Pattern and prognostic factor of ocular injuries in southwest Ethiopia: a hospital based prospective study
2016-05-17SisayBekeleYeshigetaGelaw
Sisay Bekele, Yeshigeta Gelaw
Department of Ophthalmology,College of Health Sciences, Jimma University, Jimma, Ethiopia
Correspondence to:Yeshigeta Gelaw. Department of Ophthalmology, College of Health Science, Jimma University, P.O.Box: 440, Jimma, Ethiopia. dryeshi@yahoo.com
Received: 2014-12-28 Accepted: 2016-03-10
埃塞俄比亚西南地区眼外伤类型和预后因素的回顾性研究
Sisay Bekele, Yeshigeta Gelaw
(作者单位:埃塞俄比亚,季马,季马大学健康研究学院,眼科)
Pattern and prognostic factor of ocular injuries in southwest Ethiopia: a hospital based prospective study
Sisay Bekele, Yeshigeta Gelaw
Department of Ophthalmology,College of Health Sciences, Jimma University, Jimma, Ethiopia
Correspondence to:Yeshigeta Gelaw. Department of Ophthalmology, College of Health Science, Jimma University, P.O.Box: 440, Jimma, Ethiopia. dryeshi@yahoo.com
Received: 2014-12-28Accepted: 2016-03-10
埃塞俄比亚西南地区眼外伤类型和预后因素的回顾性研究
Sisay Bekele, Yeshigeta Gelaw
(作者单位:埃塞俄比亚,季马,季马大学健康研究学院,眼科)
Abstract
•AIM: To determine the pattern, severity, and prognostic factors of ocular injuries in the southwest Ethiopia.
•METHODS:A prospective hospital based study was done on all patients presented with ocular injury to Jimma University Specialized Hospital from Apr. to Sep. 2009. Each patient underwent a detailed interview and a standard comprehensive ocular examination. Data were analyzed using SPSS version 13 andP< 0.05 was considered significant.
•RESULTS:The overall prevalence of ocular injury was 3.03%. Nearly 99% of ocular injuries were mechanical. The majority of the ocular injuries (53.2%) were work-related and none of these patients had eye protection at the time of injury. Out of 170 globe injuries, 57.6 % were closed globe injury and 42.4% were open globe injuries. Closed globe injuries were less severe and had significantly better visual outcome than open globe injuries (P<0.05). The final visual outcome was also significantly associated with presenting visual acuity and time from diagnosis to surgical treatment (P<0.05). Eye injuries were responsible for monocular blindness in 59 (34.3%) patients. Late presentation, poor presenting visual acuity, open globe injury and presence of complications were the risk factors identified for poor final visual acuity outcome.
•CONCLUSION: Most ocular injuries occurred in the workplace,and a significantly larger proportion of patients with ocular injury developed monocular blindness. For the prevention of serious injuries, eye health education and safety strategies should be applied both at home and work place.
KEYWORDS:•ocular injuries; monocular blindness; globe injuries; risk factors
Citation:Bekele S, Gelaw Y. Pattern and prognostic factor of ocular injuries in southwest Ethiopia: a hospital based prospective study.GuojiYankeZazhi(IntEyeSci) 2016;16(5):811-817
INTRODUCTION
Ocular trauma, once described as the ‘neglected disorder’, has recently been highlighted as a major cause of visual morbidity[1]. World-wide, approximately 1.6 million people are blind and 2.3 million are bilaterally visually impaired from eye injuries; and an additional 19 million with unilateral visual loss; making ocular trauma the commonest cause of unilateral blindness today[1].
Male gender, lower socioeconomic status, younger age and occupation are some of the known risk factors associated with ocular trauma[2-4]. Moreover, the pattern of ocular injuries is influenced by several factors: the environment, socioeconomy, life style and policies like economy (whether mainly agricultural or industrial lead), enforcement of seat belts and availability of eye safety measures at work[2, 4].
Besides its impact on affected individuals, there are profound social implications of ocular trauma such as loss of productivity particularly of young men[5]. The overall financial costs can only be an estimate but direct and indirect costs taken together are known to run into hundreds of millions of dollars annually. The socioeconomic impact of eye injuries is tremendous in developing countries and yet these countries are the least able to afford the costs[5].
Ethiopia is one of the countries with the highest prevalence of blindness (1.6%) and low vision (3.7%) in the world[6]. The estimated cost for medical care and vocational rehabilitation is, thus, expected to be high. This makes preventive measures more effective despite progress in the treatment of eye injuries to improve the outcome. However, prevention can only be effective when the epidemiology of ocular trauma is known. This study was conducted to determine the prevalence of ocular trauma and its determinants at Jimma University Specialized Hospital, a referral center for southwest Ethiopia. It aimed to provide health and safety strategies in the prevention of serious ocular injuries for the maintenance of eye health and design a standardized ophthalmic medical and surgical care.
SUBJECTS AND METHODS
A prospective hospital based study was conducted at Jimma University Specialized Hospital from Apr. to Sep. 2009. Since the hospital is the only referral center in the southwest Ethiopia, patients either presented directly to the hospital or referred from other health institutions in the region; and all these patients who came with a complaint of ocular trauma were enrolled in the study.
All consenting patients were interviewed using a structured questionnaire by the principal investigators and then underwent a comprehensive ocular examination including Snellen’s visual acuity test , pupillary light reaction ( using penlight), ocular motility assessment (when indicated), intraocular pressure (IOP) measurement (when indicated), slit lamp biomicroscopy and indirect ophthalmoscopy. Patients were followed after the initial evaluation and discharge from the hospital. The average follow up time for final visual acuity testing was 4.2mo (ranging from 1-6mo). Patients’ chart, of those who did not come on date of follow up,was also reviewed later to document the post treatment final visual acuity.
Tetracaine (1%) eye drop was used to anesthetize the eye with closed eye injuries and similarly tropicamide (1%) eye drop was used to dilate the pupil for fundus examination.
