低切迹解剖锁定钢板治疗成人锁骨中段骨折的临床疗效
2015-06-27敖荣广禹宝庆姜新华叶秀章施继飞许大峰
敖荣广 禹宝庆 姜新华 叶秀章 施继飞 许大峰
低切迹解剖锁定钢板治疗成人锁骨中段骨折的临床疗效
敖荣广 禹宝庆 姜新华 叶秀章 施继飞 许大峰
目的 探讨低切迹解剖锁定钢板治疗成人锁骨中段骨折的临床疗效。 方法 上海市浦东医院骨科于2012年1月至2013年12月采用低切迹解剖锁定钢板治疗38例成人锁骨中段骨折,其中36例获得完整随访资料,男性20例,女性16例;年龄18~60岁,平均38.0岁。结果 36例患者术后获12~16个月随访, 平均14.5个月,手术时间35~65 min,平均45 min,术中出血量25~55 ml,平均35 ml。所有患者切口均一期愈合,未出现伤口感染、血管神经损伤及内固定松动或断裂,5例患者出现钢板顶住皮肤引起的不适(占13.9%)。患者对治疗结果的满意度:完全满意33例,部分满意2例,不满意1例,满意率高达91.7%。末次随访时肩关节Constant评分平均92分(80~94.5分),其中优14例,良1例;DASH评分平均5.5分(1.5~10.0分)。 结论 低切迹解剖锁定钢板治疗明显移位的锁骨中段骨折不仅可以达到良好复位,稳定内固定,而且降低了与内固定相关并发症的发生,是锁骨中段骨折手术治疗的新选择。
解剖锁定钢板;锁骨;骨折;内固定术
锁骨中段骨折是临床上较为常见的一种骨折,手术指征尚存在争议。近年来文献报道[1-2],同保守治疗相比,手术治疗明显移位的锁骨中段骨折具有并发症低(包括有症状的畸形愈合及骨不愈合等)、功能恢复快等优点。但手术内固定物的选择尚存在一定争议,特别是随着患者对外观及功能要求的提高,与内固定物相关的并发症发生率逐渐上升,而低切记解剖锁定钢板从理论上可以一定程度地避免传统锁骨钢板相关的并发症[3-4]。我科自2012年1月至2013年12月采用低切记解剖锁定钢板治疗38例成人锁骨中段骨折,其中36例获得完整随访资料,取得良好疗效,现报道如下。
资 料 与 方 法
一、一般资料
本组患者36例,男性20例,女性16例;年龄18~60岁,平均38.0岁。致伤原因:交通伤9例,摩托车跌伤8例,自行车跌伤8例,运动跌伤6例,其他伤5例。按美国创伤骨科委员会(orthopeadic trauma association,OTA)制订的标准分类:A型8例,B型4例,C型16例。所有患者均在伤后1周内行切开复位低切迹解剖锁定钢板内固定术。
病例纳入标准:(1)明显移位的锁骨中段骨折,短缩>2 cm;(2)有明显成角畸形且有刺破皮肤风险。排除标准:(1)移位<2 cm;(2)无刺破皮肤风险;(3)合并其他部位骨折;(4)锁骨病理性骨折。
二、手术方法
患者在全麻或臂丛加颈丛神经阻滞麻醉下,取沙滩椅位。以骨折端为中心,于锁骨前上方作10~12 cm长切口,逐层切开皮肤及皮下组织,注意保护锁骨上神经分支,暴露骨折端,清除骨折端积血,剥离部分骨膜,用钳子分别夹住两侧锁骨干部进行复位。对于A型骨折,争取解剖复位,如果骨折呈螺旋形或长斜形,复位后可用克氏针临时固定,然后采用低切迹解剖锁定钢板置于锁骨前上方固定(图1)。对于B型骨折,亦争取解剖复位,采用拉力螺钉将蝶形骨块与一侧骨干进行复位固定,将其变成A型骨折,然后采用低切迹解剖锁定钢板置于锁骨前上方固定(图2)。对于C型骨折,不强求解剖复位,关键是纠正短缩及旋转移位,较大的骨块可用拉力螺钉固定,无法固定的骨块采用可吸收线捆扎固定。术中注意保护骨块的血运,钢板每端至少采用3枚螺钉6层皮质固定。
