关节镜下肌腱固定术治疗肱二头肌腱近端病损
2015-06-26高庆峰鄂刚何耀华张尧赵金忠皇甫小桥沈继刘闻欣
高庆峰 鄂刚 何耀华 张尧 赵金忠 皇甫小桥 沈继 刘闻欣
关节镜下肌腱固定术治疗肱二头肌腱近端病损
高庆峰1鄂刚1何耀华2张尧2赵金忠2皇甫小桥2沈继2刘闻欣2
目的 探讨关节镜下通过肌腱固定术治疗肱二头肌腱近端病损的手术方法及临床效果。方法 2010年1月至2012年6月关节镜下通过肌腱固定术治疗肱二头肌腱近端病损49例,患者诊断明确,肱二头肌长头肌腱近端病损为其症状产生的主要原因,其中男性21例,女性28例。年龄37~60岁。分别记录术前及最终随访时疼痛、活动范围、前屈上举肌力以及功能评分,并进行统计学分析。结果 所有患者术程顺利,术后顺利愈合并获随访平均18(12~34)个月。术前Constant评分为平均39.4分,UCLA评分为平均15.4分;术后Constant评分为平均89.1分,UCLA评分为平均31.2分。术后与术前相比,在疼痛、活动范围、屈肘、肌力及功能恢复方面差异均有统计学意义(P<0.05)。结论 关节镜下通过肌腱固定技术治疗肱二头肌腱近端病损的临床效果满意。
肌腱固定术;肩关节;关节镜;带线锚钉
肱二头肌长头腱的近端病损会引起肩关节功能障碍和疼痛[1]。肱二头肌长头腱具有横跨肩关节内外的特殊结构,其近端病损主要包括肱二头肌腱炎、磨损或撕裂、肌腱半脱位以及脱位等[2]。肱二头肌长头腱的近端病损会导致患者肩关节活动范围受限和前臂放射疼痛,严重影响患者的运动功能和生活质量。肱二头肌腱的近端病损一旦确诊通常需要手术治疗。