We used the Ocular Trauma Classification Group (OTCG)’s recommendation[7]to classify mechanical eye injuries; and the Birmingham Eye Trauma Terminology system (BETT)[8]to classify the type of closed globe injuries (contusion and lamellar laceration) or open globe injuries (rupture, penetration,intraocular foreign bodies and perforation). The zones of injury for open globe injuries were categorized as zone I for injuries limited to the cornea, zone Ⅱ for injuries within 5 mm from the limbus and zone Ⅲ for injuries beyond 5 mm from the limbus.
Table 1Socio-demographic characteristics of the study population

PatientcharacteristicsNumberPercentAge 1-103419.9 11-205029.2 21-303621.1 31-402212.9 41-501911.1 >50105.8 Total171100Sex M12170.8 F5029.2 Total171100Ethnicity Oromo7946.2 Keffa3017.5 Amhara2112.3 Dawuro1810.5 Bench74.1 Yem42.3 Others127.0 Total171100Religion Christian8549.7 Muslim7644.4 Others105.8 Total171100Occupation Farmer6940.4 Justachildorstudent5733.3 Worksinoffice179.9 Daylaborer95.3 Machinetechnician84.7 Merchant74.1 Driver31.8 Others10.6 Total171100
Data were analyzed using SPSS version 13 software (SPSS Inc., USA). Theχ2-test was used to see the association andP<0.05 was considered significant. Other statistical tests like the Studentt-test and logistic regression were also used to see associations and differences between variables.
The study was conducted following the guidelines of Helsinki declaration and it was approved by the Institutional Review Board (IRB) of Jimma University. Informed consent was taken and only those who consented were studied.
Table 2Final visual outcome in relation to duration of presentation
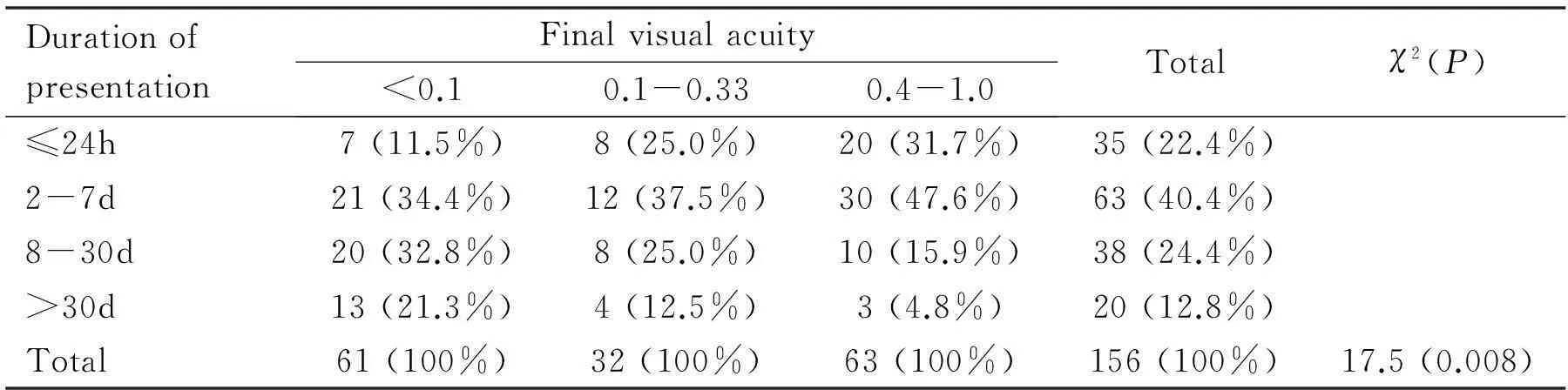
DurationofpresentationFinalvisualacuity<0.10.1-0.330.4-1.0Totalχ2(P)≤24h7(11.5%)8(25.0%)20(31.7%)35(22.4%)2-7d21(34.4%)12(37.5%)30(47.6%)63(40.4%)8-30d20(32.8%)8(25.0%)10(15.9%)38(24.4%)>30d13(21.3%)4(12.5%)3(4.8%)20(12.8%)Total61(100%)32(100%)63(100%)156(100%)17.5(0.008)
RESULTS
Socio-demographic and Clinical CharacteristicsOf the total 5642 patients seen during the study period, 171 (3.03%) had eye injury. The mean age of patients with eye injury was 25.3±15.8y. The majority of the patients were males (70.8%), farmers (40.4%) and in age group of 11-30y (50.3%) (Table 1).
The mean time of presentation after injury was 51.2±185.6d. Thirty five (22.4%) patients came within 24h of injury, 63 (40.4%) within 2-7d of injury and 38 (24.4%) within 8d to 1mo of injury and the rest after 1mo (Table 2). The majority of patients (53.5%) with globe injury had presenting visual acuity of <0.1. The remaining had presenting visual acuity of 0.4-1 (37.6%) and 0.1-0.33(8.8%). Six patients had a relative afferent papillary defect (RAPD). The time from injury to hospital arrival affected the presenting visual acuity significantly. Patients who presented early had better presenting visual acuity than those who presented late (P=0. 008). All, except one, patients with RAPD had presenting visual acuity of <0.1 but it was not statistically significant (P>0.05). Of 156 (91.2%) patients with final visual acuity, the majority (40.4%) had visual acuity of 0.4-1 and the remaining had visual acuity of <0.1 (39.1%) and 0.1-0.33 (20.5%). Patients who came early had better visual acuity outcome than those who came late (table 2); and there was a statistically significant association between time of presentation and final visual outcome (P<0.05).
Circumstances,Places and Sources of Eye InjuryMajority of the eye injuries (53.2%) were work-related. None of the patients with work-related eye injuries had eye protection at the time of injury. More than three quarter of patients sustained eye injury accidentally and non-domestic violence accounted for 19.9% of eye injuries and followed by domestic violence and child abuse (1.8%). About 5% of patients were drunk during the time of injury (Table 3).
Majority of eye injuries occurred at residential area (37.4%) and followed by at farming place (18.7%) (Table 3). More males sustained injuries in farm and on the street compared to females while more females sustained injuries at home and in the jungle compared to males (Table 4). There was a statistically significant association between sex and place of injury (P=0.004).
