Retrobulbar ocular blood flow changes after phacoemulsification in patients
2016-05-17YinYingZhaoJunHuaLiPingJunChangYunZhao
Yin-Ying Zhao, Jun-Hua Li,Ping-Jun Chang, Yun-E Zhao
Foundation item:Supported by Nature Science Foundation of Zhejiang Province(No.LY12H12004)
1School of Ophthalmology and Optometry, Wenzhou Medical University, Wenzhou 310000, Zhejiang Province, China
2Affiliated Eye Hospital, Wenzhou Medical University, Wenzhou 310000, Zhejiang Province, China
Correspondence to:Yun-E Zhao. School of Ophthalmology and Optometry, Wenzhou Medical University, 270 Xueyuan Road, Wenzhou 325027, Zhejiang Province, China. zye@mail.eye.ac.cn
Received: 2015-09-08 Accepted: 2016-02-22
白内障超声乳化术后球后血流动力学变化的研究
赵银莹,李军花,常平骏,赵云娥
(作者单位:1310000中国浙江省温州市,温州医科大学眼视光学院;2310000中国浙江省温州市,温州医科大学附属眼科医院)
Retrobulbar ocular blood flow changes after phacoemulsification in patients
Yin-Ying Zhao1,2, Jun-Hua Li1,2,Ping-Jun Chang1,2, Yun-E Zhao1,2
Foundation item:Supported by Nature Science Foundation of Zhejiang Province(No.LY12H12004)
1School of Ophthalmology and Optometry, Wenzhou Medical University, Wenzhou 310000, Zhejiang Province, China
2Affiliated Eye Hospital, Wenzhou Medical University, Wenzhou 310000, Zhejiang Province, China
Correspondence to:Yun-E Zhao. School of Ophthalmology and Optometry, Wenzhou Medical University, 270 Xueyuan Road, Wenzhou 325027, Zhejiang Province, China. zye@mail.eye.ac.cn
Received: 2015-09-08Accepted: 2016-02-22
白内障超声乳化术后球后血流动力学变化的研究
赵银莹,李军花,常平骏,赵云娥
(作者单位:1310000中国浙江省温州市,温州医科大学眼视光学院;2310000中国浙江省温州市,温州医科大学附属眼科医院)
Abstract
•AIM:To evaluate retrobulbar ocular blood flow changes after phacoemulsification.
•METHODS:Prospective consecutive study. Forty-six eyes from 46 cataract patients scheduled for phacoemulsification surgery at Affiliated Eye Hospital, Wenzhou Medical College were recruited, of which 22 patients with normal blood pressure and 24 patients with hypertension. All eyes were examined by a color Doppler imaging at before, 4h, 1d after surgery. Resistance indexes(RIs), peak systolic flow velocity(PSV), end-diastolic flow velocity(EDV) were assessed in the ophthalmic artery(OA), central retinal artery(CRA), and short posterior ciliary arteries(PCA).
•RESULTS:RIs of a retrobulbar ocular vessels are stable at 4h and 1d in both group postoperatively. A slight decrease in PSV of PCA in hypertension patients, while a slightly increase in normal patients at 4h postoperatively was observed(10.22±4.39vs11.73±4.69). There were no significant difference between them(P=0.089). PSV and EDV in CRA are lower in hypertension patients but without statistical significance compared with normal patients. There was a statistically significant decrease in EDV of the PCA in hypertension patients at 4h postoperatively compared with preoperatively(3.23±1.10vs3.63±1.15,P=0.036).
•CONCLUSION:Retinal blood flow was disturbed at super-early after phacoemulsification. Age and hypertension are important risk factors to phacoemusification.
KEYWORDS:•phacoemulsification;blood flow;color Doppler imaging;retina
Citation:Zhao YY, Li JH, Chang PJ, Zhao YE. Retrobulbar ocular blood flow changes after phacoemulsification in patients.GuojiYankeZazhi(IntEyeSci) 2016;16(5):793-797
INTRODUCTION
As the most commonly performed cataract surgery, phacoemulsification adopt applicants maximum vacuum to reduce the power and make the surgery efficient and rapid. Nevertheless, most of surgeons ignore the high intraocular pressure during surgery, which may disturb the retrobulbar circulation. Intraocular pressure(IOP) was reported to fluctuate from 66.1 to 196.6 mm Hg during nuclear disassembly of the surgery on cadaver eyes. Moreover, the final pressure was up to 73.2 mm Hg[1]. Zhaoetal[2]described that the static IOP increased to 96 mm Hg during cortical cleanup, while the dynamic IOP fluctuated to 74 mm Hg.
