外侧直切口入路治疗肩胛骨骨折的疗效和操作细节
2016-06-27张川王蕾张作君赵明李星星蔡鸿敏
张川 王蕾 张作君 赵明 李星星 蔡鸿敏
·论著·
外侧直切口入路治疗肩胛骨骨折的疗效和操作细节
张川1王蕾2张作君1赵明1李星星1蔡鸿敏1
目的 探讨外侧直切口入路治疗肩胛骨骨折的疗效,分析该切口入路在操作中的细节处理。方法 自2010年5月至2015年2月河南省骨科医院收治的46例(47肩)以肩胛颈、盂和体部骨折为主的肩胛骨骨折患者,进行了外侧直切口入路手术治疗并获得6个月以上随访。手术采用外侧直切口入路,保留三角肌后束的完整性,通过松解三角肌和周围肌肉之间的筋膜使其具有一定牵拉活动度,在适度屈伸收展肩关节和提拉三角肌后束下,自冈下肌和小圆肌的间隙进行分离,显露肩胛颈、肩胛盂后侧、肩胛骨外侧,对骨折进行复位和固定。术后分别进行临床和影像学随访,随访6个月时采用Hardegger评分和Constant-Murley评分评定肩关节功能。结果 47肩均获得骨性愈合。3例患者围手术期出现并发症,并发肺感染2例,1例伴同侧胫腓骨开放性骨折患者并发尿路感染,以上经治疗感染均得到控制。1例术后出现异位骨化。依据Hardegger肩关节功能评定标准,结果优40肩,良6肩,可1肩。Constant-Murley评分平均(90.6±6.9)分,90~100分37肩,80~89分8肩,70~79分2肩。结论 外侧直切口具有软组织剥离少,利于早期康复的优点,用于肩胛骨骨折可以取得良好疗效。
外侧直切口入路;肩胛骨;骨折;内固定
肩胛骨骨折在肩胛带骨折中所占的比例仅3%~5%,在全身所有骨折中的占比也不足1%[1],多由高能量损伤导致,常有多发肋骨骨折、血气胸和脑外伤等损伤。在重视血气胸和脑外伤等危及生命损伤的同时肩胛骨骨折的诊断和治疗容易被忽视[2]。肩胛骨关节内骨折和关节外骨折的治疗原则差异很大,早期几乎所有的肩胛骨骨折均采用保守治疗,只有关节内骨折才考虑手术治疗,随着技术进步以及手术入路的改进,肩胛骨骨折手术治疗逐渐被接受。自2010年5月至2015年2月本院采取手术治疗肩胛骨骨折或合并肩胛骨骨折的病例278例,其中大部分病例采用Judet切口、改良Judet切口或外侧直行和内侧直行联合切口,单独采用肩胛骨外侧直行切口患者87例,有46例(47肩)患者具有较完整资料并取得良好疗效,现报道如下。
资 料 与 方 法
一、一般资料
