Metabolic syndrome among infertile women with polycystic ovary syndrome
2015-12-22IbrahimAbdelazimWalidFarokElsawah
Ibrahim A. Abdelazim, Walid Farok Elsawah
1Professor of Obstetrics and Gynecology, Ain Shams University, Cairo, Egypt and Ahmadi Hospital, Kuwait Oil Company (KOC), Kuwait
2Specialist of Critical Care and Emergency, Alexandria University, Cairo, Egypt and Ahmadi Hospital, Kuwait Oil Company (KOC), Kuwait
Metabolic syndrome among infertile women with polycystic ovary syndrome
Ibrahim A. Abdelazim1, Walid Farok Elsawah2
1Professor of Obstetrics and Gynecology, Ain Shams University, Cairo, Egypt and Ahmadi Hospital, Kuwait Oil Company (KOC), Kuwait
2Specialist of Critical Care and Emergency, Alexandria University, Cairo, Egypt and Ahmadi Hospital, Kuwait Oil Company (KOC), Kuwait
ARTICLE INFO
Article history:
Received 11 July 2014
Received in revised form 10 October 2014
Accepted 18 December 2014
Available online 20 March 2015
Metabolic syndrome
Objective: To detect the prevalence of metabolic syndrome (MS) among infertile women with polycystic ovary syndrome (PCOS). Methods: Two hundred and twenty infertile PCOS women were included in this prospective cross section study. Diagnosis of PCOS was based on at least two of ESHRE/ASRM criteria and diagnosis of MS was based on at least three of NCEP ATP III criteria. A standard questionnaire was used to document length of menstrual cycles, personal and family history of medical disorders. Signs of androgen excess and insulin resistance were noted in the physical examination. Anthropometric measurements were done to measure waist circumference, hip circumference and body mass index (BMI) was calculated. Overnight fasting blood sample and a 75 gram oral glucose tolerance test, TSH, prolactin, total testosterone, SHBG and lipid profile levels were evaluated in all studied PCOS women. Trans-vaginal ultrasound was also done to measure; ovarian volume and number of follicles in both ovaries. Results: The prevalence of MS in studied PCOS women was 30.5% (67/220). There is strong positive correlation between prevalence of MS and both age and BMI of the studied PCOS women. Logistic regression analysis showed that; the age > 25 and waist-hip ratio ≥0.85 were powerful predictors for the prevalence of MS in PCOS women. Conclusion: The prevalence of MS was 30.5% in the studied PCOS women. The age above 25 years and waist-hip ratio ≥0.85 were powerful predictors for prevalence of MS in PCOS women.
1. Introduction
Polycystic ovarian syndrome (PCOS) is a complex disorder affects 5%-6% of women during reproductive age group[1]. Based on Rotterdam Criteria; PCOS can be diagnosed by at least two of the three following criteria; clinical and/ or biochemical signs of hyperandrogenism, oligo and/ or annovulation and polycystic ovary on ultrasound, after exclusion of other causes of excess androgen such as adrenal congenital hyperplasia, Cushing’s syndrome and androgen-secreting tumors[2]. Insulin resistance (IR) and compensatory hyperinsulinemia are key pathological factors of PCOS[3]. IR may act directly and/or indirectly to stimulate ovarian androgen production and it plays a pathogenic role in the development metabolic syndrome (MS)[3]. The national cholesterol education program adult treatment panel (NCEP ATP III) guidelines defined the MS as having at least three of the following abnormalities; increased waist circumference, high blood pressure, elevated fasting blood glucose, low serum high-density lipoprotein (HDL) cholesterol and hyperglycemia[4]. Evidence suggests that women with PCOS have an increased risk for developing type II diabetes mellitus and cardiovascular disease[5,6]. This study was designed to detect the prevalence of MS among infertile PCOS women.
2. Materials and methods
2.1. Patients
Two hundred and twenty (220) infertile women with PCOS were included in this prospective cross sectional study which was conducted at Ahmadi Hospital, Kuwait Oil Company (KOC), Kuwait from March 2011 to March 2013 after informed consent and approval of the study by institute ethical committee. Diagnosis of PCOS was based on at least two of European Society for Human Reproduction and Embryology and the American Society for Reproductive Medicine (ESHRE/ASRM) criteria; chronic anovulation, hyperandrogenism and polycystic ovaries, after exclusion of other causes of excess androgen such as adrenal congenital hyperplasia, Cushing’s syndrome and androgensecreting tumors[2]. Oligo-ovulation and/or anovulation was defined by oligomenorrhea (intermenstrual intervals≥35 days) and amenorrhea (intervals >3 months). Clinical hyperandrogenism was defined by presence of hirsutism (Ferriman-Gallwey score of ≥8) and/or acne. Biochemical hyperandrogenism was present if calculated free testosterone level was >2.06%. Polycystic ovary was detected by presence of at least one ovary ≥10 cm3in volume and/or at least one ovary with ≥12 follicles measuring 2-9 mm in diameter by ultrasound[7]. Women with thyroid disorders or hyperprolactinaemia or on steroids or oral contraceptives in the last 3 months were excluded from this study.