Even though it is the common clinical experience that most eyes do outstandingly well after surgery, there are still few of people discovered visual loss after uneventful phacoemulsification. Several case reports and clinical researches indicated that cataract surgery might be associated with an increased incidence of nonarteritic anterior ischemic optic neuropathy[3-4]. These authors hypothesize that the high IOP associated with cataract surgery maybe a factor to result of nonarteritic anterior ischemic optic neuropathy(NAION). Sprauletal[5]recorded retrobulbar blood flow in humans after phacoemulsification and found cataract extraction temporarily affected ocular hemodynamic. The author postulated that the increased IOP required during phacoemulsification is the main factor. The transient high pressure didn’t seem innocuous completely.
Because of the function referred to as autoregulation, blood flow in retina is stably maintained despite certain fluctuation in ocular perfusion pressure(OPP). However, autoregulation insufficiency leaded inadequate response to changes in perfusion pressure, which may induce ischemia.
This pilot study was set to explore possible changes in ocular blood flow in patients with vascular dysfunction early after the phacoemulsification surgery.
SUBJECTS AND METHODS
This prospective study was of consecutive age-related patients with hypertension and age-matched healthy patients as control group. All subjects were over 60y old and no other systemic pathology that would interfere with ocular or systemic circulation. Hypertension was defined as systolic blood pressure >140 mm Hg or diastolic blood pressure >90 mm Hg, moreover, diagnosed by physician[6]. Patients or controls with ocular conditions that may have affected the blood circulation, such as glaucoma, age-related maculopathy and high degree of myopia were excluded. Patients had phacoemulsification for uncomplicated cataract with IOL implantation. One eye of each subject was randomly selected by a process of alternation.
The procedures conformed with the Declaration of Helsinki and of the local ethical committee of Wenzhou Medical University(Wenzhou, Zhejiang Province, China). All subjects were informed of the procedure and provided written informed consent.
Surgery TechniqueAll surgeries were performed under topical anesthesia by the same surgeon after the pupil was maximally dilated. A 2.2 mm clear corneal incision and 1.0 mm side port paracentesis was made. And a 5.5 mm continuous curvilinear capsulorhexis was created followed by hydrodissection, phacoemulsification, aspiration of cortical masses, with Infiniti Vision System(Alcon, Inc.), and introduction of foldable IOLs. Once the viscoelastic material was removed, the incision was closed by stroma hydration without sutures. Postoperatively, all patients used topical steroid and antibiotic eye drops 4 times a day for 1wk and then tapered.
The intraoperative effective phacoemulsification time(EPT) and energy of the phaco-machine were documented during the surgery. Additionally, the irrigation column height and the maximum vacuum were recorded in different stage of the procedure.
Blood pressure was assessed with an electrocardio-monitor(MP2 IntelliVue, Philips Co., Eindhoven, The Netherlands) on the upper right arm of the patient in different stage of the surgery(before, nucleus removal, I/A stage and endpoint). Noninvasive device to measure systemic hemodynamics.
Color Doppler Imaging MeasurementRetrobulbar hemodynamic evaluation was performed by the same experienced operator in all subjects preoperatively, 4h and 1d postoperatively using Doppler Sonography(MyLab 90, Esaote, Genova, Italy).
After twenty minutes resting in the supine position, the patients were measured with a 7.5 MHz linear-array transducer. The transducer was applied gently to the closed eyelid using a coupling gel without any pressure on the eye. Resistance indexes(RIs), peak systolic flow velocity(PSV), end-diastolic flow velocity(EDV) were assessed in the ophthalmic artery(OA), central retinal artery(CRA), and short posterior ciliary arteries(PCA).
To ensure that the same location was repeatedly measured, patients were asked to keep the head tiled 30° angle, and eye closed during the examination.
Reproducibility of contour line and disc assessment was measured by having the same operator draw contour lines for 30 scans, delete them, and then, on a different day, redraw the contour lines. The differences in area for each contour line were recorded for each eye.
