PPI联合瑞巴派特促进内镜黏膜下剥离术术后溃疡愈合的疗效分析
2016-06-05张少君董小林
张少君,董小林
湖北医药学院附属人民医院体检中心,湖北 十堰 442000
PPI联合瑞巴派特促进内镜黏膜下剥离术术后溃疡愈合的疗效分析
张少君,董小林
湖北医药学院附属人民医院体检中心,湖北 十堰 442000
目的 系统评价质子泵抑制剂(proton pump inhibitors, PPI)联合瑞巴派特治疗内镜黏膜下剥离术(endoscopic submucosal dissection, ESD)术后溃疡的有效性和安全性。方法 计算机检索PubMed、Web of Science、Medline、Embase、Cochrane Central Register of Controlled Trials、CENTRAL、CJFD、CBM、CNKI、VIP及WanFang Data,检索时间截至2015年8月1日,查找所有比较PPI联合瑞巴派特预防ESD术后溃疡出血作用的随机对照试验(RCTs)。由2名评价者按照纳入和排除标准独立选择文献、提取资料、评价质量,采用RevMan 5.2和Stata 12.0软件进行Meta分析。结果 共纳入6项RCTs,共724例患者。合并结果显示:与单用PPI相比,应用PPI联合瑞巴派特后溃疡愈合率明显升高(OR=2.40, 95%CI: 1.68~3.44);根据疗程长短(4周和8周)进行亚组分析显示:联合用药组溃疡愈合率均高于单用PPI组(4周:OR=2.22, 95%CI: 1.53~3.24;8周:OR=3.19, 95%CI: 1.22~8.31)。对于直径>2 cm溃疡,联合用药组疗效更明显(OR=4.77, 95%CI: 2.22~10.26)。而对于溃疡部位、是否合并H.pylori感染,两者疗效无明显差异。用药过程中两组均无明显不良反应。结论 PPI联合瑞巴派特疗效优于单用PPI,尤其对于直径>2 cm的溃疡。受纳入研究数量和质量限制,需要开展更多高质量、大样本、多中心的RCTs进一步论证其安全性。
内镜黏膜下剥离术;瑞巴派特;质子泵抑制剂;Meta分析
目前,内镜黏膜下剥离术(endoscopic submucosal dissection,ESD)是广泛应用于胃腺瘤和早期胃癌的微创治疗,具有创伤小、愈合快的特点。与传统的内镜黏膜下切除术(endoscopic mucosal resection,EMR)相比,ESD 更适用于直径大(>2 cm)、形状扁平的胃癌,且其肿瘤完全切除率远高于EMR,但其所引起的医源性溃疡也更大更深,且ESD术后出现延迟出血和穿孔风险增加,因此,尽快促进ESD术后溃疡面的愈合可有效预防出血和穿孔的并发症[1]。质子泵抑制剂(proton pump inhibitor, PPI)是治疗ESD术后溃疡最有效的药物,然而有报道[2]称单用PPI 4周治疗ESD术后溃疡是不充分的。瑞巴派特是一种胃黏膜保护剂,广泛应用于亚洲国家[3]。