虽然文献报道肌腱固定术和肌腱切断术的治疗效果差异无统计学意义,但很多学者认为<60岁及对功能和外观要求较高的患者适于采用关节镜下肌腱固定术[3-4]。传统的治疗方法为切开肌腱固定术,创伤大,患者康复困难且不易处理关节内的病变[5]。关节镜下肌腱固定术创伤小,患者康复快,容易接受,在发达国家已成为治疗肱二头肌长头腱的近端病损的首选治疗方法,然而国内报道较少。本文着重介绍我科自2010年1月至2012年6月在关节镜下采用缝合锚钉肌腱固定技术治疗肱二头肌腱患者49例的手术方法及临床疗效。
对 象 与 方 法
一、一般资料
纳入标准:患者年龄均<60岁,术前体格检查、X线及MRI检查确诊为肱二头肌腱近端病损,保守治疗无效,肱二头肌腱近端病损为引起患者症状的主要原因。病例排除标准:肩关节其他疾病如神经病变等。本研究纳入的病例为2010年1月至2012年6月采用带线缝合锚钉肌腱固定术治疗肱二头肌腱近端病损的患者49例,其中男性21例,女性28例;其中肱二头肌腱炎39例、撕裂5例、肌腱不稳2例、肌腱炎合并撕裂3例,均无明确外伤史。年龄35~60岁,均获得临床12个月以上随访,平均随访时间18(12~34)个月。
二、手术方法
患者采用侧卧位,患肢外展40°,前屈15°,用大约4 kg重物作患肢纵向的牵引。常规消毒,铺单后作肩关节后侧入路,置入30°关节镜镜头。首先进行术中的探查:肱二头肌腱充血,炎症严重,证实术前诊断明确;肩胛下肌腱完整,盂肱上、中、下韧带存在,肩胛盂唇无撕裂,肩胛盂和肱骨头的软骨无剥脱,肩袖在肱骨的附着处完整。在后侧入路观察下,建立前侧入路,通过前侧入路置入刨削刀头清理关节腔内肌腱周围炎症的滑膜组织,使视野更加清晰。切换入路到肩峰下,清除肩峰下有病变的滑囊组织,并进行肩峰成形术,以增大肩峰下间隙使空间增大暴露肩袖间隙。