Intraocular pressure was measured before the CDI examination.
Statistical AnalysisStatistical analysis was performed using SPSS software(USA). Student’st-test for unpaired data was utilized for comparisons between groups. RI of retrobulbar vessels, PSV&EDV in CRA were analyzed by pairedt-tests. PSV&EDV in PCA and OA was confirmed by means of non-parametric paired tests. The relationships among variables were analyzed by Pearson correlation analyses.P≤0.05 was regarded as significant.
RESULTS
This study enrolled 46 eyes of 46 patients. Baseline characteristics of patients are presented in Table 1. There were no significant differences between the 2 groups.
The mean IOP at each time point were provided in Table 2. There was no statistical difference between the each time point of IOP in the two groups.
Table 3 shows that RIs of retrobulbar vessels at different time point in hypertension and normal patients. The CRA at 4h
Table 1Clinical and demographic data of patients

ParameterHypertensionNormalPNumberofpatients(eyes)24eyes22eyes>0.05Meanage(a)74±6.7872.4±7.87>0.05Sex(M/F)10/1414/8>0.05Accumulatedenergycomplexparameters10.14±8.227.89±6.29>0.05Visualacuity(before)0.88±0.240.97±0.43>0.05Visualacuity(postoperative)0.11±0.070.20±0.12>0.05
Table 2Intraocular pressure recorded during the follow-up time

GroupBeforeAfter4h1dPHypertension13.24±2.8115.49±4.5414.69±4.53>0.05Normal13.11±2.6217.26±5.5813.45±4.01>0.05
Table 3Resistant index evaluated in retrobulbar blood vessels at different time point

TimeOAHyperNormalPCAHyperNormalCRAHyperNormalBaseline0.821±0.0450.793±0.5960.655±0.0640.638±0.0480.725±0.0430.709±0.0364h0.823±0.0430.790±0.0610.671±0.0620.633±0.0570.744±0.0450.708±0.0351d0.824±0.0440.791±0.0590.661±0.0470.647±0.0510.732±0.0560.707±0.035P10.3800.3570.3780.5140.0820.897P20.2310.7070.5840.3930.5480.817
P1:Comparison of RI between preoperative and 4h postoperative;P2:Comparison of RI between preoperative and 1d postoperative. OA:Ophthalmic artery;PCA:Posterior ciliary artery;CRA:Central retinal artery.
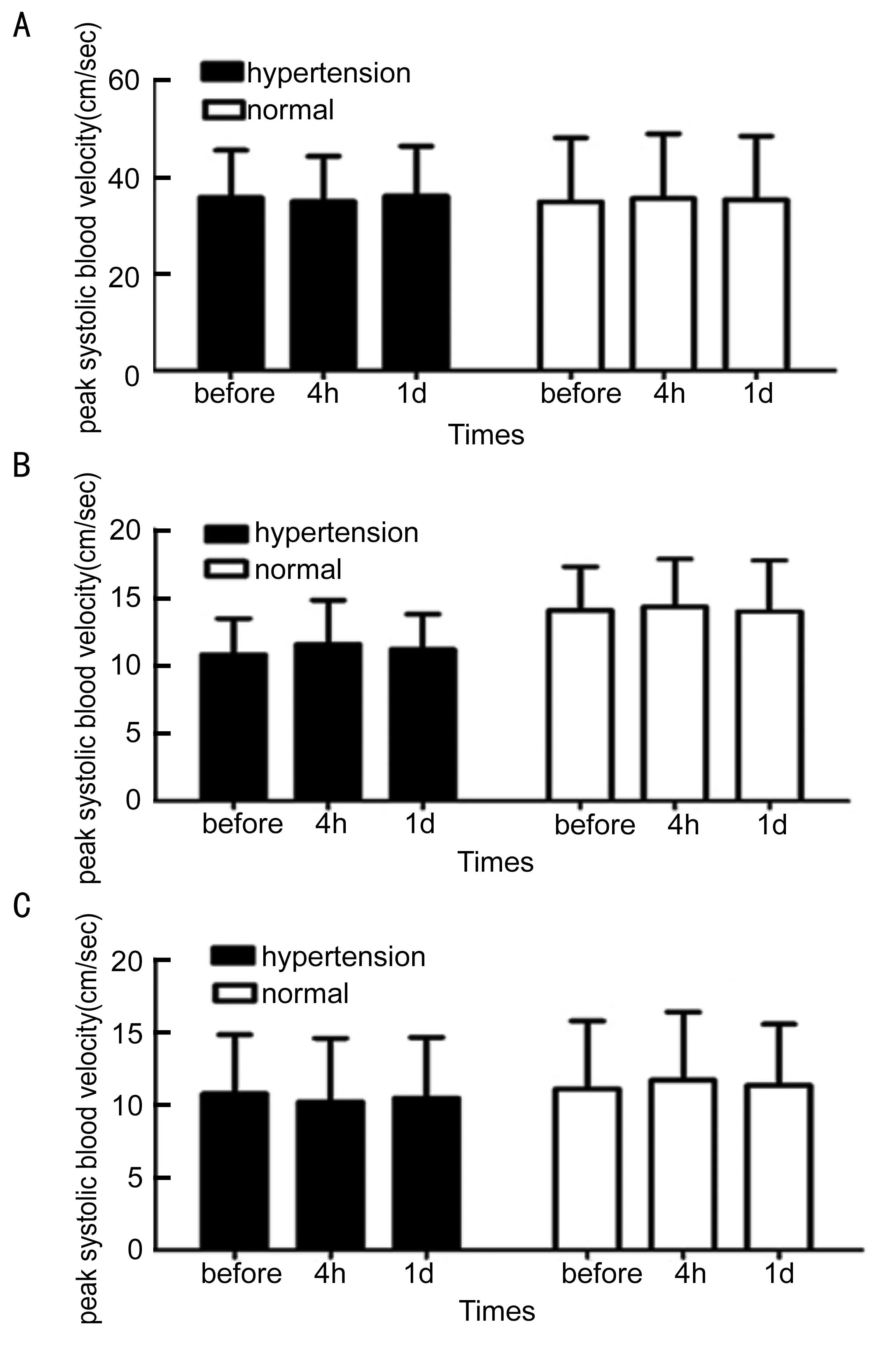
Figure 1PSV observed in different time in retrobulbar blood vessel between hypertension and normal patientsA:Represented ophthalmic artery(OA);B:Represented central retinal artery(CRA);C:Represented posterior ciliary artery(PCA).
postoperative of hypertension patients was slight higher compare with preoperative(0.725±0.043vs0.744±0.045), while there were no significant differences between them. RIs are stable at 4h and one day postoperatively.