三、术后处理
术后即予患肩三角巾悬吊制动4~6周,鼓励患者进行肘关节的主动功能锻炼,同时肩关节进行钟摆样锻炼;3周后开始行肩关节被动功能锻炼,并逐步进行肩关节主动功能锻炼,增加力量训练。

图1 患者,男性,21岁,摔伤导致左侧锁骨中段骨折,OTA-A型骨折,采用低切迹解剖锁定钢板固定,钢板外侧与锁骨表面不贴服,钢板顶住皮肤引使患者不适
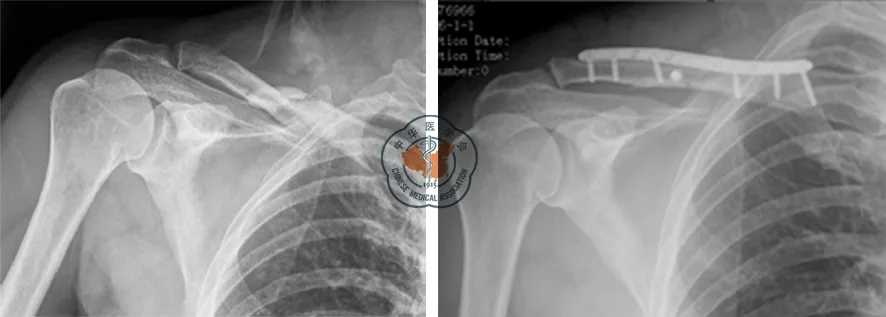
图2 患者,男性,48岁,摔伤导致右侧锁骨中段骨折,OTA-B型骨折,采用低切迹解剖锁定钢板固定
四、疗效评定标准
(1)手术时间和术中出血量;(2)患者对治疗的满意度;(3)并发症的发生情况,包括伤口感染、血管神经损伤及内固定物相关并发症(内固定断裂和内固定激惹皮肤);(4)肩关节功能Constant评分和臂、肩、手功能障碍(disabilites of the arm, shoulder, and hand, DASH)评分。
结 果
36例患者术后获12~16个月(平均14.5个月)随访,2例患者失访。手术时间35~65 min,平均45 min,术中出血量25~55 ml,平均35 ml。所有患者切口均一期愈合,未出现伤口感染及血管神经损伤,未内固定松动物或断裂,5例患者出现钢板顶住皮肤引起的不适(占13.9%),其中1例为钢板近端与锁骨不贴服引起,4例为钢板远端与锁骨不贴服引起。患者对治疗结果的满意度:完全满意33例,部分满意2例,不满意1例,满意率高达91.7%。部分满意的原因是疤痕比较明显,影响美观;不满意的原因是钢板顶住皮肤引起不适,影响日常生活。末次随访时肩关节Constant评分平均为92分(80~94.5分),其中优14例,良1例;DASH评分平均为5.5分(1.5~10.0分)。
讨 论
锁骨骨折临床上十分常见,约占成人骨折的2.6%~4.0%,肩胛带损伤的35%,其中约有80%发生在锁骨中段[5]。传统观点认为,即使是明显移位的中段骨折,也可采用保守治疗。Neer[6]报道保守治疗2 235例锁骨中段骨折,仅3例(0.1%)发生骨不愈合,而行切开复位内固定的45例患者中有2例(4.6%)发生骨不愈合,该结果为保守治疗锁骨中段骨折提供了理论依据。然而Neer报道的患者中,包括部分儿童和移位不大的锁骨骨折,而这些类型骨折保守治疗均有较好的功能结果。文献报道锁骨中段移位性骨折经保守治疗后骨不愈合发生率为15%[7-8];患者对最终治疗结果的不满意率达31%,其中包括有症状的畸形愈合。以往大多认为锁骨骨折畸形愈合仅仅是一种影像学的表现,不需要手术矫正;目前很多学者认为畸形愈合不仅存在影像学表现,而且与远期临床表现密切相关[9]。McKee等[9]认为,保守治疗多年后出现的一些症状,如肩部疼痛、乏力、易疲劳等均因骨折畸形愈合所致。
一、锁骨中段骨折内固定方式
锁骨中段骨折的固定方式包括髓内固定和髓外固定,但内固定物的选择仍存在一定的争议。髓内固定包括Pin钉、钛制弹性髓内钉等,具有手术创伤小,避免损伤锁骨上神经,术后功能恢复快及取出方便等优点[10],但由于锁骨特殊的解剖形态,髓内钉的置入可能存在困难,同时髓内固定装置通常表面光滑,无法对骨折端进行加压而出现内固定漂移是其缺陷。最近文献报道[11]髓内固定的并发症发生率为24%~50%,主要包括皮肤破溃、髓内钉断裂、髓内钉尾部激惹皮肤等。因此,髓内固定主要应用于相对简单的锁骨中段骨折[11-12]。