在后侧入路监视下建立肩峰外侧入路,到此三个主要关节镜入路建立完毕。观察入路和操作入路可以互换。在肩外侧观察入路下找到肩袖间隙,肱二头肌腱就在肩袖间隙下方。在前侧入路置入刨削刀头清理肩袖间隙上方漂浮软组织,以扩大视野方便操作。清理完毕后换用汽化电刀头暴露肱二头肌腱注意不要损伤肩袖组织(图1,2)在暴露过程要切开横韧带。暴露完毕后用器械把肌腱拨开暴露结节间沟(图3)在结节间沟最狭窄处用打磨头稍微打磨暴露新鲜骨床,然后在结节间沟内嵌入两个缝合带线锚钉,两枚锚钉相距大约1~1.5 cm。利用穿线器在前侧入路,使两根PDS线中的一根穿过肌腱,另一根在肌腱下面穿过,将PDS线的一端拴住锚钉的缝合线,然后拉另一端使锚钉的缝合线穿过肌腱,在镜下使用推结器打结(图4,5)。固定完毕后切断肌腱近端,切换入路到关节腔内清除肌腱病变残端(图6),术后闭合切口。
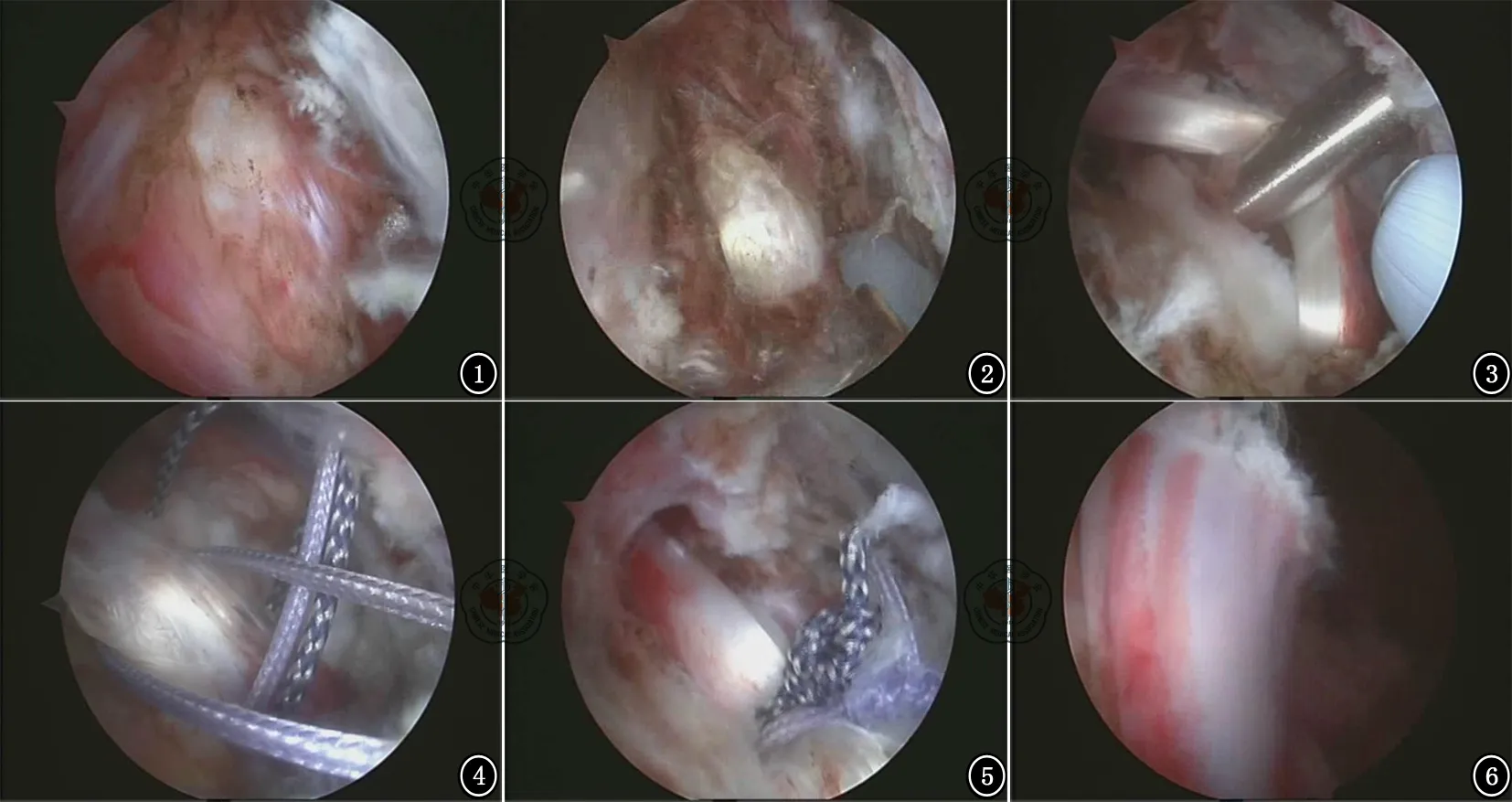
图1肩袖间隙 图2暴露肱二头肌腱 图3暴露结节间沟 图4缝线穿过肌腱 图5打结固定 图6关节内清理肌腱残端
三、术后评估
所有患者的疼痛评估和肩关节活动范围评估包括前屈上举、外旋、内旋,肩关节功能采用Constant-Murley评分[6]和美国加利福尼亚大学洛杉矶分校UCLA(university of California,Los Angeles)评分[7]进行评估。所有患者术后定期随访,术后6周、3个月、6个月及末次随访分别对其疼痛情况、肩关节活动范围、前屈上举的肌力以及功能进行评价,术后MRI复查。
四、术后处理