The PSV, EDV differences observed in the OA, CRA and PCA before and after the surgery are provided in Figure 1 and Figure 2. There was a statistically significant decrease in EDV of the PCA in hypertension patients at 4h compared with preoperatively(3.23±1.10vs3.63±1.15,P=0.036). All other parameters assessed by CDI measurements in the OA, CRA and PCA appeared to be stable. A slight decrease in PSV of PCA in hypertension patients, while a slightly increase in normal patients at 4h postoperatively was observed(10.22±4.39vs11.73±4.69). There were no significant difference between them(P=0.089). Furthermore, we found PSV and EDV in CRA are lower in hypertension patients but without statistical significance compared with normal patients.
DISCUSSION
Although phacoemulsification made cataract surgery easier and safer, this common surgery continues to carry ocular risks. Several researchers have expressed concerns about IOP elevation during phacoemulsification. Kamaeetal[7]described the peak IOPs exceeded 60 mm Hg during injection of the IOLs. Kreutzeretal[8]evaluated IOP was 60 mm Hg or higher for approximately 1min during the surgery. These researchers proposed the transient IOP may damage eyes with compromised retinal perfusion. However, there is no enough evidence to indicate that such IOP elevation induce retinal damage during phacoemulsification[9]. Azuara-Blancoetal[10]reported that acute changes in IOP affected the cup of the optic nerve head, while the compliance appeared to be

Figure 2EDV observed in different time in retrobulbar blood vessel between hypertension and normal patients. There was a significant decrease of PCA in hypertension group on 4h postoperatively(XP<0.05)A:Represented ophthalmic artery(OA);B:Represented central retinal artery(CRA);C:Represented posterior ciliary artery(PCA).
variable between cases. Schickeetal[11]reported that blood flow can’t be detected during LASIK-ring suction in 90% subjects. Whereas, there is few researches of ocular hemodynamic changes after phacoemusification. Sprauletal[5]reported that ocular blood flow decrease 3d after cataract surgery. However, their participants are all normal patients, and the measure time point was 3d after surgery. According to their result, we speculated that hypertension patients are more affected in early postoperative period. To our knowledge, no study has been reported to investigate the retrobulbar ocular blood flow after early postoperatively.