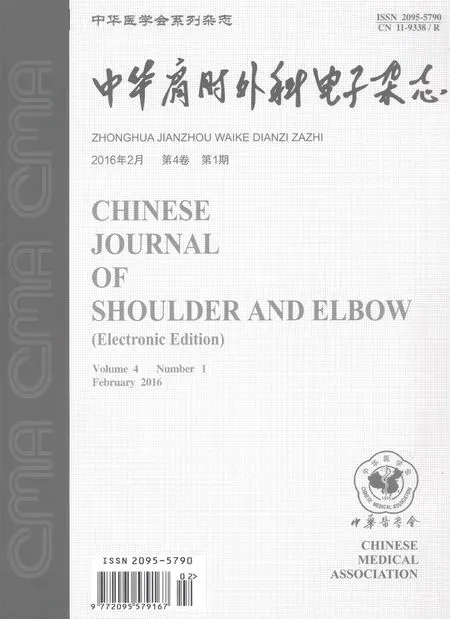
自2010年5月至2015年2月河南省骨科医院采用外侧直切口切开复位内固定治疗有完整资料的肩胛骨患者46例(47肩,1例为双肩胛骨骨折),其中男34例,女12例;年龄22~65岁,平均(44.9±12.16)岁。致伤原因:高处坠落伤12例,车祸交通伤13例,一般摔倒致伤14例,重物砸伤5例,机器绞扎上肢扭转致伤1例,击打致伤1例。合并损伤:1例双侧肩胛骨骨折(均为关节外骨折)合并多发肋骨骨折气血胸(图1),其余45例为单侧肩胛骨骨折;单纯肩胛骨骨折8例;其余病例中合并肋骨骨折18例,其中16例为多发肋骨骨折,2例单根肋骨骨折,其中伴有肺挫伤11例,合并气血胸12例;合并脑外伤或闭合性颅脑损伤8例,其中2例患者伤后昏迷3 d,3例患者有一过性昏迷;合并胸腰椎压缩性骨折3例,均无脊髓或马尾神经损伤,其中1例腰2-4横突骨折;合并锁骨骨折即浮肩损伤8例(其中7例为一般摔伤导致);合并同侧肩锁关节脱位1例,合并同侧肩袖撕裂1例,合并同侧胸锁关节前侧半脱位1例,合并同侧肱骨骨折并肩峰骨折导致肩锁关节横向分离1例,合并同侧肱骨近端骨折后脱位1例,合并尺骨骨折1例,合并同侧肩关节脱位、经尺骨鹰嘴肘关节骨折前脱位、股骨内髁并内踝骨折1例;合并同侧胫腓骨开放性骨折1例;无合并神经损伤病例。骨折按Hardegger等[3]提出的分型:其中肩胛体骨折31例(包括双肩病例的左肩),其中1例合并喙突基底部骨折,23例表现为骨折线沿肩胛冈向内侧不规则延伸;1例肩胛颈合并肩胛体骨折(双肩病例的右肩);肩胛外科颈骨折8例,其中2例合并肩峰骨折;肩胛解剖颈骨折2例,其中1例合并盂后缘骨折;肩胛盂窝骨折5例,1例合并肩胛体骨折(图2)。受伤至肩胛骨骨折手术时间4~22 d,平均(7.9±6.34)d,部分病例合并损伤为分期处理。
二、手术方法
全身麻醉或臂丛神经损伤阻滞后采用侧卧位,患侧上肢无菌包覆后放置于体侧或前屈放置于托手架上以利于肩关节自由屈伸收展,同时也利于整个肩胛带的良好显露和无菌准备,同时行锁骨骨折和肋骨骨折切开复位内固定时适当扩大无菌准备区域。
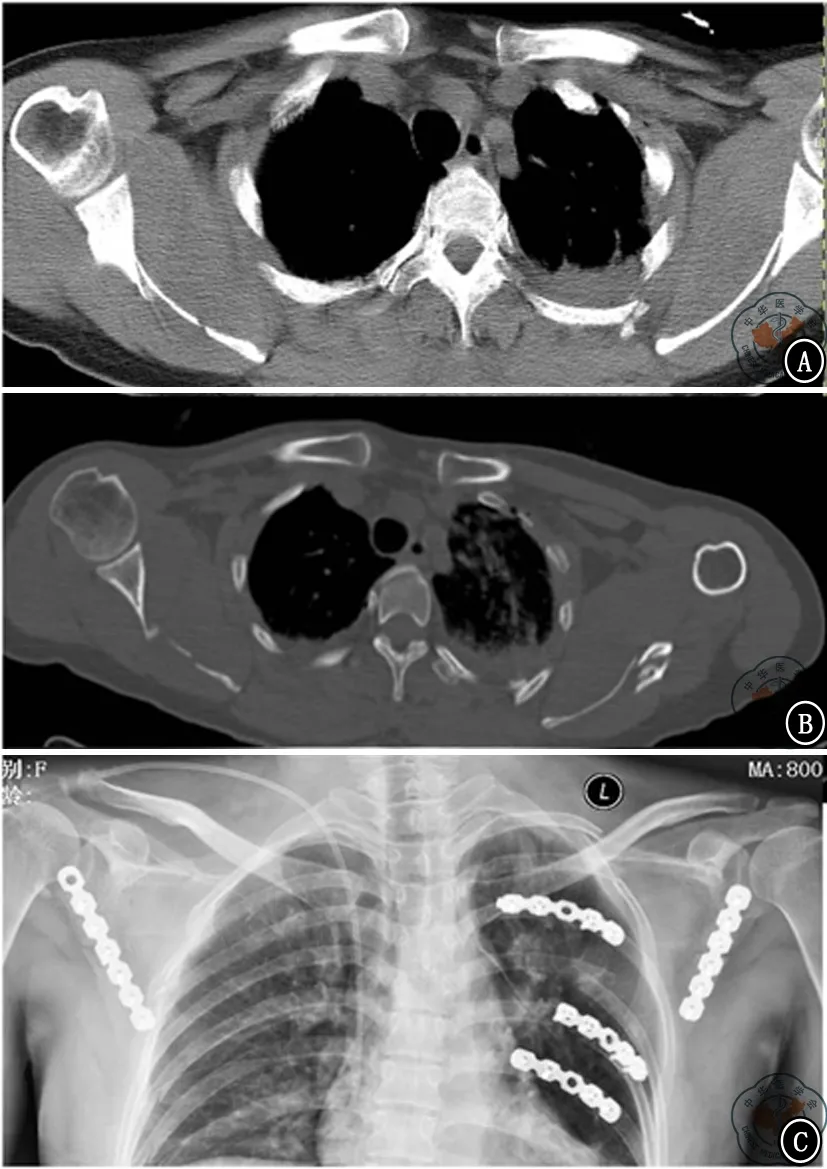
图1 双肩胛骨骨折并发多发肋骨骨折 图A、B为双侧肩胛骨CT扫描;图C为两侧均采用外侧直切口入路切开复位内固定治疗,肋骨骨折另行切口治疗
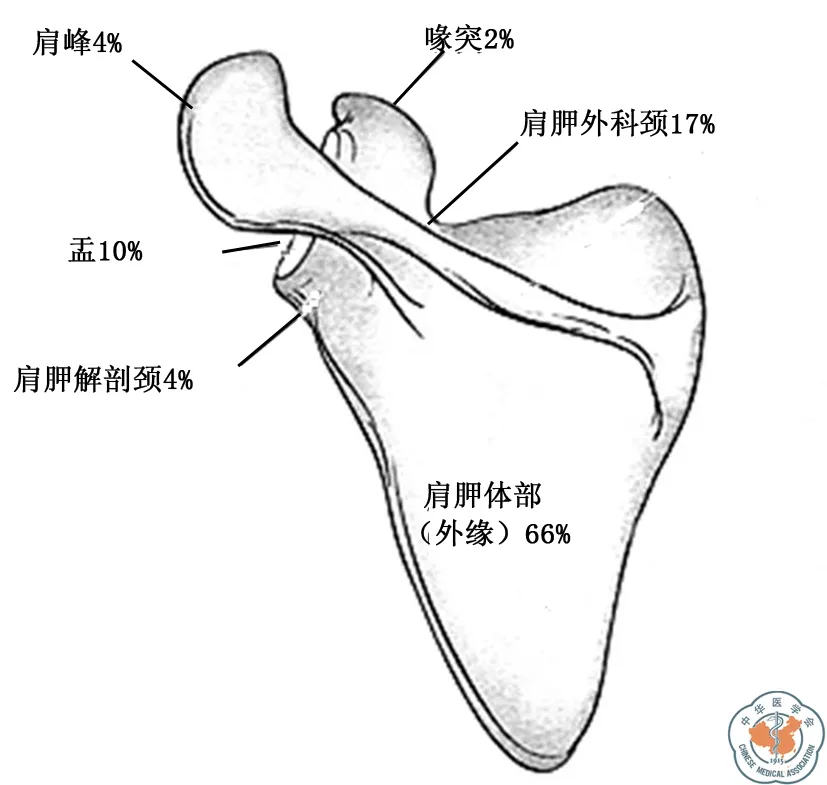