许多临床试验[4-5]发现瑞巴派特可加快溃疡的愈合。目前已有大量研究[6-12]报道了PPI联合瑞巴派特治疗ESD术后溃疡的有效性和安全性,然而在药物选择、治疗时间及最佳治疗方案等方面仍未达成一致意见。我们运用循证医学的原理和方法,对比PPI联合瑞巴派特和单用PPI治疗ESD术后溃疡愈合作用的随机对照试验(randomized controlled trials,RCTs)进行系统评价,为临床决策提供最佳证据。
1 资料与方法
1.1 纳入及排除标准
1.1.1 纳入标准:(1)比较PPI联合瑞巴派特和单用PPI治疗ESD术后溃疡愈合的研究;(2)RCTs;(3)干预措施:试验组采用PPI联合瑞巴派特,对照组采用PPI;(4)结局指标:ESD术后溃疡愈合率。
1.1.2 排除标准:(1)缺失重要研究数据的文献;(2)重复发表且病例数较少的文献;(3)有摘要而无全文,且联系作者索取未果。
1.2 文献检索计算机检索PubMed、Web of Science、Medline、Embase、Cochrane Central Register of Controlled Trials、CENTRAL、CJFD、CBM、CNKI、VIP及WanFang Data,检索时间均为建库至2015年8月1日。文种限中、英文。英文检索endoscopic submucosal dissection or ESD、proton pump inhibitor or PPI、Rebamipide;中文检索内镜黏膜下剥离术(ESD)、质子泵抑制剂(PPI)、瑞巴派特,同时辅以文献追溯。
1.3 资料提取由2名研究者独立进行文献筛选并提取资料,意见不一致时通过讨论解决或由第三名研究者协助解决。资料提取内容包括:作者、发表年份、国家、年龄、性别、试验组和对照组样本量、干预措施、疗程、肿瘤部位、大小、H.pylori感染状态及结局指标(达到S期认为溃疡愈合)。
1.4 文献质量评价由2名研究者根据Jadad量表[13]对纳入研究的方法学质量进行评估,具体内容包括随机序列产生、盲法、分配隐藏、退出/失访。分数范围为1~5分,得分>3分提示文献质量较高。
1.5 统计学分析统计分析采用Cochrane协作网的RevMan 5.2软件进行。合并效应量选用比值比(OR)及其95%CI。对纳入研究进行异质性检验(采用Q检验和I2统计量)[14],如P>0.1或I2<50%提示各研究间无异质性,采用固定效应模型进行合并分析[15],反之则采用随机效应模型[16]。敏感性分析为依次排除单个文献后重新进行Meta分析,估计综合效应大小。发表偏倚分析应用Stata 12.0软件通过Begg秩相关法[17]、Egger回归法[18]进行量化检测(P<0.05认为存在发表偏倚)。
2 结果
2.1 文献检索结果根据检索策略,初检出310篇文献,经初步筛查,7篇文献[6-12]初步纳入分析,其中1篇文献[12]缺少可提取数据被排除,最终纳入6个RCTs[6-11],包括724例患者。纳入研究的一般情况如表1所示,其中5项研究来自日本,1项研究来自韩国。Jadad评分结果显示均>3分,提示纳入文献的研究质量较好。