In the present study, we focus on the effect of phacoemulsification in patients with cataract on ocular hemodynamic parameters. All of the subjects are senile patients. Patients with hypertension were included. Conwayetal[12]suggested that the hemodynamic responses returned immediately to normal as soon as IOP elevated above 85 mm Hg for 90s. However their subjects were young persons with excellent vascular autoregulation. Autoregulation is the ability to maintain blood flow constantly despite alterations in perfusion pressure. Several reports suggested that autoregulation disappeared in the human eye if the IOP is increased above 60 mm Hg[13-14]. Furthermore hypertension alters the structure of blood vessels and disrupts blood flow[15-16]. Patients with hypertension may impair with autoregulation. Moreover, Grohetal[17]indicated that retinal and CRA blood flow decreased approximately 6% to 11% per decade.
In our study, we found RIs in retrobulbar ocular vessels are stable at 4h and 1d after surgery in normal and hypertension patients. PSV are stable in retrobulbar vessels at 4h and 1d after surgery in normal and hypertension patients. In the present study, a significant decreased in EDV of PCA in hypertension patients at 4h postoperatively were found. PCA is important for the perfusion of optical nerve. Most ischemic optic neuropathies are attributed to interference of blood flow originating within the posterior ciliary circulation[18]. It has been reported that CRA showed a faster autoregulatory response than the PCA[14]. This conclusion can explain our result that EDV in PCA is significant decreased at 4h after surgery. It was coincident with our result that the PCA circulation is highly dependent on IOP[19].
It cannot be answered from our data whether the blood flow change seen here is indeed a risk factor for loss of vision in patients after phacoemulsification. Long-term study is required to study whether this retinal blood hemodynamic response in patients with server cataract complies with disease of cardiovascular disease.
In our study, only blood velocities in the CRA are measured, but vessel diameters cannot be quantified because of the limited resolution of ultrasound devices.
Even though it is not possible to examine the blood flow during phacoemusification, we can postulated the changes after the surgery.
REFERENCES
1 Khng C, Packer M, Fine IH, Hoffman RS, Moreira FB. Intraocular pressure during phacoemulsification.JCataractRefractSurg2006;32(2):301-308
2 Zhao Y, Li X, Tao A, Wang J, Lu F. Intraocular pressure and calculated diastolic ocular perfusion pressure during three simulated steps of phacoemulsificationinvivo.InvestOphthalmolVisSci2009;50(6):2927-2931
3 Fontes BM, Jung LS, Soriano ES, Chicani CF. Nonarteritic anterior ischemic optic neuropathy after uneventful phacoemulsification:case report.ArqBrasOphthalmol2007;70(3):544-546
4 Lee H, Kim CY, Seong GJ, Ma KT. A case of decreased visual field after uneventful cataract surgery:nonarteritic anterior ischemic optic neuropathy.KoreanJOphthalmol2010;24(1):57-61
5 Spraul CW, Amann J, Lang GE, Lang GK. Effect of cataract extraction with intraocular lens implantation on ocular hemodynamics.JCataractRefractSurg1996,22(8):1091-1096