Diagnosis of MS was based on at least three of NCEP ATP III criteria; increased waist circumference (>88 cm), low serum HDL cholesterol (<50 mg/dL), hypertriglyceridemia (>150 mg/dL), increased blood pressure (systolic >130 mmHg or diastolic>85 mmHg) and high fasting blood glucose(>110 mg/dL)[8].
A standard questionnaire was used to document length of menstrual cycles, personal, medical and family history of diabetes, hypertension, obesity and ischemic heart disease. Signs of androgen excess (hirsutism, acne, and alopecia) and IR were noted in the physical examination[9]. Anthropometric measurements were done; waist circumference in centimeters measured midway between the upper border of iliac crest & the lower rib margin and hip circumference measured at the level of the greater trochanters. Height was recorded in centimeters and weight in kilograms. BMI was calculated as weight in kilograms divided by the square of height in meters (kg/m2). Overweight was defined; if BMI was between 25.0-29.9 kg/m2, and obese if BMI was ≥ 30.0 kg/m2according to World Health Organization categories. Sitting blood pressure was measured after a 5-min rest using a standard sphygmomanometer[10].
Overnight fasting blood sample and a 75 gram oral glucose tolerance test was obtained in all studied PCOS women. Impaired fasting glucose, impaired glucose tolerance test and diabetes were defined according to American Diabetes Association revised definitions. Thyroid stimulating hormone (TSH), prolactin, total testosterone, sex hormone-binding globulin (SHBG), and a fasting lipid profile (total cholesterol, triglycerides, HDL, and low-density lipoprotein) levels were also evaluated in all studied PCOS women.
Laboratory methods; Total testosterone was measured by a solid-phase competitive chemiluminescent enzyme immunoassay (IMMULITE 2000, Siemens, Eschborn, Germany), SHBG by electrochemiluminescence immunoassay (ECLIA modular analysis E170, Roche Diagnostics, Mannheim, Germany), TSH by two site sandwich immunoassay (ADVIA Centaur, Bayer Corporation, Tarry town, NY, USA), serum prolactin by direct chemiluminometric sandwich method (IMMULITE 2000, Siemens, Eschborn, Germany) and blood glucose by glucose oxidase and peroxidase methods. Triglyceride level was measured by using the standard lipase, glycerokinase, glycerol-3-phosphate oxidase and peroxidase method and HDL cholesterol was measured by the cholesterol esterase, oxidase, peroxidase method. To calculate free testosterone, initially serum albumin, SHBG and total testosterone levels were estimated. Using these values, the free testosterone was calculated by using the free testosterone formula (Free testosterone = 100 × total testosterone /SHBG).
Trans-vaginal ultrasound for both ovaries was done using a vaginal probe of 4-9 MHz of a ultrasound machine (Philips international; Amsterdam; Netherlands) to measure; ovarian volume and number of follicles in both ovaries. The primary outcome of this study measures; the prevalence of MS in infertile PCOS women and secondary outcome measures; factors which may predispose to development of MS[10].
2.2. Sample size and statistics

3. Results
The prevalence of MS in studied PCOS women was 30.5% (67/220). Three features of MS were present in 44 cases (20%), four features in 18 cases (8.2%), and all five features were present in 5 cases (2.3%) of the studied population.
The prevalence of MS was 22.7% in PCOS women ≤ 24 years, 32.1% in PCOS women between 25-29 years, 35.9% in PCOS women between 30-34 years and 100% in PCOS women above 35 years. There is strong positive correlation between prevalence of MS and age of the studied PCOS women, the prevalence of MS increased with increased age of the studied PCOS women (Table 1).

Table 1 Distribution of metabolic syndrome according to age of the studied PCOS women.