图2 本组病例肩胛骨骨折Hardegger分型分布情况
采用沿肩胛骨外下缘的直行切口,上起自肩峰后外侧角内下各一指即肩关节镜常规后侧软点入路部位,向肩胛骨下角延伸,骨折部位偏于近端盂下时切口向上延伸到肩峰,骨折偏下时切口向下延伸达到肩胛骨下角,合并肩峰骨折时切口向肩峰延伸。显露三角肌和冈下肌、小圆肌交叉点,适度游离此交叉点周围深筋膜以及各个肌肉之间的联结,使此部位各个肌肉相互间具有一定活动度以利于骨折端的显露,前屈外展患肢并用拉钩提拉三角肌后束,良好显露冈下肌和小圆肌,确定羽状冈下肌和束状小圆肌之间间隙后分离此间隙,部分病例在骨折过程中旋肩胛动静脉已经断裂并回缩,可以在手术过程出现相应部位出血时进行电凝止血或缝扎止血,旋肩胛动静脉完整病例应予以显露并结扎止血,显露肩胛盂后部时行骨膜下剥离以保护肩胛上神经。在肩胛骨外缘偏内侧1 cm部位用3.5 mm钻头或斯氏针打孔作为大号弯钳的把持点,钳夹断端两侧临时复位,斜行或横断型骨折可尝试用2.0 mm克氏针贯穿断端临时固定后再用重建钢板、T型钢板或跟骨钢板固定,断端外缘具有粉碎小骨片的病例可以先复位临时固定小骨片于一侧再行整体复位固定,小骨片难以临时固定病例可尝试复位并预留骨片空间以保持肩胛骨外缘长度,钢板固定外缘后再将小骨片填塞固定于折端,肩胛盂下半骨折可将盂复位后自盂后下向前上打入固定螺钉。钢板需向盂后缘放置时重建钢板的近端行侧向折弯并扭转使其贴服盂后缘,T型钢板和跟骨钢板适度扭转,螺钉打入方向平行于关节盂面,行真正的肩关节正位即肩胛盂侧位透视以确定螺钉未穿入肩关节。冲洗切口后彻底止血,对合缝合筋膜、皮下,切口放置引流管。

图3 左侧肩胛骨骨折病例,伴同侧胫腓骨开放性骨折,多发肋骨骨折并血胸,胸12、腰1椎体压缩性骨折,头皮撕裂伤 图A肩胛骨骨折三维重建,肩胛体中间可见翻转骨折片;图B采用重建板和T型板固定;图C为术后3周患者即可无痛下主动上举患肩;图D、E为双侧上举可见患侧肩胛骨活动度良好,并稍大于健侧肩胛骨活动度
三、术后处理及康复
术后根据引流量决定引流管留置时间,术前0.5 h预防性应用抗生素,术后继续应用48 h,有并发损伤患者根据情况延长抗生素应用时间。术后早期应用悬吊带制动患肢并鼓励患者进行无痛下患肩非负重功能锻炼,具体包括钟摆样运动,卧位健肢辅助下被动前屈,4周后开始卧位健肢辅助下被动上举、外展、外旋,部分患者可适度提前主动活动(图3);6周后开始站位健肢辅助上举、外展、外旋,并逐渐减小辅助力度,使患肢活动转变为主动负重下前屈上举、外旋和内旋;6~12周逐渐加大患肩负重力度和力量锻炼,术后12周完全恢复正常工作和生活;多发伤患者根据具体情况适度调整患肩锻炼的节点并与其他并发损伤的康复锻炼相结合。