More than half (56.7%) of eye injuries were caused by blunt objects and about 20% were caused by sharp wooden material (Table 3). The highest frequency of eye injury occurred in Jun. during which 43 (25.1%) patients presented followed by Sep., 39(22.8%) and least occurred in Jul., 6 (3.5%)( Figure 1).
Table 3Circumstances, places and sources of eye injury
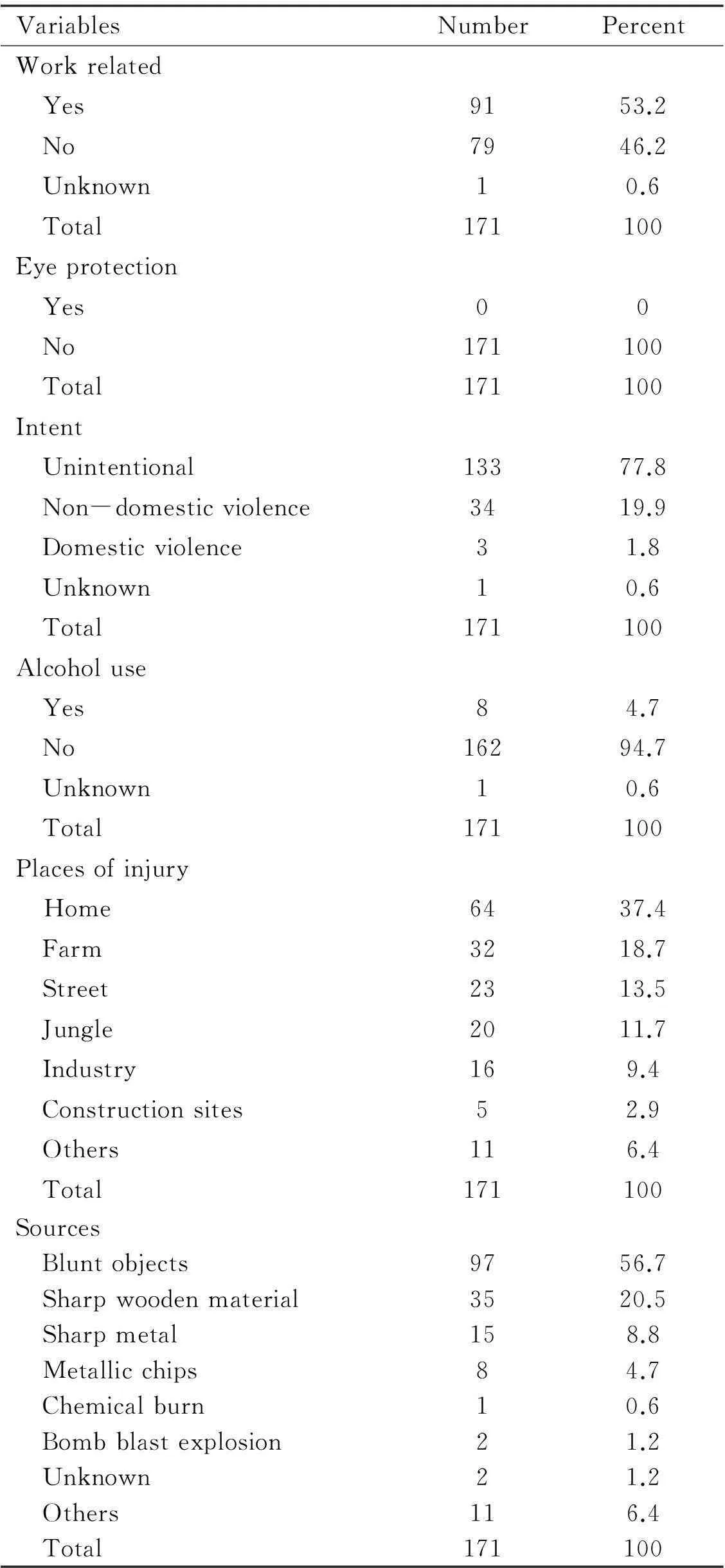
VariablesNumberPercentWorkrelated Yes9153.2 No7946.2 Unknown10.6 Total171100Eyeprotection Yes00 No171100 Total171100Intent Unintentional13377.8 Non-domesticviolence3419.9 Domesticviolence31.8 Unknown10.6 Total171100Alcoholuse Yes84.7 No16294.7 Unknown10.6 Total171100Placesofinjury Home6437.4 Farm3218.7 Street2313.5 Jungle2011.7 Industry169.4 Constructionsites52.9 Others116.4 Total171100Sources Bluntobjects9756.7 Sharpwoodenmaterial3520.5 Sharpmetal158.8 Metallicchips84.7 Chemicalburn10.6 Bombblastexplosion21.2 Unknown21.2 Others116.4 Total171100
Table 4Association between place of ocular injury and gender
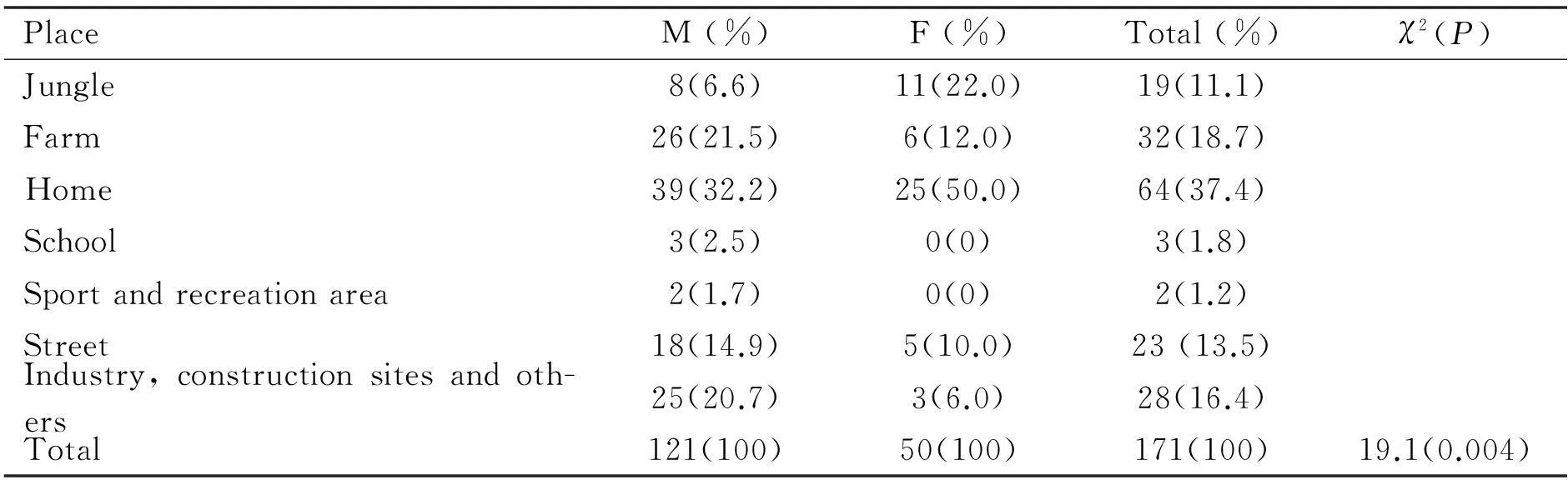
PlaceM(%)F(%)Total(%)χ2(P)Jungle8(6.6)11(22.0)19(11.1)Farm26(21.5)6(12.0)32(18.7)Home39(32.2)25(50.0)64(37.4)School3(2.5)0(0)3(1.8)Sportandrecreationarea2(1.7)0(0)2(1.2)Street18(14.9)5(10.0)23(13.5)Industry,constructionsitesandoth-ers25(20.7)3(6.0)28(16.4)Total121(100)50(100)171(100)19.1(0.004)
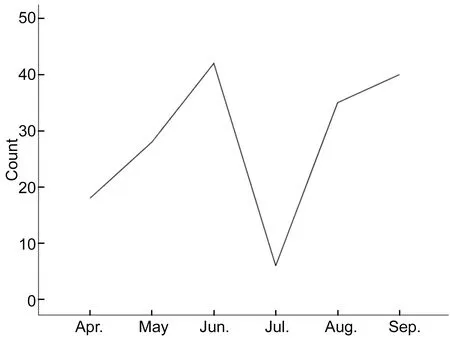
Figure 1Monthly distributions of ocular injuries.
