蜗神经与血管交互压迫引起。Hüfner等[3]研究结果显示,95%的前庭阵发症患者存在神经与血管交互压迫,李艳成等[6]对51例前庭阵发症患者采用MRI三维稳态进动快速成像序列(3D-FIESTA)对桥小脑角区轴位扫描,结果显示42例患者存在神经与血管交互压迫,其中单侧37例,双侧5 例。李慧等[7]采用三维-磁共振血管成像技术分别对28例前庭阵发症及对照组患者进行扫描,结果显示前庭阵发症患者神经与血管交互压迫发生率高,且压迫血管以小脑前下动脉多见。本文中6例患者发现前庭蜗神经与血管交互压迫,检出率较低,分析原因为:(1)MRI普通平扫检出率较低,建议采用局部薄层扫描以增加检出率;(2)1.5T MRI分辨率较低,建议使用高分辨率MRI;(3)临床医生未能识别。本文3例患者在明确诊断后再次阅片发现前庭蜗神经与血管交互压迫,因此提高临床医生对前庭阵发症的鉴别诊断意识意义重大。
临床治疗前庭阵发症首选卡马西平[3],对于卡马西平不耐受的患者可以选用奥卡西平、加巴喷汀、丙戊酸或苯妥英钠[8]。Russell等[9]研究结果显示,低剂量加巴喷汀(600 mg/d)对前庭阵发症有较好的控制效果。
综上所述,前庭阵发症的临床症状以发作性眩晕、头晕为主,磁共振检查多显示前庭蜗神经与血管交互压迫,BAEP检查结果多显示Ⅰ~Ⅲ波峰间期延长;前庭阵发症的临床误诊率高的原因与临床医生认识不足、患者病史提供不准确、临床症状缺乏特异性、缺少高效特异的实验室检查手段有关。因此,快速明确诊断前庭阵发症需加强临床医师对前庭阵发症临床特点的了解,从而减轻患者的经济、精神负担。
[1]Jannetta PJ.Neurovascular cross-compression in patients with hyperactive dysfunction symptoms of the eighth cranial nerve[J].Surg Forum,1975(26):467-469.
[2]Brandt T,Dieterich M.Vestibular paroxysmia: vascular compression of the eighth nerve?[J].Lancet,1994,343(8900):798-799.
[3]Hüfner K,Barresi D,Glaser M,et al.Vestibular paroxysmia:diagnostic features and medical treatment[J].Neurology,2008,71(13):1006-1014.
[4]Brandt T,Strupp M.Migraine and vertigo: classification,clinical features and special treatment considerations[J].Headache Currents,2006,3(1):12-19.
[5]李艳成,徐瑾,陈瑛,等.前庭阵发症脑干听觉诱发电位的特点[J].临床神经病学杂志,2012,25(1):57-59.
[6]李艳成,徐瑾,贺琦,等.前庭阵发症的影像学特点[J].临床神经病学杂志,2013,26(1):63-65.
[7]李慧,刘春岭,张超,等.28例前庭阵发症的MRI表现分析[J].中风与神经疾病杂志,2014,31(5):426-428.
[8]Brandt T,Huppert T,Hufner K,et al.Long-term course and relapses of vestibular and balance disorders[J].Restor Neurol Neurosci,2010,28(1):69-82.
[9]Russell D,Baloh RW.Gabapentin responsive audiovestibular paroxysmia[J].J Neurol Sci,2009,281(1/2):99-100.
(本文编辑:毛亚敏)
Clinical Features and Causes of Misdiagnosis of Vestibular Paroxysmia
KONGWei-guo.
DepartmentofNeurology,thePeople′sHospitalofXuancheng,Xuancheng242000,China
ObjectiveTo analyze the clinical features and causes of misdiagnosis of vestibular paroxysmia.MethodsA total of 11 outpatients and inpatients were selected in the People′s Hospital of Xuancheng,and their clinical data was retrospectively analyzed,clinical features and causes of misdiagnosis summarized.Results(1)Clinical symptoms:10 cases performed as episodic vertigo and dizziness,4 cases performed as tinnitus,3 cases performed as instability of gait,2 cases performed as dysacusis;10 cases complicated with nausea,emesis and epigastric discomfort.Self-reported symptoms duration:6 cases within 10 minutes,3 cases from 10 minutes to 1 hour,2 cases over 1 hour.Symptoms attack frequency:10 to 50 times per month.Physical examination at attack showed that,11 cases performed as nystagmus,that mainly were horizontal nystagmus without any other abnormal signs of nervous system.Magnetic resonance inspection(MRI)found 6 cases with interactive oppression of vestibulocochlear nerve and blood vessel;electro-audiometry found 5 cases with dysacusis,including 4 cases with monaural dysacusis and 1 case with binaural dysacusis,thereinto 3 cases were mild,1 case was obvious.Brainstem auditory evoked potential(BAEP)examination found 6 cases with latency of Ⅰ to Ⅲ inter-peak.Diagnosis,treatment and misdiagnosis:5 cases were firstly diagnosed as benign paroxysmal positional vertigo(BPPV)and were treated by manual reposition;2 cases were firstly diagnosed as anxiety and were treated by anti-anxiety treatment;1 case was firstly diagnosed as posterior circulation ischemia(PCI),1 case was firstly diagnosed as cerebral insufficiency,both of them were treated by prevention of stroke and improvement of blood circulation;1 case was firstly diagnosed as sudden deafness and was treated by expansion of blood vessel and nutrition of nerve;1 case was firstly diagnosed as Meniere′s disease and was treated by diuresis and nutrition of nerve.The duration between first diagnosis and final definite diagnosis was 3 to 10 days,average at(7.2±2.1)days.Of the 11 cases,3 cases clarified a diagnosis according to clinical symptoms and laboratory examination,other 8 cases clarified a diagnosis according to the effectiveness of antiepileptic drugs combined with medical history,all of their clinical symptoms relieved to varying degrees.ConclusionEpisodic vertigo and dizziness are the main clinical symptoms of vestibular paroxysmia,MRI mostly showed interactive oppression of vestibulocochlear nerve and blood vessel,BAEP examination mostly showed latency of Ⅰ to Ⅲ inter-peak;the misdiagnosis rate is relatively higher,the causes of misdiagnosis includes insufficient understanding of clinicians,patient-provide inaccurate medical history,nonspecific clinical symptoms and laboratory examination methods.
Vestibular paroxysmia;Vertigo;Diagnostic errors
242000安徽省宣城市人民医院神经内科
R 764.34
B
10.3969/j.issn.1008-5971.2016.02.032
2015-12-05;
2016-02-03)