钢板内固定仍然是锁骨中段骨折手术治疗的最常见方法,具有绝对稳定固定、允许早期活动的优点。目前常用的钢板包括重建钢板、锁定钢板等。重建钢板虽易塑形,但钢板强度不佳,特别是多次塑形后钢板强度下降,容易出现钢板变形或断裂而导致骨折延迟愈合或畸形愈合;而锁定钢板具有成角稳定性高、骨膜剥离范围小、创伤小等优点,有利于减轻疼痛及功能恢复。由于锁骨特殊的解剖形态及其位于皮下的特点,因而对锁骨钢板也有其相应的要求。传统的重建钢板,非解剖锁定钢板,术中需根据锁骨的不同解剖形态进行塑形,耗费手术时间,降低了钢板的强度,同时由于钢板与锁骨表面无法完全贴服,容易出现钢板顶住皮肤引起的不适。
二、低切迹解剖锁定钢板治疗锁骨中段骨折
随着时代的发展,患者对骨折治疗不仅要求恢复功能骨折的连接,同样关注骨折区域的局部感受,由钢板顶住皮肤引起的不适越来越引起国内外学者的重视。由于锁骨位置表浅,目前绝大部分钢板均位于锁骨上方,对于体型偏瘦的患者,特别是女性,可能造成钢板或螺钉顶住皮肤而引起不适,从而降低患者治疗满意度,并要求二次取出内固定。虽然有文献报道前方放置钢板可有效降低内固定对皮肤的激惹,但该方法需剥离三角肌前束来暴露锁骨远端前方骨面,可能会影响肩关节前屈功能。
低切迹解剖锁定钢板可以很好地解决上述问题,该类型钢板依据骨骼的解剖形态设计,具有锁定钢板的优点。一项200例尸体标本的研究表明,绝大多数的锁骨解剖钢板能够与锁骨上方解剖形态匹配[13],因此术中大多不用塑形,可以节省手术时间,减少感染发生,降低钢板因折弯出现疲劳断裂风险,同时该类型钢板具有边缘斜面设计,可以降低对局部皮肤的激惹,减少钢板顶住皮肤引起的不适。同其他非解剖的3.5 mm锁骨钢板相比,生物力学研究显示[14],两者在轴向拉力、压缩及扭转性能方面无明显差异。
文献报道非解剖与低切迹解剖钢板治疗锁骨骨折的结果显示,两者均可实现良好的肩关节功能,较低的骨不愈合发生率及并发症,但在解剖锁定钢板组中钢板顶住皮肤引起不适的发生率更低,内固定再次取出的更少。在一项回顾性研究钢板内固定治疗锁骨中段骨折文献中,15例采用解剖锁定钢板,15例采用非解剖钢板,通过18个月随访,解剖锁定组无内固定取出病例,非解剖钢板组中9例取出钢板(占60%),其中5例因顶住皮肤引起不适,Chandrasenan等[3]认为同非锁定钢板组相比,解剖锁定钢板组对皮肤激惹更少。VanBeek等[4]回顾性比较了42例钢板治疗锁骨中段骨折的病例,28例采用解剖锁定钢板,14例采用非解剖钢板,结果显示两组分别有9例出现钢板顶住皮肤不适,分别占32.1%和64.3%,解剖锁定钢板组在与钢板相关的并发症方面明显低于非解剖钢板组。本组患者我们均采用低切迹解剖锁定钢板于锁骨上方固定,通过患者的主观功能评价,包括肩关节主观功能评分,患者对治疗的满意度及内固定对皮肤的激惹等评价指标,全面评估了患者的主观感受,结合肩关节客观功能评分,全面评估了该类型钢板治疗锁骨中段骨折的疗效。我们发现本组患者与内固定相关的并发症仅为13.9%,比国外文献报道的结果更低,且无内固定断裂。
