不同收缩压、不同降压方案对老年高血压脑出血患者预后影响的比较研究
2016-05-09李芳会
李芳会
710043陕西省西安市东郊第一职工医院
不同收缩压、不同降压方案对老年高血压脑出血患者预后影响的比较研究
李芳会
710043陕西省西安市东郊第一职工医院
【摘要】目的 比较不同收缩压、不同降压方案对老年高血压脑出血(HICH)患者预后的影响。方法选取2011年2月—2015年6月在西安市东郊第一职工医院内科住院的老年HICH患者541例,按照入院时收缩压将患者分为A组(收缩压<180 mm Hg)179例、B组(收缩压为180~200 mm Hg)227例和C组(收缩压>200 mm Hg)135例;按照降压方案不同将患者分为非强化降压组309例和强化降压组232例。比较不同收缩压患者入院时脑血肿体积、脑水肿体积、美国国立卫生研究院卒中量表(NIHSS)评分及发病90 d改良Rankin量表(mRS)评分;比较不同降压方案及强化降压组不同收缩压患者入院时和治疗后7 d脑血肿体积、脑水肿体积及发病90 d mRS评分。结果B组和C组患者入院时脑血肿体积大于A组,入院时NIHSS评分及发病90 d mRS评分高于A组(P<0.05);C组患者入院时脑血肿体积大于B组,脑水肿体积大于A组,发病90 d mRS评分高于B组(P<0.05)。入院时非强化降压组与强化降压组患者脑血肿体积、脑水肿体积比较,差异无统计学意义(P>0.05);治疗后7 d强化降压组患者脑血肿体积、脑水肿体积小于非强化降压组,发病90 d mRS评分低于非强化降压组(P<0.05)。强化降压组不同收缩压患者入院时脑血肿体积、脑水肿体积比较,差异无统计学意义(P>0.05);B组和C组患者治疗后7 d脑血肿体积、脑水肿体积大于A组,C组患者发病90 d mRS评分高于A组(P<0.05)。结论入院时收缩压较高的老年HICH患者病情更严重、预后更差,强化降压较非强化降压能更有效地改善患者病情严重程度及预后,且收缩压较低的老年HICH患者强化降压效果更佳。
【关键词】颅内出血,高血压性;收缩压;强化降压;预后
李芳会.不同收缩压、不同降压方案对老年高血压脑出血患者预后影响的比较研究[J].实用心脑肺血管病杂志,2016,24(3):56-59.[www.syxnf.net]
Li FH.Comparative study for influence of systolic blood pressure and antihypertensive regimens on prognosis of aged patients with hypertensive intracerebral hemorrhage[J].Practical Journal of Cardiac Cerebral Pneumal and Vascular Disease,2016,24(3):56-59.
高血压脑出血(hypertensive intracerebral hemorrhage,HICH)是指由高血压导致脑实质内血管破裂引起的出血,是一种临床急危重症[1]。长期以来有关脑出血患者急性期的降压治疗方案争议颇多,理论上讲早期降压可缩小血肿体积、避免出血继续增加及二次出血,但过度降压可能引起病灶周围水肿扩大,导致神经功能恶化及病死率升高[2-3]。2013年的INTERACT-2研究为HICH患者早期降压提供了重要依据,该研究结果显示将收缩压控制在140 mm Hg(1 mm Hg=0.133 kPa)以下可降低血肿扩大发生率,且未增加不良事件发生率[4]。老年人既是HICH的高危人群,也是特殊人群。本研究回顾性分析了541例老年HICH患者的临床资料,旨在比较不同收缩压、不同降压方案对老年HICH患者预后的影响,现报道如下。
1资料与方法