四、术后随访和评价
术后即记录手术并发症情况,出院时叮嘱患者分别于术后1.5、2、6个月来院复查,行X线检查观察骨折愈合情况,并指导进一步加强功能锻炼。超过6个月以上随访时记录患者疼痛、肩关节活动度、肩关节肌力和日常生活能力情况。肩关节功能评定分别采用Hardegger肩关节功能评分[3]和肩关节功能综合评分系统Constant-Murley评分。
结 果
大多数患者未按照出院时的医嘱随访时间进行规范的术后复查随访,尤其是在术后2个月基本恢复正常工作和生活之后,即使经过电话或信件联系,其满足6个月以上随访病例的比例仅有55%,即46例患者末次随访在术后6个月以上,随访时间6~17.5个月,平均(8.3±7.1)个月。47肩均获得骨性愈合;3例患者围手术期出现并发症,并发肺感染2例,1例并发同侧胫腓骨开放性骨折患者出现尿路感染,以上经治疗感染均得到控制;1例术后出现异位骨化但无明显活动受限(图4);无患者出现切口血肿感染等问题;全部病例未发生骨折再移位、内固定装置断裂或者移位、内固定螺钉穿破肩胛盂关节面、神经损伤等并发症。
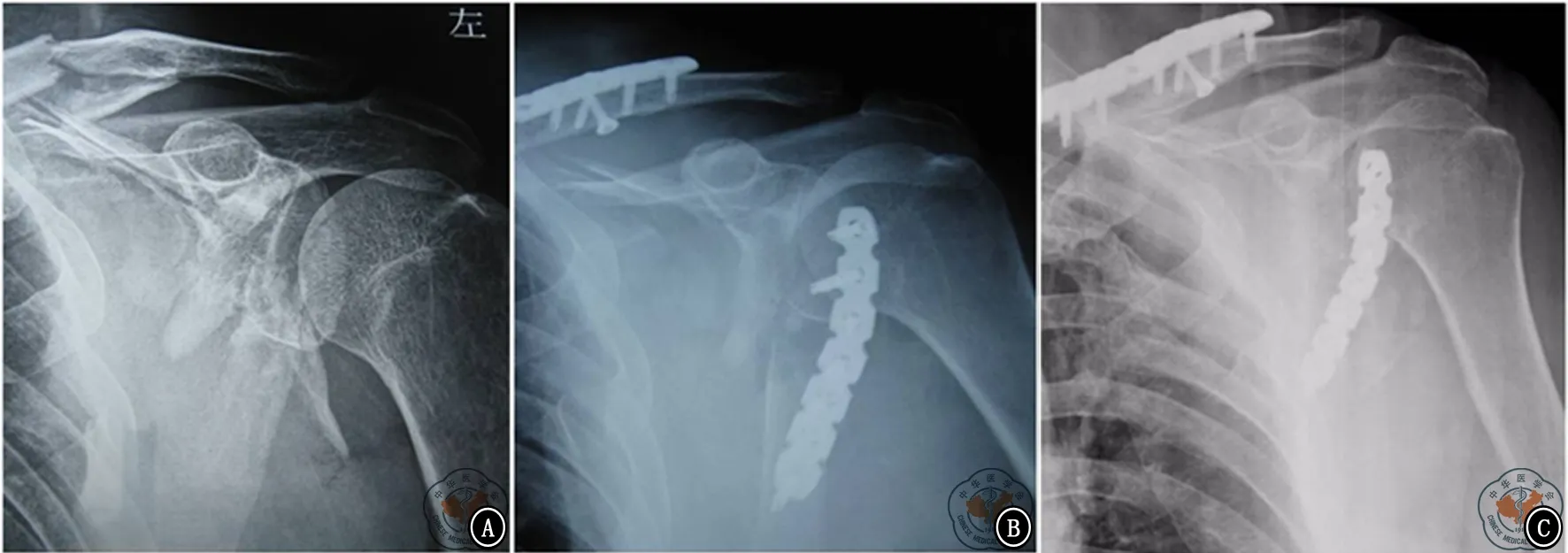
图4 典型浮肩损伤 图A平片;图B肩胛颈骨折并锁骨骨折同时固定术后;图C左侧术后9个月可见盂下异位骨化
依据Hardegger肩关节功能评定标准评价疗效:优,肩关节活动不受限,肩周无疼痛,外展肌力5级;良,肩关节活动略受限,肩周轻度疼痛,外展肌力4级;可,肩关节活动中度受限,肩周中度疼痛,外展肌力3级;差,肩关节活动严重受限,肩周严重疼痛,外展肌力2级。结果为优40例,良6例,可1例。依据肩关节Constant-Murley评分标准:90~100分为优有37例,80~89分为良有8例,70~79分为可有2例,平均(90.6±6.9)分。
讨 论
一、入路选择和肩胛盂颈部的显露