77.6% (52/67) of the studied PCOS women with MS presented with primary infertility, 83.6% (56/67) of them had menstrual irregularities in form of oligomenorrhea and/ or amenorrhea. A family history of diabetes mellitus was positive in 38.8% (26/67) of the studied PCOS women with MS, hypertensive disorders was positive in 32.8% (22/67) of the studied PCOS women with MS. Family history obesity was positive in 23.9% (16/67) of the studied PCOS with MS and family history of ischemic heart disease was in 11.9% (8/67) of the studied PCOS women with MS.
There is strong positive correlation between the prevalence of MS and Body Mass Index (BMI) of the studied PCOS women, the Prevalence of MS increased with increased BMI of the studied PCOS women. The prevalence of MS was 22.6% in PCOS women with BMI ≤ 24.9 kg/m2, 34.1% in PCOS women with BMI 25-29.9 kg/m2and 46.9% in PCOS women with BMI ≥30 kg/m2(Table 2).Mean age of studied PCOS women was significantly higher in women with MS than those without MS (30.13 ± 6.52 versus 26.58 ± 5.34) and mean BMI was significantly higher in those with MS than those without MS (29.32 ± 3.30 versus 25.26 ± 2.75) also, the waist–hip ratio was significantly higher in those with MS compared to those without MS (0.87 ± 0.05 versus 0.81+0.05). The free testosterone level was significantly higher in PCOS women with MS compared to women without MS (1.94 ± 0.45 versus 1.76 ± 0.33). The features of hyperandrogenism such as hirsutism with a Ferriman and Gallwey score 8, acne and acanthosis were significantly higher in PCOS women with MS compared to women without MS (32.8% versus 8.5%, 10.4% versus 2.6% and 16.4% versus 3.3%; respectively). Table 3
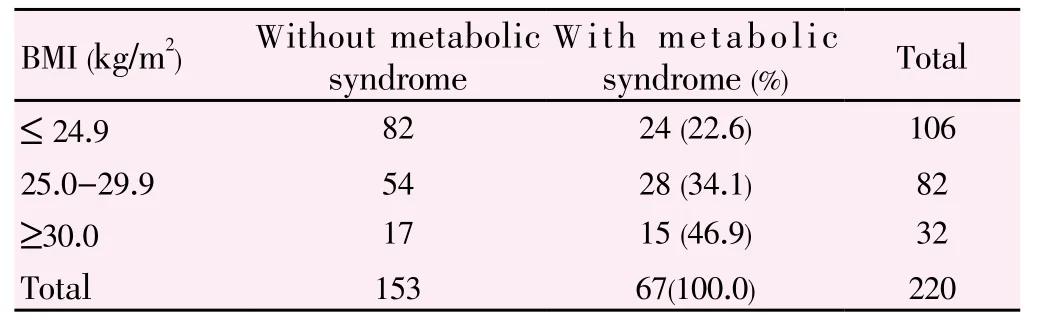
Table 2 Distribution of metabolic syndrome according to Body Mass Index (BMI) of the studied PCOS women.

Table 3 Clinical and biochemical parameters in PCOS women with and without MS.
Logistic regression analysis showed that; the age above 25 years and waist-hip ratio ≥0.85 were powerful predictors for prevalence of MS in PCOS women than other parameters.
4. Discussion
MS is characterized by three main interrelated abnormalities: elevated plasma glucose, dyslipidemia and elevated blood pressure, which directly contribute to a prothrombotic and pro-inflammatory state, predisposing to the development of atherosclerotic cardiovascular disease andtype 2 diabetes mellitus[11]. MS and consequently long-term risk of cardiovascular disease/type 2 diabetes mellitus has been found to be higher in PCOS women compared to non-PCOS women[12,5].
The prevalence of MS in studied PCOS women was 30.5% (67/220 cases). Three features of MS were present in 44 cases (20%), four features in 18 cases (8.2%), and all five features were present in 5 cases (2.3%) of the studied population.
Sixty-nine (69) young women with PCOS and 73 agematched healthy females were evaluated for the occurrence of MS according to the Adult Treatment Panel III by Vrbikova et al. They found that overt MS (the presence of three and more features of MS) was not common in PCOS women (1.6%) than in healthy controls (0%) and they also found isolated features of MS in 50% of PCOS women[13].
Although vrbikova et al concluded that overt Ms was not common in PCOS women, Two hundred and ninety five (295) premenopausal Chinese PCOS women diagnosed by the Rotterdam criteria and 98 control subjects without PCOS were evaluated for prevalence of MS and cardiovascular risk factors by Cheung et al. They found ≥ 3 risk factors of MS in 24.9% of PCOS women compared to 3.1% of controls (using the 2005 modified Adult Treatment Panel III criteria) [14].