1.1纳入与排除标准纳入标准:(1)年龄≥60岁;(2)高血压病程≥1年;(3)符合HICH的诊断标准,并经颅脑CT和/或MRI证实;(4)出血部位为基底核区或丘脑;(5)出血量10~30 ml;(6)脑出血首次发作,且在发病24 h内入院接受治疗;(7)意识清楚。排除标准:(1)严重心、肝、肾功能障碍患者;(2)脑血管畸形患者;(3)颅内肿瘤患者;(4)重度昏迷、脑疝患者;(5)存在脑室出血或脑出血破入脑室无法计算出血量患者。
1.2一般资料选取2011年2月—2015年6月在西安市东郊第一职工医院内科住院的老年HICH患者541例,按照入院时收缩压将患者分为A组(收缩压<180 mm Hg)179例、B组(收缩压为180~200 mm Hg)227例和C组(收缩压>200 mm Hg)135例;按照降压方案不同将患者分为非强化降压组309例和强化降压组232例。
1.3降压方案所有患者卧床休息,并根据病情给予吸氧、脱水降颅压、控制血糖、维持电解质平衡及液体支持等基础治疗。强化降压组患者入院后立即进行强化降压,降压目标为1 h内收缩压降至140 mm Hg以下,并维持该血压目标值;非强化降压组患者的降压目标为24 h内收缩压降至180 mm Hg以下。常用的静脉降压药物包括尼卡地平、乌拉地尔、硝酸甘油等,常用的口服降压药物包括长效钙通道阻滞剂、血管紧张素Ⅱ受体阻滞剂、β1肾上腺素受体阻滞剂等。
1.4观察指标比较不同收缩压患者入院时脑血肿体积、脑水肿体积、美国国立卫生研究院卒中量表(National Institutes of Health Stroke Scale,NIHSS)评分及发病90 d改良Rankin量表(Modified Rankin Scale,mRS)评分;比较不同降压方案及强化降压组不同收缩压患者入院时和治疗后7 d脑血肿体积、脑水肿体积及发病90 d mRS评分。患者均行颅脑CT检查,并根据公式计算脑血肿体积和脑水肿体积,脑血肿体积=最大横截面长轴×最大横截面短轴×出血层面或水肿层面×π/6[5],脑水肿体积=水肿带体积-脑血肿体积。所有患者在发病90 d时通过门诊或电话随访进行mRS评分,其中0~2分为基本康复、3~5分为残疾、6分为死亡。

2结果
2.1不同收缩压患者基线资料比较3组患者年龄、男性比例及糖尿病、电解质紊乱、血脂异常、高热(≥39 ℃)发生率比较,差异无统计学意义(P>0.05,见表1)。
2.2不同收缩压患者疾病严重程度及预后比较3组患者入院时脑血肿体积、脑水肿体积、NIHSS评分及发病90dmRS评分比较,差异均有统计学意义(P<0.05);其中B组和C组患者入院时脑血肿体积大于A组,入院时NIHSS评分及发病90dmRS评分高于A组,差异有统计学意义(P<0.05);C组患者入院时脑血肿体积大于B组,脑水肿体积大于A组,发病90dmRS评分高于B组,差异有统计学意义(P<0.05,见表2)。
2.3不同降压方案患者病情严重程度及预后比较入院时两组患者脑血肿体积、脑水肿体积比较,差异无统计学意义(P>0.05);治疗后7d强化降压组患者脑血肿体积、脑水肿体积小于非强化降压组,发病90dmRS评分低于非强化降压组,差异有统计学意义(P<0.05,见表3)。
2.4强化降压组不同收缩压患者病情严重程度及预后比较强化降压组不同收缩压患者入院时脑血肿体积、脑水肿体积比较,差异无统计学意义(P>0.05);强化降压组不同收缩压患者治疗后7d脑血肿体积、脑水肿体积及发病90dmRS评分比较,差异有统计学意义(P<0.05)。B组和C组患者治疗后7d脑血肿体积、脑水肿体积大于A组,C组患者发病90dmRS评分高于A组,差异有统计学意义(P<0.05,见表4)。
表1不同收缩压患者基线资料比较
Table1Comparisonofbaselinedataofpatientswithdifferentsystolicpressure