肩胛盂前侧、喙突以及包括盂上部在内的基底部适合于前侧入路,肩胛体和肩胛颈部骨折适合后侧入路[4]。后侧入路主要有早期的Judet入路,之后有改良的Judet入路和直切口入路,三种入路所需要的体位相同,差别在于切口位置和入路间隙。Judet入路和其改良入路均需要做弧形切口掀起皮瓣,将三角肌后束自肩胛冈剥离,其中Judet入路要将冈下肌自肩胛骨内侧缘和肩胛窝掀起以显露肩胛体,通过对皮瓣和肌瓣的牵拉肩胛骨外缘、肩胛颈部和肩胛盂可以得到良好显露[5],改良Judet入路利用冈下肌和小圆肌之间的间隙显露外缘和颈部, 二者在显露中均有牵拉损伤肩胛上神经的风险,对于后束的剥离必定影响术后早期的肩关节外展力量,掀起较大的皮瓣影响早期的康复同时切口也远大于直切口[6],Gauger等[7]采用内外侧双直切口入路切开复位内固定治疗肩胛骨骨折,并将此切口和传统Judet入路进行了对比,在切口大小方面双直切口(14.8 cm)明显优于Judet入路(29.2 cm),王勇等[6]在肩胛骨骨折手术治疗中采用外侧单切口入路,和Judet入路相比,切口长度方面优势明显6.73 cm对比18.88 cm,可见单独外侧切口相对于Judet入路的外观优势更加明显。对于骨折范围较广、需广泛显露的病例,可采用Judet入路或改良Judet入路,这些病例包括肩胛冈合并肩胛骨外缘和肩胛颈骨折、肩胛颈和肩胛骨外缘骨折,单纯外侧固定无法稳定肩胛颈者[8]。对于肩胛骨外侧、肩胛颈和盂后、下方错位的病例选择外侧直切口入路,切口跨越三角肌后束,三角肌后部可适当切断术后再缝合[6],选择在不剥离三角肌起点的情况下可以松解筋膜,使各个肌肉间具有活动度,通过患肩适度外展和三角肌的提拉同样可以显露肩胛颈和肩胛盂后部。本组在切口选择时即已排除了需要广泛显露的病例,因此本组病例的疗效评分和其他切口入路病例之间的可比性较低,这体现了本文的局限性。
二、旋肩胛血管的处理
肩胛骨发生骨折不愈合几率很低,因为肩胛骨血供丰富而且有大量肌肉附着和覆盖,其中最主要的血管包括旋肩胛动脉,旋肩胛动脉及其伴行静脉的出现恒定,93.3%起始于肩胛下动脉[9],深支多在肩胛盂下4 cm左右和伴行静脉绕肩胛骨外侧向内上和肩胛上动静脉相交通[10],跨肩胛骨部位多在骨折线上下,并且血管走行紧贴骨面,因此在肩胛骨骨折外缘固定中难以规避并保护旋肩胛动静脉,部分病例在骨折时可能旋肩胛动静脉即已经撕裂,此时血管撕裂断端回缩,但在操作过程中多会在相应部位出现残端出血,可单独予以缝扎或电凝止血,另有部分旋肩胛动静脉完整病例可在分离时清晰显露,应予以切断结扎。旋肩胛动静脉是外缘固定中必然要处理的知名动静脉,是否止血完善既影响术中出血量也涉及术后继发血肿的形成,笔者均在术前计划和术中预留旋肩胛动静脉处理时间。