Mean age of studied PCOS women was significantly higher in women with MS than those without MS (30.13 ± 6.52 versus 26.58 ± 5.34) and mean BMI was significantly higher in those with MS than those without MS (29.32 ± 3.30 versus 25.26 ± 2.75).
There is strong positive correlation between prevalence of MS and both age and BMI of the studied women, the prevalence of MS increased with increased age and BMI of the studied PCOS women.
Essah and colleagues concluded that the prevalence of MS in PCOS women is high across all age groups[15] and Cheung et al, found that the prevalence of MS in PCOS women increased from 16.7% at age below 30 years to 53.3% at age over 40 years and they also, found that MS was also more prevalent in overweight and obese (41.3%) than normalweight PCOS women (0.9%) [14].
Similar to the results of this study, Hahn et al, found that the prevalence of MS was 33.8% in German PCOS women and they found that the prevalence of MS in German PCOS women increased with obesity and age, also, Soares and colleagues, found that the prevalence of metabolic syndrome increased with increased BMI of Brazilian PCOS women: 3.2%, 19.2%, and 52.3% for normal, overweight, and obese PCOS women, respectively[16,17].
In this study, the waist–hip ratio was significantly higher in those with MS compared to those without MS (0.87 ± 0.05 versus 0.81 ± 0.05) and free testosterone levels were significantly higher in women with PCOS and MS compared to women without MS (1.94 ± 0.45 versus 1.76 ± 0.33). The features of hyperandrogenism such as hirsutism with a Ferriman and Gallwey score ≥ 8, acne and acanthosis were significantly higher in PCOS women with MS compared to women without MS and Logistic regression analysis showed that; the age > 25 and waist-hip ratio ≥ 0.85 were a powerful predictors for the prevalence of MS in PCOS women than the other parameters. Also, Goverde and colleagues, reported that a waist circumference of >83.5 cm along with biochemical evidence of hyperandrogenism were a powerful predictors of the presence of MS and IR in PCOS women [18]. A logistic regression analysis in this study showed that age and central obesity (waist–hip ratio/waist circumference) were powerful predictors of MS in PCOS women compared to other parameters including BMI, also Janssen and colleagues concluded that waist circumference is closely related with obesity-related risk factors as compared with the BMI [19].
The results of this study suggest that PCOS women having any of the following risk factors: age > 25 or with central obesity waist–hip ratio >0.85, are at a greater risk of having MS. However, the results need to be cautiously interpreted because this study was conducted on PCOS women without non-PCOS control group, so, further larger studies with non-PCOS control group will be required for a more accurate estimation of metabolic syndrome prevalence in PCOS women.
The prevalence of metabolic syndrome was 30.5% in the studied PCOS women. There is strong positive correlation between prevalence of MS and both age and BMI of PCOS women. The age above 25 years and waist-hip ratio ≥ 0.85 were powerful predictors for prevalence of MS in PCOS women than other parameters.
Conflict of interest statement
We declare that we have no conflict of interest.
[1] Padubidri VG, Daftary SN. Disorders of the ovary and benign tumours. In: Howkins and Bourne (eds.) Shaws textbook of gynaecology. 15th ed. Haryana: Elsevier Publication; 2011,p. 369-370.
[2] Rotterdam ESHRE/ASRM-Sponsored PCOS Consensus Workshop Group. Revised 2003 consensus on diagnostic criteria and longterm health risks related to polycystic ovary syndrome. Fertil Steril 2004; 81(1): 19-25.
[3] S Asmathulla, Rupa Vani K, Kripa S, Rajarajeswari R. Insulin resistance and its relation to inflammatory status and serum lipids among young women with PCOS. Int J Reprod Contracept Obstet Gynecol 2013; 2(3): 325-329.
[4] Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) final report. Circulation 2002; 106(25): 3143-3421.
[5] Dokras A, Bochner M, Hollinrake E, Markham S, Vanvoorhis B, Jagasia DH. Screening women with polycystic ovary syndrome for metabolic syndrome. Obstet Gynecol 2005; 106(1): 131-137.
[6] Wild S, Pierpoint T, McKeigue P, Jacobs H. Cardiovascular disease in women with polycystic ovary syndrome at long-term followup: a retrospective cohort study. Clin Endocrinol (Oxf) 2000; 52(5): 595-600.