Patterns and Complications of Ocular InjuryOf 171 patients, 170 (99.4%) had globe injury and 7 (4.1%) had associated particular injury and one patient had an isolated lid injury. Ninety-eight patients (57.6%) had closed globe injury while 72 (42.4%) had open globe injury. Of those with open globe injuries, 44 (60.1 %) had globe penetration and 28 (38.9%) had a globe rupture. Globe penetration occurred commonly on cornea (90.9%) and the rest occurred on sclera (9.1%). The most common site of globe rupture was cornea (64.2%) and scleral and corneoscleral ruptures accounted for 17.9% each. Among closed globe injuries, contusion was the commonest (68.4%) followed by corneal lamellar laceration (21.4%) and corneal foreign body (10.2%) (Table 5).
Patients with open globe injuries had worse presenting visual acuity and final visual outcome as compared to patients with closed globe injury and this was found to be statistically significant (P<0.05) (Table 6).
Forty one (24.1%) patients had an injury to the lens: 33 (80.5%) of them developed cataract and 8 (19.5%) of the patients had lens subluxation and dislocation.
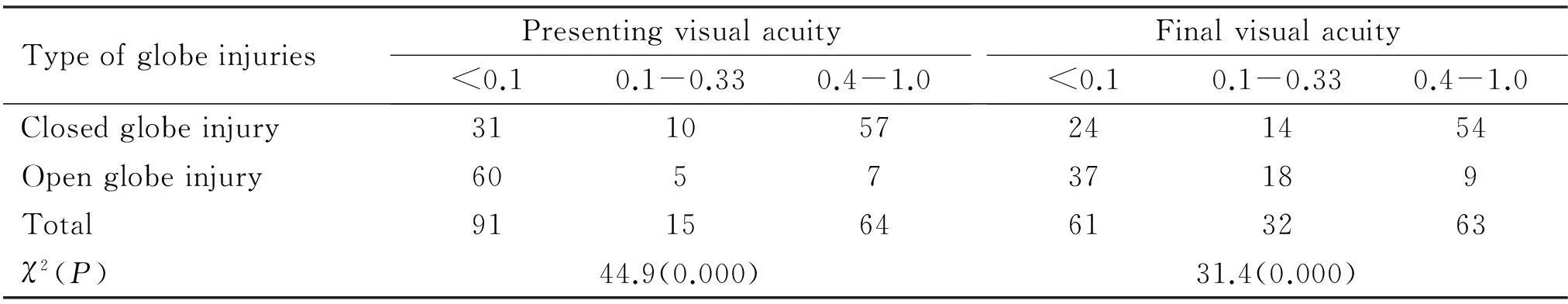
Vitreoretinal injuries were not uncommon. Of the total 170 patients presented with globe injury, 18 (10.6%) had vitreoretinal injury. The most common injury was commotio retina which was seen in 5 (2.9%) patients. Retinal detachment was seen in 4 (2.4%) patients (Table 7).