表1 纳入文献的基本情况
续表1
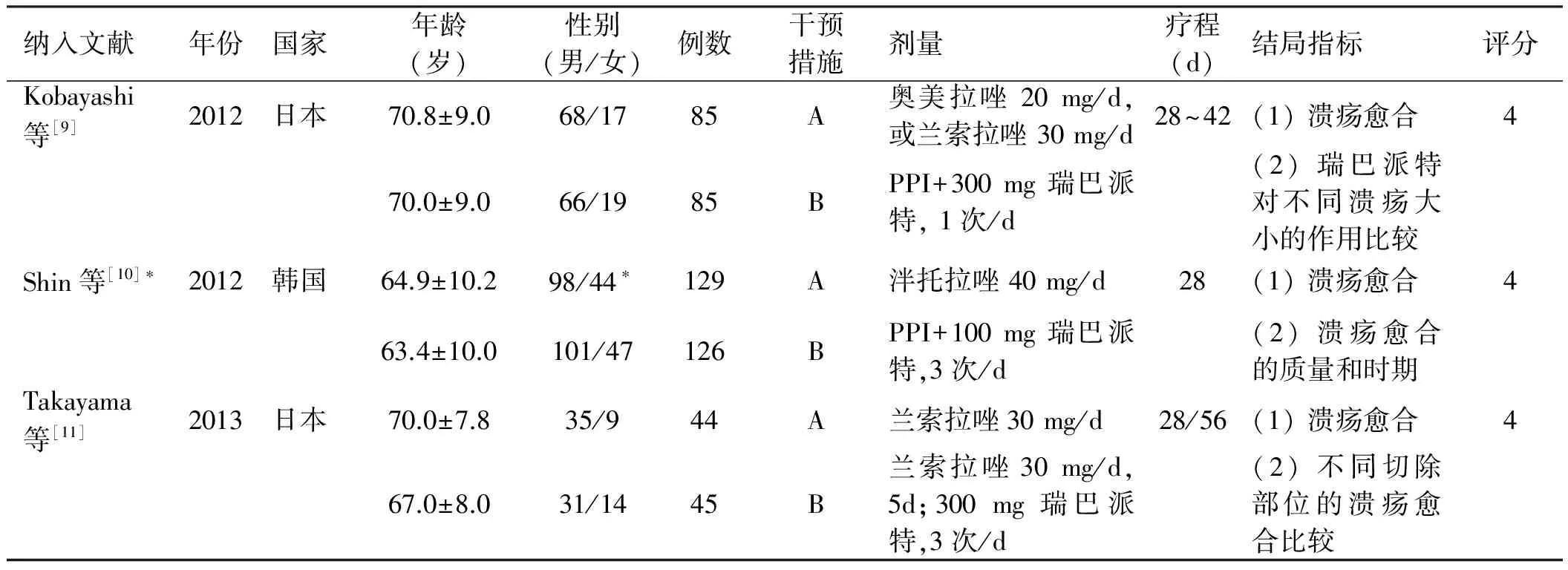
纳入文献年份国家年龄(岁)性别(男/女)例数干预措施剂量疗程(d)结局指标评分Kobayashi等[9]2012日本70.8±9.068/1785A奥美拉唑20mg/d,或兰索拉唑30mg/d28~42(1)溃疡愈合470.0±9.066/1985BPPI+300mg瑞巴派特,1次/d(2)瑞巴派特对不同溃疡大小的作用比较Shin等[10]∗2012韩国64.9±10.298/44∗129A泮托拉唑40mg/d28(1)溃疡愈合463.4±10.0101/47126BPPI+100mg瑞巴派特,3次/d(2)溃疡愈合的质量和时期Takayama等[11]2013日本70.0±7.835/944A兰索拉唑30mg/d28/56(1)溃疡愈合467.0±8.031/1445B兰索拉唑30mg/d,5d;300mg瑞巴派特,3次/d(2)不同切除部位的溃疡愈合比较
注:A:PPI;B:PPI+瑞巴派特。*指A、B两组入选例数分别为142和148,但最终符合条件的例数分别为129和126。
2.2 Meta分析结果
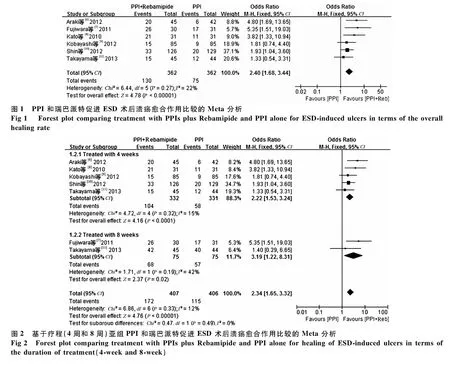
2.2.1 溃疡愈合率:6个研究[6-11]均报道了PPI 与瑞巴派特促进ESD术后溃疡愈合的作用,其中PPI 组和PPI联合瑞巴派特组均为362例。各研究结果间无统计学异质性(I2=22%,P=0.27),故采用固定效应模型进行Meta分析。结果显示,PPI联合瑞巴派特组促进溃疡愈合的作用优于单用PPI组(OR=2.40, 95%CI: 1.68~3.44)(见图1);根据疗程进行亚组分析显示,无论用药4周还是8周,PPI联合瑞巴派特组均优于单用PPI组(4周:OR=2.22, 95%CI: 1.53~3.24;8周:OR=3.19, 95%CI: 1.22~8.31)(见图2)。
有2项研究分别报道了切除部位[7,11]和H.pylori感染状态[10-11]的数据,结果显示在溃疡愈合率方面,两组之间无明显差异;另外,有2项研究[6,8]报道了溃疡大小的数据,结果显示,无论是直径为2~4 cm还是>4 cm的溃疡,PPI联合瑞巴派特组均优于单用PPI组(2~4 cm:OR=3.58, 95%CI: 1.51~8.52;>4 cm:OR=12.66, 95%CI: 2.04~78.70)(见图3)。
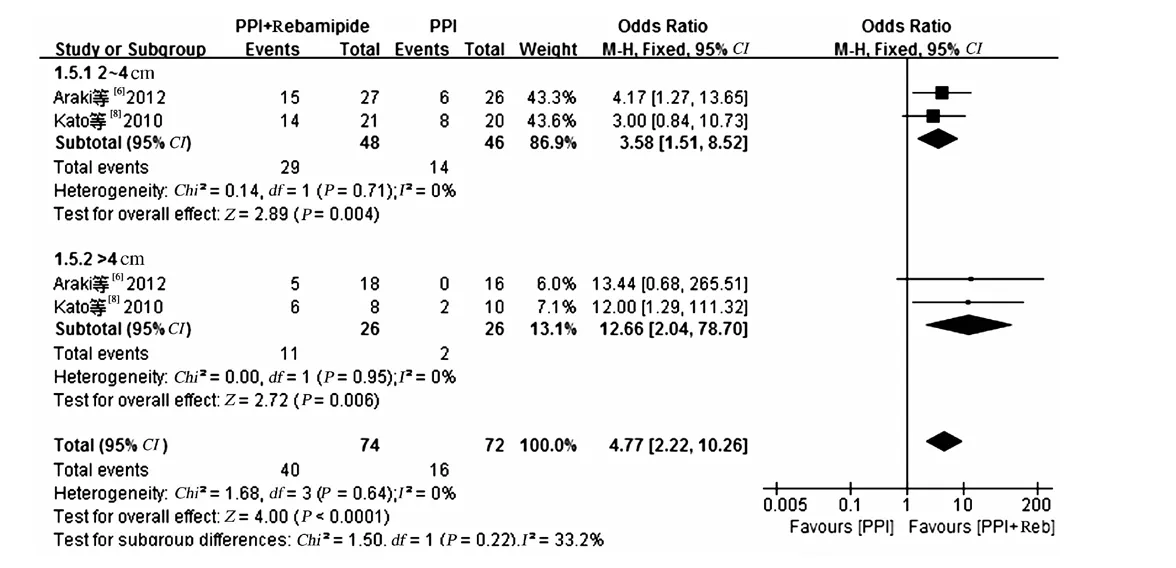
图3 基于溃疡大小PPI 和瑞巴派特促进ESD 术后溃疡愈合作用比较的Meta 分析
2.2.2 不良反应:3项研究[7-8,11]报道了不良反应情况,仅有1项研究[7]中单用PPI组出现了术后出血。