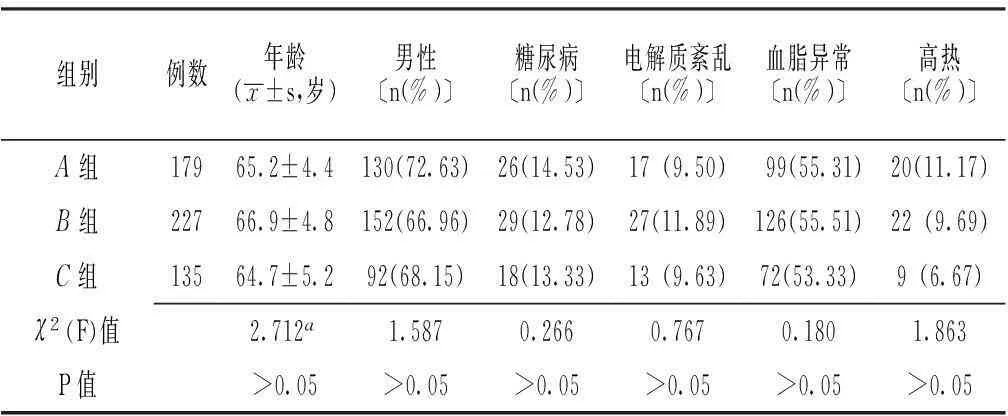
组别例数年龄(x±s,岁)男性〔n(%)〕糖尿病〔n(%)〕电解质紊乱〔n(%)〕血脂异常〔n(%)〕高热〔n(%)〕A组17965.2±4.4130(72.63)26(14.53)17(9.50) 99(55.31) 20(11.17)B组22766.9±4.8152(66.96)29(12.78)27(11.89)126(55.51)22(9.69)C组13564.7±5.292(68.15)18(13.33)13(9.63)72(53.33)9(6.67)χ2(F)值2.712a1.5870.2660.7670.1801.863P值>0.05>0.05>0.05>0.05>0.05>0.05
注:a为F值
3讨论
流行病学资料显示,我国颅内出血(ICH)患者占所有卒中患者的20%~30%,其中高血压所致的ICH约占70%,且高血压是ICH的重要危险因素。有研究显示,HICH患者急性期血压升高可能引起血肿扩大及二次出血,从而增加患者的病死率和残疾率[6-9]。本研究以老年HICH患者作为研究对象,并根据患者入院时收缩压进行分组比较,结果显示B组和C组患者入院时脑血肿体积大于A组,入院时NIHSS评分及发病90 d mRs评分高于A组;C组患者入院时脑血肿体积大于B组,脑水肿体积大于A组,发病90 d mRs评分高于B组。提示收缩压较高的HICH患者病情更严重、预后更差。
有学者指出,不恰当的降压方案可能导致脑血流灌注不足,进一步加重周围水肿。2007年美国心脏病协会(AHA)根据急性脑出血抗高血压研究 (ATACH)结果制定ICH指南,该指南指出ICH早期降压是安全的,但具体降压目标及对预后的影响未进行明确说明[10-11]。2008年以中国人为主要研究对象的INTERACT-1研究结果发表,该研究证实了ICH患者早期强化降压目标为140/90 mm Hg的安全性,但该研究仍未对早期强化降压的预后进行观察[12]。2013年同样以中国人为主要研究对象的INTERACT-2研究结果发表,该研究指出收缩压控制在140 mm Hg以下可以降低血肿扩大发生率,但对不良事件及3个月病死率和致残率无明显影响[13]。本研究根据不同降压方案将老年HICH患者进行分组,结果显示治疗后7 d强化降压组患者脑血肿体积、脑水肿体积小于非强化降压组,发病90 d mRS评分低于非强化降压组,提示强化降压能改善HICH患者病情严重程度及预后。本研究进一步比较强化降压组不同收缩压患者病情严重程度及预后,结果显示B组和C组患者治疗后7 d脑血肿体积、脑水肿体积大于A组,C组患者发病90 d mRS评分高于A组,提示收缩压低的患者强化降压效果更好。
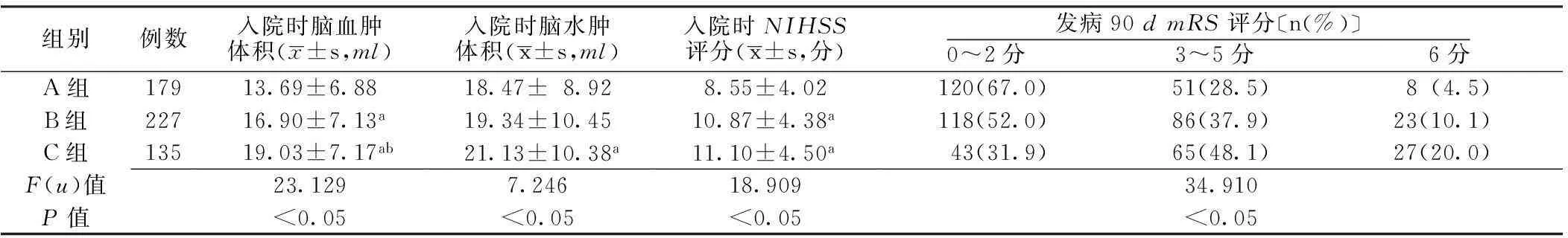
表2 不同收缩压患者疾病严重程度及预后比较
注:NIHSS=美国国立卫生研究院卒中量表,mRS=改良Rankin量表;与A组比较,aP<0.05;与B组比较,bP<0.05;c为u值

表3 不同降压方案患者病情严重程度及预后比较
注:a为u值

表4 强化降压组不同收缩压患者病情严重程度及预后比较
注:a为u值;与A组比较,bP<0.05
综上所述,入院时收缩压较高的老年HICH患者病情更严重、预后更差,强化降压较非强化降压能更有效地改善患者病情严重程度及预后,且收缩压较低的老年HICH患者强化降压效果更佳。但需要注意的是本研究所选的患者均在发病24 h内住院接受治疗,因脑出血发病后首个24 h是脑血肿扩大和颅内水肿加重的主要时期,因此可能对本研究结果产生一定影响。
参考文献