三、固定方式的选择
肩胛骨形状不规则,其骨折复位方式与长管状骨有很大不同,单独外侧切口显露空间有限,所以点式钳等复位工具难以置入,操作时可以在外缘内侧打孔作为复位钳的把持着力点[8],而肩胛盂部位可以打入Schanz针进行把持复位。肩胛骨中间菲薄,周缘是较坚强的皮质骨,因此多选择边缘尤其是皮质骨丰厚的外缘进行固定,固定方式包括重建钢板、管型钢板或者联合微型钢板固定等多种。肩胛盂向前上延伸为喙突,在肩胛骨固定中,自盂下向喙突方向置钉即喙突螺钉可以取得较大的螺钉把持力,尤其适合于关节盂下半骨折的固定[11],但喙突螺钉的置入方向需要对切口进行外侧显露或者自腋窝后下经皮置入,存在损伤腋神经风险,而关节外的盂下骨折多需要联合钢板固定,应用喙突螺钉时需要将钢板放置于肩胛骨外缘的外下缘[12],对小圆肌甚至肱三头肌长头腱进行部分剥离,我们多选择将内固定放置于外缘后侧以最大程度减少对附着软组织的剥离,上部螺钉置入方向平行于或偏离肩胛盂。肩关节真正正位下的透视是确定螺钉是否穿入关节面的关键,此步骤也是手术操作中必须进行的。部分病例骨折线向内下延伸,肩胛体中间部位有较大骨折片形成成角错位甚至反转,而跟骨钢板有多个侧向固定支,在固定肩胛骨外缘的同时可以固定错位较多的中间骨片,也可以附加钢板固定中间骨片。骨折部位邻近关节盂下病例,常规应用重建钢板固定肩胛盂需要进行侧向折弯,但盂后侧上下长度有限,一般仅能够固定2枚螺钉,笔者于部分病例选用了桡骨远端骨折使用的T型钢板,目的是不必侧向折弯而能够在盂后尽可能多枚螺钉固定,加强内固定的牢固度。肩胛骨骨折病例多有并发损伤,本组病例中有并发伤的比例高达82.6%(38/46),仅有8例病例为单发肩胛骨骨折,在手术中多数并发损伤如并发尺骨骨折、肩关节骨折后脱位等需要一并处理,因此其手术时间、术中出血量和术后引流量等多个数据虽然在病例原始资料中有记录,但病例间差别较大,笔者认为在本研究中无明确对比价值。
综上所述,虽然本研究属回顾性研究,具有明显局限性,但从本组病例的结果可以看出,肩胛盂后下、颈部和外缘骨折可以采用外侧直切口获得良好显露和满足早期功能锻炼的稳固固定,关键是显露细节的处理。
[1] Cole PA,Freeman G,Dubin JR.Scapula fractures[J].Curr Rev Musculoskelet Med,2013,6(1):79-87.