2.3 敏感性和发表偏倚分析依次单独剔除1篇文献后,合并效应量无明显改变。Begg漏斗图结果显示未见发表偏倚(见图4)。Egger回归法量化检测也未见发表偏倚(P=0.143)。
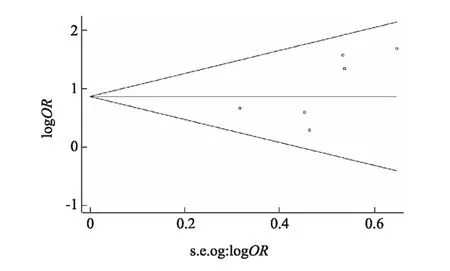
图4 Begg漏斗图分析
3 讨论
本文共纳入6项RCTs,包括724例患者。合并结果显示,与单用PPI相比,应用PPI联合瑞巴派特后溃疡愈合率明显升高;根据疗程长短(4周和8周)进行亚组分析同样显示:联合用药组溃疡愈合率均高于单用PPI组。此外,对于直径>2 cm溃疡,联合用药组疗效更明显。而对于不同部位的溃疡,两者疗效无明显差异。虽然H.pylori感染是消化性溃疡的病因之一,有研究[19]显示H.pylori感染状态对ESD术后溃疡愈合无明显影响。本文有2篇文献报道了H.pylori感染的情况,合并分析结果提示两者疗效无明显差异。然而由于纳入文献较少,结论需进一步验证。另外,我们也对两组中不良反应情况进行分析,发现用药过程中两组均无明显不良反应。
虽然PPI是ESD术后治疗溃疡和出血的标准药物,Fujiwara等[7]报道称在胃酸分泌水平较低的患者(如胃黏膜严重萎缩)中,单独给予PPI和胃酸抑制剂作用有限,在这种患者中,单纯的抑制胃酸对于溃疡愈合已不是主要因素。另外,不同个体间对PPI药物的反应性也可影响药物的疗效,如PPI代谢与细胞色素P450 2C19酶有关,该酶基因型差异可能会影响机体对PPI药物的反应性。因此,与其他药物合用是必须的。瑞巴派特是一种新型的黏膜保护剂,兼有增强防御因子和炎症抑制两方面作用。Terano等[4]进行的一项研究显示与安慰剂相比,H.pylori根除治疗后,给予7周瑞巴派特治疗可促进胃溃疡的愈合。其主要机制[20-25]可能为;(1)抑制中性粒细胞引发的自由基损伤;(2)剂量依赖性地清除氧自由基;(3)减少炎症因子的产生;(4)升高表皮生长因子(epidermal growth factor, EGF)及其受体的表达;(5)激活环氧化酶-2 的基因表达;(6)促进胃黏膜PG 合成;(7)加强上皮屏障作用。
本Meta 分析也存在一定的局限性:(1)纳入文献较少,且文献质量参差不齐;(2)纳入文献均为正式发表的文献,不能完全排除发表偏倚的影响;(3)纳入文献中结局指标不完全一致,影响进一步的亚组分析等;(4)纳入文献中PPI选择存在差异,可能会对结果有所影响。
综上所述,PPI联合瑞巴派特治疗ESD术后溃疡疗效优于单用PPI,尤其对于直径>2 cm的溃疡。然而受纳入研究数量和质量限制,尚需要开展更多高质量、大样本、多中心的RCTs进一步论证其安全性。
[1]Yamamoto H. Endoscopic submucosal dissection-current success and future directions [J]. Nat Rev Gastroenterol Hepatol, 2012, 9(9): 519-529.