本组病例均采用低切迹解剖锁定钢板固定,术中注意保护骨折端软组织血供,减少骨膜剥离。对于A型及B型骨折,争取解剖复位,尽量保留蝶形骨块的血运;对于C型骨折,不强求解剖复位,关键是纠正短缩及旋转移位,较大的骨块可用拉力螺钉固定,无法固定的骨块可采用可吸收线捆扎固定。低切迹解剖锁定钢板放置于锁骨上方,骨折端区域无螺钉孔,通过两端各至少3枚螺钉6层皮质固定后,则起到桥接钢板与内固定支架的功能,不仅具有锁骨锁定钢板的一般优点,而且术中不用塑形,可以减少手术时间,有效减少骨折端血供破坏,有利于骨折愈合,同时低切迹的设计可以有效减少钢板对皮肤的激惹,减少钢板顶住皮肤引起的不适。值得注意的是,该类钢板中间一段没有螺孔,因此对于骨折线偏远端的锁骨骨折,锁骨远端难以采用3枚或更多的螺钉固定,因此需慎重使用。对于部分患者,该钢板不一定能与锁骨上方完全匹配,特别是钢板两端部分,这时则需对钢板适当的塑形以防止钢板上翘顶住皮肤,而减少激惹皮肤的风险。在本组患者中,我们发现共有5例患者出现皮肤激惹症状,均由钢板远端或近端与锁骨表面不贴服引起,故术中需加以注意。
本研究结果显示低切迹解剖锁定钢板治疗明显移位的锁骨中段骨折可以达到良好复位,稳定内固定的目的,降低了与内固定相关并发症的发生,提高了患者主观满意度,是锁骨中段骨折手术治疗的新选择。但本文为回顾性研究,样本量小,随访时间短,缺乏前瞻性对比研究,对手术治疗与保守治疗的结果缺少比较,对不同类型的钢板治疗结果缺少比较,故结论尚有一定局限性。
[1] Robinson CM, Court-Brown CM, Mcqueen MM, et al. Estimating the risk of nonunion following nonoperative treatment of a clavicular fracture[J]. J Bone Joint Surg Am, 2004, 86-A(7): 1359-1365.
[2] Zlowodzki M, Zelle BA, Cole PA, et al. Treatment of acute midshaft clavicle fractures: systematic review of 2144 fractures: on behalf of the Evidence-Based Orthopaedic Trauma Working Group[J]. J Orthop Trauma, 2005, 19(7): 504-507.
[3] Chandrasenan J, Espag M, Dias R, et al. The use of anatomic pre-contoured plates in the treatment of mid-shaft clavicle fractures[J]. Injury Extra, 2008, 39(5): 171.
[4] VanBeek C, Boselli KJ, Cadet ER, et al. Precontoured plating of clavicle fractures: decreased hardware-related complications?[J]. Clin Orthop Relat Res, 2011, 469(12): 3337-3343.
[5] Postacchini F, Gumina S, De Santis P, et al. Epidemiology of clavicle fractures[J]. J Shoulder Elbow Surg, 2002, 11(5): 452-456.
[6] Neer CS. Nonunion of the clavide [J]. J Am Med Assoc,1960,172(5):1006-1011.