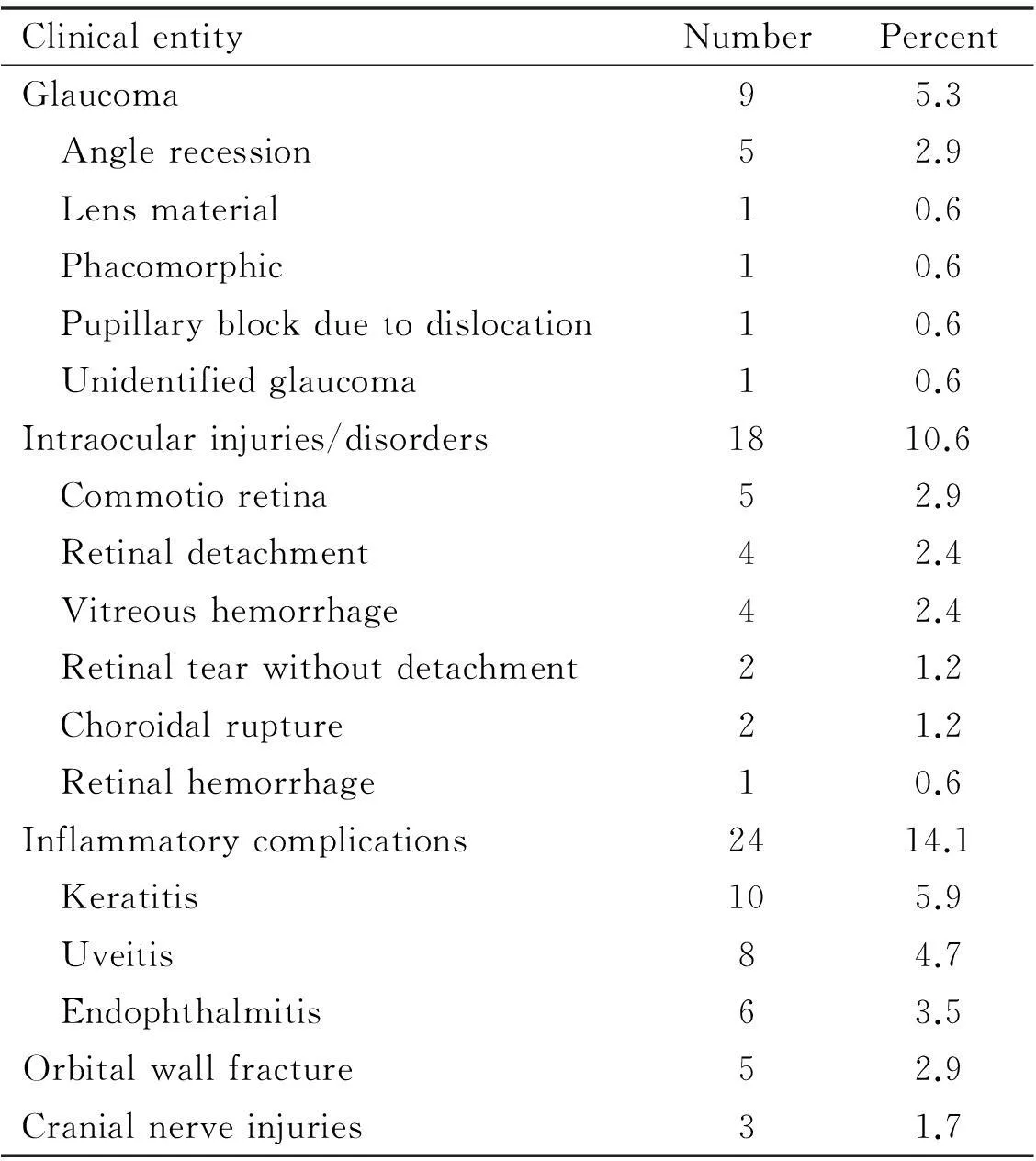
As shown in figure 2, of 70 open globe injuries with clearly identifiable zone of injury, 56 (80%) of them occurred in zone I, 10 (14%) of them in zone Ⅱ and the rest 4 (6%) in zone Ⅲ. Patients with zone I open globe injury had a worse final visual outcome compared to patients with other zones of injury but this difference was not statistically significant (P>0.05).
Table 5Type of globe injuries

TypesofglobeinjuryNumberPercentOpenglobeinjury7242.4 Globerupture2838.9 Cornealrupture1864.2 Scleralrupture517.9 Corneoscleralrupture517.9 Globepenetration4460.1 Cornealperforation4090.9 Scleralperforation49.1Closedglobeinjury9857.6 Contusion6768.4 Lamellarcorneallaceration2121.4 Cornealforeignbody1010.2
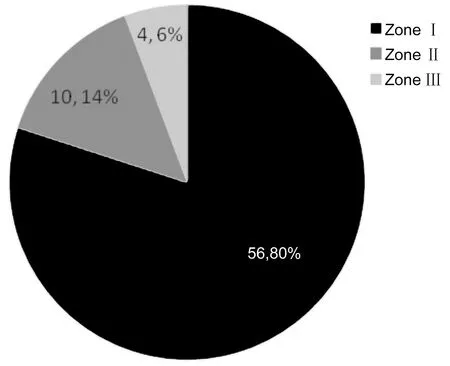
Figure 2Distribution of zones of injury among open globe injuries.
Of all patients presented with eye injury, 24 (14.1%) also had an infection and or inflammation, 5 (2.9%) orbital injury and 3 (1.7%) had cranial nerves injury. The most common complication was keratitis (5.9%) followed by uveitis (4.7%) and endophthalmitis (3.5%).
Regarding intraocular pressure, 9 (5.3%) had glaucoma and 4 (2.3%) had hypotony. The most frequent type of glaucoma was angle recession (2.9%) (Table 7).
Table 6Association of the type of globe injuries with presenting visual acuity and final visual acuity (n=166)
TypeofglobeinjuriesPresentingvisualacuity<0.10.1-0.330.4-1.0Finalvisualacuity<0.10.1-0.330.4-1.0Closedglobeinjury311057241454Openglobeinjury605737189Total911564613263χ2(P)44.9(0.000)31.4(0.000)
Table 7Complication of ocular injuries and other associated injuries
ClinicalentityNumberPercentGlaucoma95.3 Anglerecession52.9 Lensmaterial10.6 Phacomorphic10.6 Pupillaryblockduetodislocation10.6 Unidentifiedglaucoma10.6Intraocularinjuries/disorders1810.6 Commotioretina52.9 Retinaldetachment42.4 Vitreoushemorrhage42.4 Retinaltearwithoutdetachment21.2 Choroidalrupture21.2 Retinalhemorrhage10.6Inflammatorycomplications2414.1 Keratitis105.9 Uveitis84.7 Endophthalmitis63.5Orbitalwallfracture52.9Cranialnerveinjuries31.7
Therapeutic Measures for Ocular InjuryOut of 171 injured eyes, 107 (62.5%) needed only conservative treatment and 64 (37.5%) were surgically treated. The mean duration of surgery after evaluation at Eye Clinic was 2.88±3.67d and range 19d. The time interval from presentation to surgical intervention significantly affected the final visual outcome (Pearson’sr=-0.321,P=0.015) and those who were operated earlier had a better visual outcome than those operated later.