[2]Asakuma Y, Kudo M, Matsui S, et al. Comparison of an ecabet sodium and proton pump inhibitor (PPI) combination therapy with PPI alone in the treatment of endoscopic submucosal dissection (ESD)-induced ulcers in early gastric cancer: prospective randomized study [J]. Hepatogastroenterology, 2009, 56(94-95): 1270-1273.
[3]Naito Y, Yoshikawa T. Rebamipide: a gastrointestinal protective drug with pleiotropic activities [J]. Expert Rev Gastroenterol Hepatol, 2010, 4(3): 261-270.
[4]Terano A, Arakawa T, Sugiyama T, et al. Rebamipide, a gastro-protective and anti-inflammatory drug, promotes gastric ulcer healing following eradication therapy for Helicobactor pylori in Japanese population: a randomized, double-blind, placebo-controlled trial [J]. J Gastroenterol, 2007, 42(8): 690-693.
[5]Song KH, Lee YC, Fan DM, et al. Healing effects of rebamipide and omeprazole in Helicobacter pylori-positive gastric ulcer patients after eradication therapy: a randomized double-blind, multinational, multi-institutional comparative study [J]. Digestion, 2011, 84(3): 221-229.
[6]Araki H, Kato T, Onogi F, et al. Combination of proton pump inhibitor and rebamipide, a free radical scavenger, promotes artificial ulcer healing after endoscopic submucosal dissection with dissection size >40 mm [J]. J Clin Biochem Nutr, 2012, 51(3): 185-188.
[7]Fujiwara S, Morita Y, Toyonaga T, et al. A randomized controlled trial of rebamipide plus rabeprazole for the healing of artificial ulcers after endoscopic submucosal dissection [J]. J Gastroenterol, 2011, 46(5): 595-602.
[8]Kato T, Araki H, Onogi F, et al. Clinical trial: rebamipide promotes gastric ulcer healing by proton pump inhibitor after endoscopic submucosal dissection-a randomized controlled study [J]. J Gastroenterol, 2010, 45(3): 285-290.
[9]Kobayashi M, Takeuchi M, Hashimoto S, et al. Contributing factors to gastric ulcer healing after endoscopic submucosal dissection including the promoting effect of rebamipide [J]. Dig Dis Sci, 2012, 57(1): 119-126.
[10]Shin WG, Kim SJ, Choi MH, et al. Can rebamipide and proton pump inhibitor combination therapy promote the healing of endoscopic submucosal dissection-induced ulcers? A randomized, prospective, multicenter study [J]. Gastrointest Endosc, 2012, 75(4): 739-747.
[11]Takayama M, Matsui S, Kawasaki M, et al. Efficacy of treatment with rebamipide for endoscopic submucosal dissection-induced ulcers [J]. World J Gastroenterol, 2013, 19(34): 5706-5712.
[12]Bunno M, Gouda K, Yamahara K, et al. A case-control study of esomeprazole plus rebamipide vs. omeprazole plus rebamipide on post-ESD gastric ulcers [J]. Jpn Clin Med, 2013, 4: 7-13.
[13]Jadad AR, Moore RA, Carroll D, et al. Assessing the quality of reports of randomized clinical trials: is blinding necessary? [J]. Control Clin Trials, 1996, 17(1): 1-12.
[14]Lau J, Ioannidis JP, Schmid CH. Quantitative synthesis in systematic reviews [J]. Ann Intern Med, 1997, 127(9): 820-826.
[15]Mantel N, Haenszel W. Statistical aspects of the analysis of data from retrospective studies of disease [J]. J Natl Cancer Inst, 1959, 22(4): 719-748.
[16]DerSimonian R, Laird N. Meta-analysis in clinical trials [J]. Control Clin Trials, 1986, 7(3): 177-188.