[1]Butcher KS,Jeerakathil T,Hill M,et al.The Intracerebral Hemorrhage Acutely Decreasing Arterial Pressure Trial[J].Stroke,2013,44(3):620-626.
[2]Rodriguez-Luna D,Pieiro S,Rubiera M,et al.Impact of blood pressure changes and course on hematoma growth in acute intracerebral hemorrhage[J].Eur J Neurol,2013,20(9):1277-1283.
[3]Frontera JA.Blood pressure in intracerebral hemorrhage——how low should we go?[J].N Engl J Med,2013,368(25):2426-2427.
[4]Anderson CS,Heeley E,Huang Y,et al.Rapid blood-pressure lowering in patients with acute intracerebral hemorrhage[J].N Engl J Med,2013,368(25):2355-2365.
[5]王文娟,刘艳芳,赵性泉.脑出血治疗指南[J].中国卒中杂志,2006(12):888-899.
[6]张荣军,王晓峰,唐宗椿,等.6374例高血压脑出血患者临床特点的分析及治疗方法的选择[J].中华神经医学杂志,2013,12(1):57-61.
[7]Chiquete E,Ochoa-Guzmán A,Vargas-Sánchez A,et al.Blood pressure at hospital admission and outcome after primary intracerebral hemorrhage[J].Arch Med Sci,2013,9(1):34-39.
[8]Falcone GJ,Biffi A,Devan WJ,et al.Burden of blood pressure-related alleles is associated with larger hematoma volume and worse outcome in intracerebral hemorrhage[J].Stroke,2013,44(2):321-326.
[9]Graffagnino C,Bergese S,Love J,et al.Clevidipine Rapidly and Safely Reduces Blood Pressure in Acute Intracerebral Hemorrhage: The ACCELERATE Trial[J].Cerebrovasc Dis,2013,36(3):173-180.
[10]Broderick J,Connolly S,Feldmann E,et al.Guidelines for the management of spontaneous intracerebral hemorrhage in adults:2007 update:a guideline from the American Heart Association/American Stroke Association Stroke Council,High Blood Pressure Research Council,and the Quality of Care and Outcomes in Research Interdisciplinary Working Group[J].Stroke,2007,116(16):e391-e413.