[7] Hill JM, Mcguire MH, Crosby LA. Closed treatment of displaced middle-third fractures of the clavicle gives poor results[J]. J Bone Joint Surg Br, 1997, 79(4): 537-539.
[8] Nordqvist A, Petersson CJ, Redlund-Johnell I. Mid-clavicle fractures in adults: end result study after conservative treatment[J]. J Orthop Trauma, 1999, 12(8): 572-576.
[9] McKee MD, Wild LM, Schemitsch EH. Midshaft malunions of the clavicle[J]. J Bone Joint Surg Am, 2003, 85(5): 790-797.
[10] Tarng YW, Yang SW, Fang YP, et al. Surgical management of uncomplicated midshaft clavicle fractures: a comparison between Titanium elastic nails and small Reconstruction plates[J]. J Shoulder Elbow Surg, 2012, 21(6): 732-740.
[11] Ferran NA, Hodgson P, Vannet N, et al. Locked intramedullary fixation vs plating for displaced and shortened mid-shaft clavicle fractures: a randomized clinical trial[J]. J Shoulder Elbow Surg, 2010, 19(6): 783-789.
[12] Mueller M, Burger C, Florczyk A, et al. Elastic stable intramedullary nailing of midclavicular fractures in adults: 32 patients followed for 1-5 years[J]. Acta Orthop, 2007, 78(3): 421-423.
[13] Huang JI, Toogood P, Chen MR, et al. Clavicular anatomy and the applicability of precontoured plates[J]. J Bone Joint Surg Am, 2007, 89(10): 2260-2265.
[14] Goswami T, Markert RJ, Anderson CG, et al. Biomechanical evaluation of a pre-contoured clavicle plate[J]. J Shoulder Elbow Surg, 2008, 17(5): 815-818.
(本文编辑:李静)
敖荣广,禹宝庆,姜新华,等.低切迹解剖锁定钢板治疗成人锁骨中段骨折的临床疗效[J/CD]. 中华肩肘外科电子杂志,2015,3(3):141-145.
Analysis on the clinical curative effects of low-profile locking anatomic plate therapy on the middle clavicular fracture of adult
AoRongguang,YuBaoqing,JiangXinhua,YeXiuzhang,ShiJifei,XuDafeng.
DepartmentofOrthopaedics,ShanghaiPudongHospital,Shanghai201200,China
YuBaoqing,Email:doctorybq@163.com;JiangXinhua,Email:doctorjxh@163.com
Background Middle clavicular fracture is a clinically common fracture, and there are still disputes over its operation indications. According to literature reports over recent years, in comparison with conservative treatment, operative treatment on middle clavicular fracture with obvious fracture displacement has lower complications (including symptomatic malunion and bone ununion), faster functional rehabilitation and functional result. However, there are some disputes over the selection of internal fixators during operation. In particular, since the patients have higher requirments for appearance and functions, the occurrence rate of internal fixator relevant complications has been gradually rising. However, theoretically, the clinical curative effects of low-profile locking anatomic plate can avoid the traditional clavicular plate related complications to certain extent. During the period from January 2012 to December 12, our department adopted ow-profile locking anatomic plate in the treatment of 38 adult cases of middle clavicular fracture, obtained integral follow-up data of 36 cases and achieved good curative effects. The specific conditions are hereby reported as follows.Method I. General materials:This groups includes totaled 36 cases(20 male cases and 16 female cases); they are aged 18-60, with an average age of 38.0 years. Injury causes: traffic injury 9 cases, motorcycle falling injury 8 cases, bicycle falling injury 8 cases, exercise falling injury 6 cases and other injury 5 cases. Classification by the standard established by US Orthopaedic Trauma Association (OTA): 8 cases of A type, 4 cases of B type and 16 cases of C type; All the patients
open reduction and internal fixation with low-profile locking anatomic plate in a week after injury. Case inclusion criteria: (1) Middle clavicular fracture with obvious displacement, with shortening >2 cm; has obvious angulation deformity and risk of piercing skin. Case exclusion criteria: (1) Displacement of less than 2 cm; (2) Without risk of piercing skin; (3) Complicated with fractured on other sites; (4) Clavicular pathologic fracture. II. Operative method:Under general anesthesia or brachial plexus combined cervical plexus nerve block anaesthesia, allow the patient to lie on beach chair position; with the fracture end as the