6 Wong TT, Wong TY, Foster PJ, Crowston JG, Fong CW, Aung T;SiMES Study Group. The relationship of intraocular pressure with age, systolic blood pressure, and central corneal thickness in an asian population.InvestOphthalmolVisSci2009;50(9):4097-4102
7 Kamae KK, Werner L, Chang W, Johnson JT, Mamalis N. Intraocular pressure changes during injection of microincision and conventional intraocular lenses through incisions smaller than 3.0 mm.JCataractRefractSurg2009;35(8):1430-1436
8 Kreutzer TC, Al Saeidi R, Kampik A, Grueterich M. Real-time intraocular pressure measurement in standard and microcoaxial phacoemulsification.JCataractRefractSurg2010;36(1):53-57
9 Mackool RJ. Lack of evidence of damage from elevated IOP during phacoemulsification.JCataractRefractSurg2010;36(7):1244
10 Azuara-Blanco A, Harris A, Cantor LB, Abreu MM, Weinland M. Effects of short term increase of intraocular pressure on optic disc cupping.BrJOphthalmol1998;82(8):880-883
11 Schicke SH, Krumeich J, Duncker GI, Scheibel S, Thielscher M. Retinal colour duplex scanning during LASIK-ring suction with different keratomes.GraefesArchClinExpOphthalmol2008;246(7):1009-1015
12 Conway ML, Wevill M, Benavente-Perez A, Hosking SL. Ocular blood-flow hemodynamics before and after application of a laserinsitukeratomileusis ring.JCataractRefractSurg2010;36(2):268-272
13 Bek T, Hajari J, Jeppesen P. Interaction between flicker-induced vasodilatation and pressure autoregulation in early retinopathy of type 2 diabetes.GraefesArchClinExpOphthalmol2008;246(5):763-769
14 Kaya S, Kolodjaschna J, Berisha F, Schmetterer L, Garhöfer G. Comparison of the autoregulatory mechanisms between central retinal artery and posterior ciliary arteries after thigh cuff deflation in healthy subjects.MicrovascRes2011;82(3):269-273
15 Iadecola C, Davisson RL. Hypertension and cerebrovascular dysfunction.CellMetab2008;7(6):476-484
16 He Z,Nguyen CT, Armitage JA, Vingrys AJ, Bui BV. Blood pressure modifies retinal susceptibility to intraocular pressure elevation.PLoSONE2012;7(2):e31104
17 Groh MJ, Michelson G, Langhans MJ, Harazny J. Influence of age on retinal and optic nerve head blood circulation.Ophthalmology1996;103(3):529-534
18 Hayreh SS. Blood supply of the optic nerve head and its role in optic atrophy, glaucoma, and oedema of the optic disc.BrJOphthalmol1969;53(11):721-748
19 Joos KM, Kay MD, Pillunat LE, Harris A, Gendron EK, Feuer WJ, Steinwand BE. Effect of acute intraocular pressure changes on short posterior ciliary artery haemodynamics.BrJOphthalmol1999;83(1):33-38
摘要
关键词:白内障超声乳化手术;球后血流;彩色多普勒超声成像;视网膜
DOI:10.3980/j.issn.1672-5123.2016.5.01
通讯作者:赵云娥,毕业于温州医科大学,硕士,主任医师,教授;研究方向:白内障. zyehzeye@126.com
作者简介:赵银莹,毕业于温州医科大学,博士,住院医师,讲师;研究方向:白内障。
基金项目:浙江省自然科学基金(No.LY12H12004)
目的:观察白内障超声乳化合并人工晶状体植入术后患者的球后血流动力学的变化。
方法:前瞻性对照研究。 选取我院行单眼白内障超声乳化吸除并植入人工晶状体患者46例。高血压组24名,正常血压组22名,年龄>60岁。分别于术前、术后4h与术后1d行彩色多普勒超声诊断仪(color Doppler imagining, CDI)检查患者术眼球后血流。检测指标包括眼动脉(OA)、视网膜中央动脉(CRA)、睫状后动脉(PCA)的阻力指数(RI)、最大收缩期血流速度(PSV)、舒张末期血流速度(EDV)。不同时间点比较采用Mann-Whitney Test方法。
结果:两组球后血流的RI在术后4h及术后1d均保持稳定。术后4h,高血压患者PCA的PSV轻度降低,而正常血压患者轻度升高,两组间无统计学差异(10.22±4.39vs11.73±4.69,P=0.089)。高血压组患者的CRA的PSV和EDV在各时间点均低于正常血压组患者,但均无显著差异。高血压组术后4h的PCA的EDV较术前有显著差异(3.23±1.10vs3.63±1.15,P=0.036)。
结论:年龄相关性白内障超声乳化合并人工晶状体植入术后,球后血流动力存在一定的波动,年龄及高血压是重要的影响因素。
引用:赵银莹,李军花,常平骏,赵云娥. 白内障超声乳化术后球后血流动力学变化的研究.国际眼科杂志2016;16(5):793-797
·Original article·