[7] Haffner SM, D’Agostino R Jr., Festa A, Bergman RN, Mykkanen L, Karter A, et al. Low insulin sensitivity [(Si) =0)] in diabetic and nondiabetic subjects in the insulin resistance atherosclerosis study: is it associated with components of the metabolic syndrome and nontraditional risk factors? Diabetes Care 2003; 26(10): 2796-2803.
[8] Lepor NE, Vogel RE. National Cholesterol Education Program Adult Treatment Panel III. Summary of the third report of the National Cholesterol Education Program Adult Treatment Panel III. Rev Cardiovas Med 2001; 2:160-165.
[9] Legro RS, Castracane VD, Kauffman RP. Detecting insulin resistance in polycystic ovary syndrome: purposes and pitfalls. Obstet Gynecol Surv 2004; 59(2): 141-154.
[10] Mandrelle K, Kamath MS, Bondu DJ, Chandy A, Aleyamma TK, George K. Prevalence of metabolic syndrome in women with polycystic ovary syndrome attending an infertility clinic in a tertiary care hospital in south India. J Hum Reprod Sci 2012; 5: 26-31.
[11] Grundy SM, Cleeman JL, Daniels SR, Donato KA, Eckel RH, Franklin BA, et al. American Heart Association; National Heart, Lung, and Blood Institute. Diagnosis and management of the metabolic syndrome: An American Heart Association/National Heart, Lung, and Blood Institute Scientific Statement. Circulation 2005; 112 (17): 2735-2752.
[12] Shroff R, Syrop CH, Davis W, Van Voorhis BJ, Dokras A. Risk of metabolic complications in the new PCOS phenotypes based on the Rotterdam criteria. Fertil Steril 2007; 88(5): 1389-1395.
[13] Vrbíková J, Vondra K, Cibula D, Dvoráková K, Stanická S, Srámková D, et al. Metabolic syndrome in young Czech women with polycystic ovary syndrome. Hum Reprod 2005; 20: 3328-3332.
[14] Cheung LP, Ma RC, Lam PM, Lok IH, Haines CJ, So WY, et al. Cardiovascular risks and metabolic syndrome in Hong Kong Chinese women with polycystic ovary syndrome. Hum Reprod 2008; 23: 1431-1438.
[15] Essah PA, Nestler JE. Metabolic syndrome in women with polycystic ovary syndrome. Fertil Steril 2006; 86 (Suppl 1): S18-19. [16] Hahn S, Tan S, Sack S, Kimmig R, Quadbeck B, Mann K, et al. Prevalence of the metabolic syndrome in German women with polycystic ovary syndrome. Exp Clin Endocrinol Diabetes 2007; 115 (2):130-135.
[17] Soares EM, Azevedo GD, Gadelha RG, Lemos TM, Maranhao TM. Prevalence of the metabolic syndrome and its components in Brazilian women with polycystic ovary syndrome. Fertil Steril 2008; 89(3): 649-655.
[18] Goverde AJ, Van Koert AJ, Eijkemans MJ, Knauff EA, Westerveld HE, Fauser BC, et al. Indicators for metabolic disturbances in anovulatory women with polycystic ovary syndrome diagnosed according to the Rotterdam consensus criteria. Hum Reprod 2009; 24(3): 710-717.
[19] Janssen I, Katzmarzyk PT, Ross R. Waist circumference and not body mass index explains obesity related health risks. Am J Clin Nutr 2004; 79(4): 379-384.
*Corresponding author: Ibrahim A. Abdelazim, Professor of Obstetrics and Gynecology, Ain Shams University, Cairo, Egypt and Ahmadi Hospital, Kuwait Oil Company (KOC), Kuwait.
Tel: (+965) 66551300
Fax: (+965) 23984184
E-mail: dr.ibrahimanwar@gmail.com
Infertile
Polycystic ovary syndrome
杂志排行
Asian Pacific Journal of Reproduction的其它文章
- Molecular dysregulation of renal development: Congenital anomalies of the kidney and urinary tract
- Ovine fetal sex determination using circulating cell-free fetal DNA (ccffDNA) and cervical mucous secretions
- A new treatment for premature ejaculation? Case series for a desensitizing masturbation aid
- Reproductive status of Camelus bactrianus during early breeding season in India
- Effect of frequency of collection on seminal characteristics of White Pekin duck
- Evaluation of norgestomet Crestar® on oestrus synchronization and reproductive performance of dairy cows in Algeria