center, make incision in length of 10-12 cm at the anterior-superior clavicular, cut open skin and subcutaneous tissues layer by layer, pay attention to the protection of supraclavicular nerve branches, expose the fracture end, remove the aemorrhage at fracture end, strip partial periosteum, and use tongs to respectively clamp the clavicular diaphysis on both sides for fracture reduction. For Type A fracture, try for anatomical reduction. If the fracture presents spiral or long oblique, after reduction use Kirschner wires for temporary fixation and place low-profile locking anatomic plate on the anterior superior clavicular for fixation. For type B fracture, also try for anatomical reduction, adopt lag screws to perform reduction and fixation of butterfly bone blocks with diaphysis on other side, turn it into type A fracture, then place low-profile locking anatomic plate at anterior superior clavicular for fixation. For type C fracture, not try for anatomical reduction, and key measure is to correct shortening and rotation displacement; bigger bone blocks can be fixed by means of lag screws. The bone blocks which cannot be fixed through lag screws can be tied and fixed through absorbable wires. During the operation, pay attention to protecting the blood supply for bone blocks, and adopt at least 3 screws at each end of plate for 6-layer cortex fixation.III. Postoperative treatment:Upon completion of operation, use a piece of triangle bandage to suspend and brake affected shoulder for 4-6 weeks, encourage the patient to perform active functional exercise of elbow joint and perform pendulum exercise of shoulder joint; 3 weeks later, start passive functional exercise of shoulder joint, and gradually perform active functional exercise of shoulder joint and enhance strength training. IV. Evaluation criteria for curative effects: (1)Operation time and intraoperatve blood loss; (2) Patient satisfaction to treatment; (3) Occurrence of complications, including wound infection, vascular nerve injury and internal fixator related complications (internal fixation fracture and skin irritation by internal fixation); (4) Shoulder joint function Constant scoring as well as scoring of disabilities of the arm, shoulder and hand, DASH.Results 36 cases received postoperative follow-up for 12-16 months (14.5 months on average), and 2 cases lost follow-up. The operation time is 35-65 min, with average time being 45 min; the intraoperatve blood loss is 25-55 ml, with average value of 35 ml. All the incisions are healed at phase I, without occurrence of wound infection and vascular nerve injury, without internal fixation loosening or fracture; 5 cases have discomfort caused by plate pressing aginst skin (accounting for 13.9%), in which 3 cases are caused by proximal end of plate not fitting with clavicular, and 2 cases are caused by distal end of plate not fitting with clavicular. The degree of satisfaction of the patients to treatment: 33 cases are completely satisfied with the therapy result, 2 cases are partially satisfied and 1 case is not satisfied, with satisfaction rate as high as 91.7%. The reason for partial satisfactory is that the scar is relatively obvious and may affect esthetic appearance; the cause for dissatisfaction is that the steel plate presses aginst skin, thus causing discomfort and affecting daily life. In final follow-up, Constant score of shoulder joint is 92 points on average(80-94.5 points), including 14 cases with excellent score and 1 case with good score; DASH score is 5.5 points on average(1.5-10.0 points).Conclusion Low-profile locking anatomic plate therapy of middle clavicular fracture with obvious displacement can not only achieve good fracture reduction and stable internal fixation, but also reduce the occurrence of internal fixation related complications. Therefore it is a new option for operative treatment of middle clavicular fracture.
Anatomic locking plate;Clavicular;Fracture;Internal fixation
10.3877/cma.j.issn.2095-5790.2015.03.003
浦东新区卫生系统优秀青年医学人才培养计划(PWRq2014-06);上海市浦东医院“浦菁计划”
201200上海市浦东医院 复旦大学附属浦东医院骨科
禹宝庆,Email:doctorybq@163.com;姜新华,Email:doctorjxh@163.com
2015-04-09)
(PJ201402)