Blindness and Determinants of Final Visual Acuity OutcomeSixty one (34.3%) patients had monocular blindness (final visual acuity<0.1); of these 40 (67.8%) were male and 28 (47.1%) were 1-19y of age. Nearly two third of monocular blindness 37 (60.7%) was due to open globe injury and this was statistically significant (P<0.05).Twenty four patients had monocular blindness due to closed globe injuries and contusion (19, 70.4%) was the most frequent cause of monocular blindness.
A logistic regression analysis was made for variables which had significant association with final visual acuity outcome. Patients who came later than 3d after injury were 3.6 times more likely to have an impaired final visual acuity than patients who came earlier and this was found to be statistically significant (P<0.001;CI:1.9-6.9) and the odds of having impaired final visual acuity for those who presented later than three days was 2.8 when controlled for presenting visual acuity and types of injury which was also found to be significant (P<0.05;CI: 1.1-7.6). Patients with open globe injuries were 6.5 times more likely to have an impaired final visual acuity than patients with closed globe injury and this was statistically significant (P<0.001;CI: 3.1-13.8 ) but when controlled for duration and presenting visual acuity, the odds was 1.7 which was not statistically significant (P>0.05;CI: 0.6-4.7). Patients with the presenting visual acuity of <6/18 were 66.3 times more likely to have impaired visual acuity outcome than those with the presenting visual acuity of ≥6/18 which was statistically significant (P<0.001;CI: 22.6-194.3) and when controlled for the duration, type of injury and complication, the odds was 35.9 and it was still statistically significant (P<0.001;CI: 10.7-120.5). Patients who had complications were 9.3 times more likely to have impaired visual acuity than those without complication which was statistically significant (P<0.001;CI: 4.3-20.0) and it was 7.4 times when controlled for duration of presentation and type of injury (P<0.001;CI: 3.1-17.9) (Table 8).
DISCUSSION
Today, ocular injuries particularly work-related accidents are still frequent despite health education and other primary prevention efforts, and the eye is a high-risk organ for such an accident. Although it represents only 0.27% of the total body area and 4% of the facial area, ocular trauma is very frequent[9].
In this study, it was found that blunt objects were the commonest cause of eye injury. This is similar to other reports from Croatia[10]but different from study in Nigeria[11]where pointed objects and missiles were the most common cause of eye injury.
The most frequent type of eye injury found in the study was closed globe injury, and contusional type of closed globe injury was the most prevalent. This is similar to findings of other studies[10-11]. Studies done by Soliman and Macky[12]in Egypt and Caoetal[13]in China, however, found that open globe injuries were the major type accounting for 80.4% and 55.1% of all eye injuries respectively. There was a statistically significant difference between the type of globe injuries and final visual outcome whereby closed globe injuries had a better final visual outcome. This is a well documented fact reported by many studies[10-11,14-15].
Table 8Risk factors for impaired final visual acuity outcome
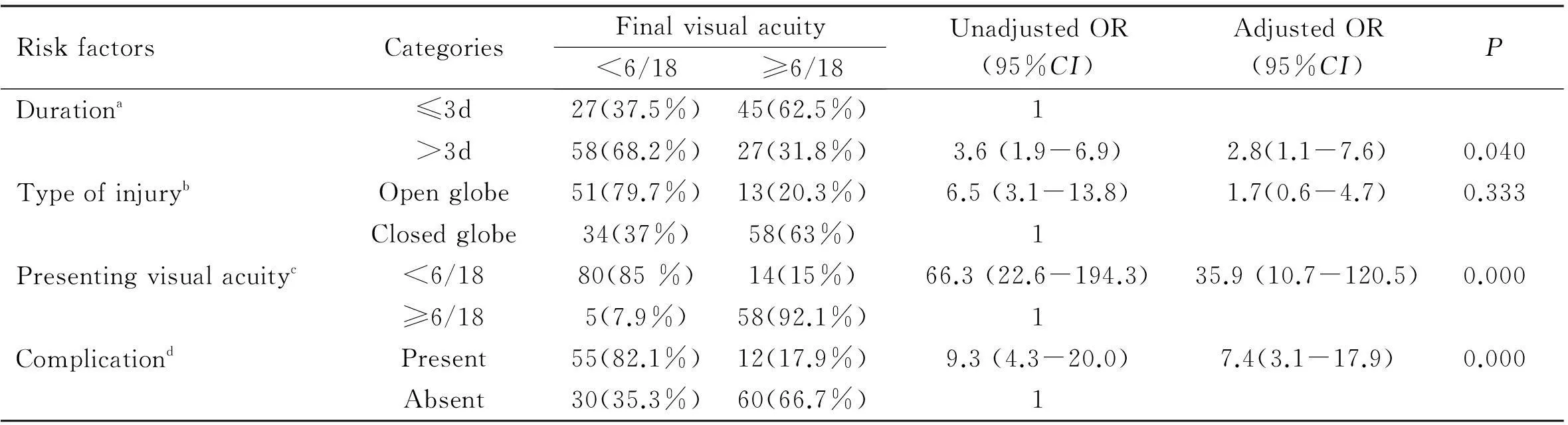
RiskfactorsCategoriesFinalvisualacuity<6/18≥6/18UnadjustedOR(95%CI)AdjustedOR(95%CI)PDurationa≤3d27(37.5%)45(62.5%)1>3d58(68.2%)27(31.8%)3.6(1.9-6.9)2.8(1.1-7.6)0.040TypeofinjurybOpenglobe51(79.7%)13(20.3%)6.5(3.1-13.8)1.7(0.6-4.7)0.333Closedglobe34(37%)58(63%)1Presentingvisualacuityc<6/1880(85%)14(15%)66.3(22.6-194.3)35.9(10.7-120.5)0.000≥6/185(7.9%)58(92.1%)1ComplicationdPresent55(82.1%)12(17.9%)9.3(4.3-20.0)7.4(3.1-17.9)0.000Absent30(35.3%)60(66.7%)1
aAdjusted for type of injury and presenting visual acuity;bAdjusted for duration and presenting visual acuity;cAdjusted for duration, type of injury, and complication;dAdjusted for duration and type of injury.