[2] Romero J,Schai P,Imhoff AB.Scapular neck fracture--the influence of permanent malalignment of the glenoid neck on clinical outcome[J].Arch Orthop Trauma Surg,2001,121(6):313-316.
[3] Hardegger FH, Simpson LA, Weber BG. The operative treatment of scapular frature[J]. J Bone Joint Surg Br, 1984, 66(11): 725-731.
[4] Lantry JM,Roberts CS,Giannoudis PV.Operative treatment of scapular fractures:a systematic review[J].Injury,2008,39(3):271-283.
[5] 付中国,张堃.Judet入路治疗肩胛骨骨折[J/CD].中华肩肘外科电子杂志,2014,2(1):63-68.
[6] 王勇,许兵,吴银生,等.直切口与Judet入路治疗肩胛骨颈部及体部骨折的对比研究[J].中华骨科杂志,2013,33(10):1018-1023.
[7] Gauger EM,Cole PA.Surgical technique:a minimally invasive approach to scapula neck and body fractures[J].Clin Orthop Relat Res,2011,469(12):3390-3399.
[8] 赵良瑜,陈爱民,李永川.经改良 Judet 入路手术治疗肩胛骨骨折的疗效[J/CD].中华肩肘外科电子杂志,2015,3(1) :30-34.
[9] 王金平,赵玉玲,王岱君,等.旋肩胛动脉双叶皮瓣修复手足皮肤软组织缺损的解剖学研究[J].解剖与临床,2007,12(4):240-242.
[10] Wijdicks CA,Armitage BM,Anavian J,et al.Vulnerable neurovasculature with a posterior approach to the scapula[J].Clin Orthop Relat Res,2009,467(8):2011-2017.
[11] Nork SE,Barei DP,Gardner MJ,et al.Surgical exposure and fixation of displaced type IV,V,and VI glenoid fractures[J].J Orthop Trauma,2008,22(7):487-493.
[12] Jones CB, Sietsema DL. Analysis of operative versus nonoperative treatment of displaced scapular fractures[J]. Clin Orthop Relat Res, 2011, 469(12): 3379-3389.
(本文编辑:李静)
张川,王蕾,张作君,等.外侧直切口入路治疗肩胛骨骨折的疗效和操作细节[J/CD]. 中华肩肘外科电子杂志,2016,4(1):48-53.
Evaluationoflateralstraightincisionapproachinthetreatmentofscapulafracturesandinvestigationofoperationaldetails
ZhangChuan1,WangLei2,ZhangZuojun1,ZhaoMing1,LiXingxing1,CaiHongmin1.