[11]Qureshi AI.Antihypertensive Treatment of Acute Cerebral Hemorrhage Investigators.Antihypertensive treatment of acute cerebral hemorrhage (ATACH)[J].Neurocritical Care,2007,6(1):56-66.
[12]Anderson CS,Huang Y,Wang JG,et al.Intensive blood pressure reduction in acute cerebral haemorrhage trial (INTERACT):a randomised pilot trial[J].Lancet Neurology,2008,7(5):391-399.
[13]Lattanzi S,Silvestrini M.Optimal achieved blood pressure in acute intracerebral hemorrhage: INTERACT 2[J].Neurology,2015,88(6):557-558.
(本文编辑:谢武英)
Comparative Study for Influence of Systolic Blood Pressure and Antihypertensive Regimens on Prognosis of Aged Patients With Hypertensive Intracerebral Hemorrhage
LIFang-hui.TheFirstWorker′sHospitalofDongjiao,Xi′an,Xi′an710043,China
【Abstract】ObjectiveTo compare the influence of systolic blood pressure and antihypertensive regimens on prognosis of aged patients with hypertensive intracerebral hemorrhage.MethodsFrom February 2011 to June 2015,a total of 541 inpatients with hypertensive intracerebral hemorrhage were selected in the Department of Internal Medicine,the First Worker′s Hospital of Dongjiao,Xi′an,and they were divided into A group(with systolic blood pressure less than 180 mm Hg,n=179),B group(with systolic blood pressure between 180 and 200 mm Hg,n=227)and C group(with systolic blood pressure over 200 mm Hg,n=135)according to systolic blood pressure,into control group(treated by routine antihypertensive regimens,n=309)and observation group(treated by strengthening antihypertensive regimens,n=232) according to antihypertensive regimens.Cerebral hematoma volume,cerebral edema volume and NIHSS score at admission,modified Rankin scale score after 90 days of attack were compared among A group,B group and C group;cerebral hematoma volume and cerebral edema volume at admission and after 7 days of treatment,and modified Rankin scale score after 90 days of attack were compared between control group and observation group,in patients with different systolic blood pressure of observation group.ResultsCerebral hematoma volume at admission of B group,of C group was statistically significantly larger than that of A group,respectively,NIHSS score at admission and modified Rankin scale score after 90 days of attack of B group,of C group was statistically significantly higher than those of A group,respectively(P<0.05);cerebral hematoma volume at admission of C group was statistically significantly larger than that of B group,cerebral edema volume at admission of C group was statistically significant larger than that of A group,while modified Rankin scale score after 90 days of attack of C group was statistically significantly higher than that of B group.No statistically significant differences of cerebral hematoma volume or cerebral edema volume was found between control group and observation group at admission(P>0.05),while cerebral hematoma volume and cerebral edema volume of observation group were statistically significantly smaller than those of control group after 7 days of treatment,and modified Rankin scale score after 90 days of attack of observation group was statistically significantly lower than that of control group(P<0.05).No statistically significant differences of cerebral hematoma volume or cerebral edema volume at admission was found in patients with different systolic blood pressure of observation group(P>0.05);of observation group,cerebral hematoma volume and cerebral edema volume of patients with systolic blood pressure equal or over 180 mm Hg were statistically significantly larger than those of patients with systolic blood pressure less than 180 mm Hg after 7 days of treatment,while modified Rankin scale score of patients with systolic blood pressure equal or over 180 mm Hg was statistically significantly higher than that of patients with systolic blood pressure less than 180 mm Hg(P<0.05).Conclusion The severity of illness and prognosis of aged hypertensive intracerebral hemorrhage patients with higher systolic blood pressure at admission are more severe and worse,and the effect of strengthening antihypertensive regimens is relatively better in patients with lower systolic blood pressure.
【Key words】Intracranial hemorrhage,hypertensive;Systolic blood pressure;Enhanced blood pressure;Prognosis
(收稿日期:2015-12-06;修回日期:2016-03-15)
【中图分类号】R 743.34
【文献标识码】B
doi:10.3969/j.issn.1008-5971.2016.03.015
·疗效比较研究·