In published literatures it is documented that the zones of injuries significantly affect the final visual outcome[16-17]. In our study, even if patients with zone Ⅰ injury had a worse final visual outcome, the difference was not statistically significant. This could be due to the relatively small number of study subjects in the present study.
In our study the prevalence of monocular blindness was found to be high (34.3%) with the majority occurring in males. This is similar to the study findings in central Ethiopia[18]but higher than what was reported in Croatia[10].This could be due to the difference in the setup of the eye care as well as population characteristics, transport facility, distance to health facilities and awareness level which have an impact on severity of injury and time of presentation as is the case in our study where majority of patients had serious eye injuries and came to hospital late.
Although there were patients who had no documented final visual acuity, their number was small to affect the statistical analysis. Nevertheless, this should be taken into consideration. In this study we found that the type of injury, the initial visual acuity and time of presentation were main determinants of the final visual acuity. The same has been shown by Karamanetal[14].Similarly, the timing of surgery after arrival (diagnosis to the surgical intervention) significantly affected the final visual outcome of our study subjects. Nearly one third of patients underwent eye surgery and the most commonly performed surgical procedure was corneal repair as it was the case in study done in Menellik Ⅱ hospital[16]but the rate of evisceration in the present study was very low compared to a similar study[16].
In our study, the higher prevalence of eye injuries (70.2%) occurred in the younger population (30y and below). This finding is similar to a study conducted in Iran[19]and Upper East Ghana[15].The average age of patients with eye injury was 25.3y which is nearly similar to the other studies conducted in developing countries[15-16]but lower than that of developed countries[20-23]. This difference could be due to difference in population composition in developing countries and developed countries. In this study, male patients predominated. Male predominance in ocular injury was documented in a number of studies[10-11,15-16,19,21-23]and could probably be the result of nature of men’s jobs and other activities and difference in the health seeking ability of men especially in developing countries as men are the head of household and decision makers on economic issues; as most of the studies are hospital based.
In our study, most of the injuries occurred in farmers. This is similar to a study conducted in Menellik Ⅱ hospital[16]. The occurrence of injury mostly in farmers could be due to the high risk associated with agricultural activities and the large proportion of Ethiopian population who are farmers. The majority of patients presented later than 24 hours which significantly affected the final visual acuity. Similar finding is documented in a Menellik Ⅱ study[16].
In this study, we found variation among the months in occurrence of eye injuries. The highest number of eye injuries occurred in June while the lowest frequency was seen in July. This finding is similar to study conducted in Pakistan[24].This could be due to the life style of Ethiopian people whereby majority of people are farmer and June is the time when agricultural activity is at its peak.
In this study, most injuries were work related and none of the patients used eye protection even when needed. This is not in agreement with reports from other studies in industrialized countries[14,20]where most eye injuries occurs in leisure or sport places[10,20-21]. This could be due to the difference in the availability of awareness creation activities and safety precautions. More than three fourth of injuries in this study occurred accidentally and injuries due to assault also contributed a lot. This might be due to the less attention that is given by people to take preventive measures as well as the level of awareness that the public has on injuries in general and eye injuries in particular.
In this study, most eye injuries occurred at residential area during domestic activities, at the farm, on the street and in the jungle. This is in agreement with reports from Croatia[10]and Nigeria[11]but differ from study in Glasgow[20]where sport and leisure areas accounted for the majority of eye injuries. These differences and similarities could be due to the difference and the similarity in the population characteristics, habit and living conditions of the different population. It was also found in the study that significant difference in place of injuries existed between males and females whereby males were more likely to be injured at farm place and on the street where as females were more likely to be injured at home and in the jungle. This could be explained by the difference in gender activity divisions that exist in the majority of Ethiopian population where by females spend more time at home and fetching fire woods and males spend more times at farm and outdoor.
As our study is a hospital based, it is expected to have all the weaknesses, like missing less serious eye injuries, of these types of studies. The followup duration for final visual acuity might not be the optimum but still useful information can be generated from the findings related to final visual acuity outcome.
Ocular injury is a major cause of ocular morbidity in the study setting. Majority of the ocular injuries were work-related and none of these patients had eye protection. Monocular blindness due to globe injuries was high and occurred most frequently in males, at home and mainly caused by open globe injuries and blunt objects. The final visual acuity outcome was significantly affected by presenting visual acuity, duration of presentation, type of injuries and presence of other complications. Being young, male, and farmer were the common risk factors for ocular injury.
In order to reduce the burden of eye injury and trauma related blindness, concerted effort is needed especially from those working in the area of preventive medicine. The public should be educated on eye health in general and eye injury in particular. Special emphasis should be given to occupational hazard as the majority of eye injuries were work related.