1DepartmentofUpperLimbInjury,OrthopedicHospitalofHenanProvince,Luoyang471002,China;2DepartmentofOrthopedics,theAffiliatedRuijinHospital,ShanghaiJiaotongUniversitySchoolofMedicine,Shanghai200025,China
Correspondingauthor:ZhangZuojun,Email:zc360006@163.com
Background The approach of choice for open reduction internal fixation of displaced scapular fractures involving the scapula neck or body is from posterior including modified Judet approach, the lateral straight incision approach and so on. The chosen surgical approach depends on fracture location, complexity, and chronicity. Less invasive approaches are preferred when feasible, but are technically more demanding. There is an unstudied belief that patients rehabilitate faster and have less pain with less invasive dissection. In this study, lateral straight incision approach was evaluated as the treatment of some subgroup of scapular fractures.Methods 278 cases of scapular fractures were treated operatively in our hospital from 2005 to 2015, most of the cases were operated through Judet or modified Judet approach. Eighty-seven cases underwent lateral straight incision approach, 46 cases (47 scapulas) of them were followed up for more than 6 months from May 2010 to February 2015. The age of the 34 males and 12 females ranged from 22 to 65 years old with an average age of 44.9. The causes of injury included fell from height in 12 cases, automobile accident in 13 cases, crashed injury in 5 cases, fell from standing height in 14 cases, torsional injury of arm in 1 case, beated by other guy in 1 case. There were 8 solo scapular fractures, 1 bilateral scapular fracture with associate injuries of pneumohemothorax and multiple rib fractures, all the other 35 patients had associate injuries, including 8 cases of craniocerebral injury, 16 cases of multiple rib fracture and 2 solo rib fracture, 11 cases of contusion of lung and pleural effusion, 12 cases of pneumohemothorax, 3 cases of spine fractures with no spinal cord injury, 8 cases of craniocerebral injury,8 cases of ipsilateral clavicular fracture, 1 case respectively with the injury of posterior fracture-dislocation of proximal humerus, cervical cord injury, ipsilateral ulnar fracture, disassociation of acromioclavicular joint caused by acromion fracture, ipsilateral shoulder dislocation, anterior trans-olecranon fracture dislocation, malleolus fracture, open fracture of tibia and fibula. There were 31 scapular body fractures, 8 scapular surgical neck fractures, 2 scapular anatomic neck fractures, 5 glenoid fossa fractures, 1 scapular neck combined with body fracture according to Hardegger scapular fracture classification. The time interval between injury and operation was 4-22 days, averaged in 7.9 days. Operation method: The patients were placed on lateral decubitus position under general anesthesia, entire forequarter was carefully prepped and draped in the usual sterile fashion with the arm free, associated injured site was also prepped if it need to be addressed. Lateral straight incision approach was performed, the incision started from the soft point of 1cm medial inferior to the posterolateral corner of acromion in the dorsal side of scapula, extending toward the inferior angle of scapula, it could be extended superiorly or inferiorly along with the need for exposure. The fascia around deltoid and adjacent muscles were released to improve the movement between each other, the location and tension of posterior bundle of deltoid could also be changed with the ad-abduction or flexion and extension to facilitate exposure by retractors. Interval between infraspinatus and teres minor was opened to expose the lateral rim, scapula neck and dorsal glenoid. Circumflex scapular artery was routinely ligated for the expansion of exposure and placement of implants. The fracture was reduced with reduction clamps and provisionally fixed with K-wires, plates were contoured as the dorsal facet of lateral scapular rim and dorsal glenoid, the screws were inserted parallel or even deviated to the glenoid surface and this should be confirmed by fluoroscopy to avoid joint penetration. The wound was closed in layers after hemostasis and irrigation. Postoperative treatments: Painless pendulum movement and assisted movement in lying position was proceeded in the first 4 weeks, then the movement was started in standing position, active movement was started after 6 weeks and the patients recuperated 12 weeks later. Patients were asked to return to the hospital for follow-up and instructions for functional rehabilitation. Hardegger scoring system and Constant-Murley score were used for functional evaluation.Results Most of the patients could not regularly return to hospital for follow-up, only 46 patients were followed for more than 6 months, the mean time is 8.3±7.1(6-17.5) months. Complications such as infection occurred in 3 patients and heterotopic ossification occurred in 1 patient. No nonunion, nerve injury occurred. According to Hardegger shoulder score, the results were excellent in 40 cases,good in 6 cases, moderate in 1 case. According to Constant-Murley score, the mean score was 90.6±6.9(71-100)points, there were 37 cases in the range 90 to 100 points, 8 cases in the range 80 to 89 points and 2 cases in the range 70 to 79 points.Conclusion The lateral straight incision approach is indicated for lateral rim, scapular neck and posterior glenoid fractures with the advantages of less soft tissue dissection and early good recovery, anatomic reduction and rigid fixation, especially favorable exposure can be achieved with this approach.
Lateral straight incision approach;Scapula;Fracture;Internal fixation
10.3877/cma.j.issn.2095-5790.2016.01.009
2013年河南省中医药科学研究专项课题(2013ZY04003)
471002洛阳,河南省骨科医院上肢损伤科1;200025上海交通大学医学院附属瑞金医院骨科2
张作君,Email:zc360006@163.com
2015-09-21)