[17]Begg CB, Mazumdar M. Operating characteristics of a rank correlation test for publication bias [J]. Biometrics, 1994, 50(4): 1088-1101.
[18]Egger M, Davey Smith G, Schneider M, et al. Bias in meta-analysis detected by a simple, graphical test [J]. BMJ, 1997, 315(7109): 629-634.
[19]Kakushima N, Fujishiro M, Yahagi N, et al. Helicobacter pylori status and the extent of gastric atrophy do not affect ulcer healing after endoscopic submucosal dissection [J]. J Gastroenterol Hepatol, 2006, 21(10): 1586-1589.
[20]Kleine A, Kluge S, Peskar BM. Stimulation of prostaglandin biosynthesis mediates gastroprotective effect of rebamipide in rats [J]. Dig Dis Sci, 1993, 38(8): 1441-1449.
[21]Tarnawski A, Arakawa T, Kobayashi K. Rebamipide treatment activates epidermal growth factor and its receptor expression in normal and ulcerated gastric mucosa in rats: one mechanism for its ulcer healing action? [J]. Dig Dis Sci, 1998, 43(9 Suppl): 90S-98S.
[22]Takaishi O, Arakawa T, Yamasaki K, et al. Protective effect of rebamipide against ammonia-induced gastric mucosal lesions [J]. Dig Dis Sci, 1998, 43(9 Suppl): 78S-82S.
[23]Naito Y, Yoshikawa T, Tanigawa T, et al. Hydroxyl radical scavenging by rebamipide and related compounds: electron paramagnetic resonance study [J]. Free Radic Biol Med, 1995, 18(1): 117-123.
[24]Tarnawski AS, Chai J, Pai R, et al. Rebamipide activates genes encoding angiogenic growth factors and Cox2 and stimulates angiogenesis: a key to its ulcer healing action? [J]. Dig Dis Sci, 2004, 49(2): 202-209.
[25]Qi Z, Jie L, Haixia C, et al. Effect of rebamipide on quality of peptic ulcer healing in rat [J]. Dig Dis Sci, 2009, 54(9): 1876-1883.
(责任编辑:李 健)
The efficacy and safety of PPI plus Rebamipide for endoscopic submucosal dissection-induced ulcers: a Meta-analysis
ZHANG Shaojun, DONG Xiaolin
Medical Examination Center, Renmin Hospital Affiliated to Hubei University of Medicine, Shiyan 442000, China
Objective To compare the efficacy and safety of proton pump inhibitors (PPI) plus Rebamipide and PPI alone for the healing of ulcer after endoscopic submucosal dissection (ESD). Methods PubMed, Web of Science, Medline, Embase, Cochrane Central Register of Controlled Trials, CENTRAL, CJFD, CBM, CNKI, VIP and WanFang Data were researched up to the end of Aug. 2015 to identify all randomized controlled trials (RCTs) that reported the effect of PPI plus Rebamipide for the healing of ulcer after ESD. Outcome measures were ulcer healing. Results Six studies involving 724 patients were included. Pooled data suggested a significantly higher ulcer healing rate after endoscopic therapies in PPI plus Rebamipide group than that in the PPI alone group (OR=2.40, 95%CI: 1.68-3.44). Subgroup analysis showed PPI plus Rebamipide was more effective in the healing of ESD-induced ulcer than PPI in both 4-week (OR=2.22, 95%CI: 1.53-3.24) and 8-week duration of medication (OR=3.19, 95%CI: 1.22-8.31). The combination therapy was significantly more effective than the PPI alone for every size of ESD ulcer larger than 2 cm (OR=4.77, 95%CI: 2.22-10.26). There was no significantly difference in ulcer location (low, middle, or upper stomach) andH.pyloriinfection or not between combination therapy and PPI alone groups. No serious adverse events occurred in the two groups. Conclusion PPI plus Rebamipide is superior to PPI alone for the healing of ulcer after ESD, especially for large-sized ulcers. However, more well-designed trials are needed to confirm the findings.
Endoscopic submucosal dissection; Rebamipide; Proton pump inhibitor; Meta-analysis
10.3969/j.issn.1006-5709.2016.06.024
张少君,主治医师,研究方向:胆胰疾病的诊断。E-mail: zhangshaojunsy@163.com
董小林,主治医师,研究方向:胆胰疾病和消化道肿瘤的防治。E-mail: dongxlmail@163.com
R57
A
1006-5709(2016)06-0686-05
2015-09-06