REFERENCES
1 Negrel AD. Magnitude of eye injuries worldwide.JCommEyeHealth1997;10(24):49-53
2 Thylefors B. Epidemiological patterns of ocular trauma.AustNZJOphthalmol1992;20(2):95-98
3 Omolase CO, Omolade EO, Ogunleye OT,Omolase BO, Ihemedu CO, Adeosun OA.Pattern of ocular injuries in owo, Nigeria.JOphthalmicVisRes2011;6 (2): 114-118
4 Oluyemi F. Epidemiology of penetrating eye injury in Ibadan: a 10-year hospital-based review.MiddleEastAfrJOphthalmol2011;18 (2): 159-163
5Schein OD, Hibberd PL, Shingleton BJ, Kunzweiler T, Frambach DA, Seddon JM, Fontan NL, Vinger PF.The spectrum and burden of ocular injury.Ophthalmology1988;95 (3): 300-305
6 Berhane Y , Worku A , Bejiga A, Adamu L, Alemayehu W, Bedri A, Ayalew A, Adamu Y, Gebre T, Kebede TD, West E, West S. National survey on blindness, low vision and trachoma in Ethiopia.Ethiop.J.HealthDev2007;21(3):185-203
7 Pieramici DJ, Sternberg P Jr, Aaberg TM Sr,Bridges WZ Jr, Capone A Jr, Cardillo JA, de Juan E Jr, Kuhn F, Meredith TA, Mieler WF, Olsen TW, Rubsamen P,Stout T.. A system for classifying mechanical injuries of the eye (globe). The Ocular Trauma Classification Group.AmJOphthalmol1997;123(6):820-831
8 Kuhn F, Morris R, Witherspoon CD, Heimann K, Jeffers JB, Treister G. A standardized classification of ocular trauma.Ophthalmology1996;103 (2): 240-243
9 Cruciani F, Lucchetta F, Regine F, Salandri AG, Abdolrahimzadeh B, Balacco Gabrieli C. Work-related accidents of ophthalmologic interest in Italy during 1986-1991.Ophthalmologica1997;211(4):251-255
10 Karaman K, Gverovic-Antunica A, Rogosic V, Lakos-Krzelj V, Rozga A, Radocaj-Perko S.Epidemiology of adult eye injuries in Split- Dalmatian County.CroatMedJ2004;45: 304-309
11 Adeyinka O. Eye injuries in children and adolescents: areport of 205 cases.JNatlMedAssoc2009;101(1):51-56
12 Soliman MM, Macky TA. Pattern of ocular trauma in Egypt.GraefesArchClinExpOphthalmol2008; 246(2): 205-212
13 Cao H, Li L, Zhang M, Li H. Epidemiology of patients hospitalized for ocular trauma in the Chaoshan region of China, 2001-2010.PLoSOne2012; 7(10):e48377
14 Karaman K, Znaor L, Lakos V, Olujic I. Epidemiology of pediatric eye injury in Split-Dalmatia County.OphthalmicRes2009;42 (2): 199-204
15 Gyasi M, Amoaku W, Adjuik M. Epidemiology of hospitalized ocular injuries in the Upper East Region of Ghana.GhanaMedJ2007;41 (4): 171-175
16 Mulugeta A. Bayu S. Pattern of perforating ocular injuries at Menelik Ⅱ hospital, Addis Ababa.Ethiop.JHealthDev2001;15(2):131-137
17 Gothwal VK, Asolph S, Jalali S, Naduvilath TJ. Demography and prognostic factors of ocular injuries in South India.AustNZJOphthalmol1999; 27(5):318-325
18 Tesfaye A, Bejiga A. Ocular injuries in a rural Ethiopian community.EastAfrMedJ2008; 85(12):593-596
19 Mansouri M, Faghihi H, Hajizaden F, Rasoulinejad SA, Rajabi MT, Tabatabaey A, Shoaee S, Faghihi S, Khabazkhoob M.Epidemiology of open globe injuries in Iran: Analysis of 2,340 Cases in 5 Years (Report No. 1).Retina2009; 29 (8): 1141-1149
20 McEwen C J. Eye injuries: a prospective survey of 5671 cases.BrJOphthalmol1989; 73(11): 888-894
21 Smith AR, O’Hagan SB, Gole GA. Epidemiology of open-and closed-globe trauma presenting to Cairns Base Hospital, Queensland.ClinExperimentOphthalmol2006; 34(3): 252-259
22 Kanoff JM, Turalba AV, Andreoli MT, Andreoli CM. Characteristics and outcomes of work-related open globe injuries.AmJOphthalmol2010; 150(2):265-269
23 Koo L, Kapadia MK, Singh RP, Sheridan R, Hatton MP. Gender differences in etiology and outcome of open globe injuries.JTrauma2005; 59(1):175-178
24 Qureshi M B.Ocular injury pattern in Turbat, Baluchistan, Pakistan.JCommEyeHealth1997;10(24): 57-58
摘要
关键词:眼外伤;单眼失明;眼球损伤;危险因素
DOI:10.3980/j.issn.1672-5123.2016.5.05
通讯作者:Yeshigeta Gelaw. dryeshi@yahoo.com
目的:探究埃塞俄比亚西南部的眼外伤类型、严重程度和预后因素。
方法:回顾性研究。选取2009-04/09就诊于季马大学专科医院的眼外伤患者纳入本研究。所有患者均进行详细诊断,并接受全面眼科检查。SPSS 13.0进行数据分析,P<0.05表示差异有统计学意义。
结果:眼外伤总患病率为3.03%。近99%的眼外伤为机械性损伤。多数眼外伤(53.2%)与工作相关,这些患者受伤时均未使用眼部防护装置。在170例眼外伤中,57.6%为闭合性眼外伤,42.4%为开放性眼外伤。闭合性眼外伤较开放性眼外伤的损伤程度较低,且有明显较好的视力预后(P<0.05)。最终视力和就诊时视力与从诊断到手术的时间间隔明显相关(P<0.05)。眼外伤致单眼失明患者59例(34.3%)。就诊晚、就诊时视力差、开放性眼外伤和并发症是导致低视力的危险因素。
结论:大多数眼外伤发生在工作场所,且有较大比例的眼外伤患者发展为单眼失明。为预防严重的眼外伤,应在家中和工作场所普及眼部健康教育知识并做好安全防护措施。
引用:Bekele S, Gelaw Y.埃塞俄比亚西南地区眼外伤类型和预后因素的回顾性研究. 国际眼科杂志2016;16(5):811-817
·Original article·