所有患者术后即刻进行颈腕吊带固定,无痛前提下进行肘、腕及手部的主动活动。禁止主动屈肘6~8周,以使肌腱固定愈合,6~8周后,主动屈肘锻炼慢慢进入康复措施,并强化直至术后3个月,术后3个月开始肌肉力量的恢复训炼。
五、统计学分析

结 果
49例患者术后均顺利康复,术后无感染,无伤口不愈合以及肩关节感觉异常等并发症,术后患者对肩关节功能满意(图7),1例患者因剧烈运动,没有进行预订的康复锻炼,仍存在疼痛。所有患者肘关节屈伸活动满意,肌肉的形状和轮廓与术前无变化,屈肘力量与健侧相比普遍稍微下降但能满足正常生活和运动需要。术前Constant评分为平均39.4分,UCLA评分为平均15.4分;术后Constant评分为平均89.1分,UCLA评分为平均31.2分。术后与术前相比,在疼痛、活动范围、屈肘、肌力及功能恢复方面差异均有统计学意义(P<0.05)。即疼痛、活动范围、屈肘、肌力及功能评分通过关节镜手术治疗差异均有统计学意义(表1,2)。
讨 论
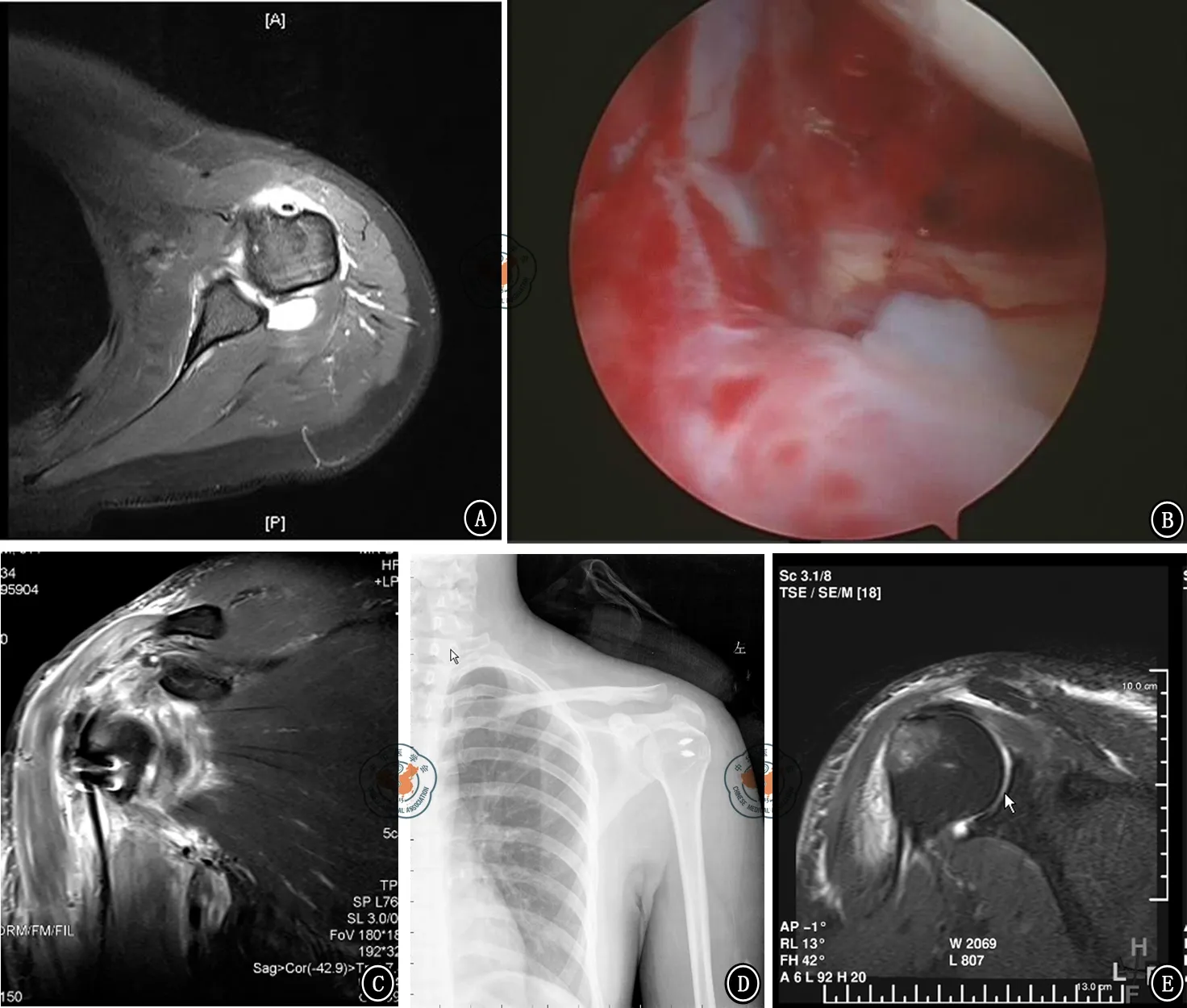
图7男性患者,45岁,外伤至肱二头肌腱长头腱顽固性炎症。A.术前核磁共振显示肱二头肌腱炎;B.术中探查显示肌腱顽固性的炎症;C.术后第1天核磁共振显示固定牢靠;D.术后X线片;E.术后3个月时显示肌腱已经愈合

表1 本组患者术前与末次随访时UCLA评分结果比较±s)

表2 本组患者术前与末次随访时Constant评分结果比较±s)
肱二头肌腱的近端病损经常合并其他肩关节的病变[8]。所以术前应明确肱二头肌腱近端病损为患者症状产生的主要病因。由于肱二头肌腱长头腱存在于肩袖间隙和结节间沟内,所以发生病变的主要原因就是长期的机械性的刺激导致肌腱和横韧带及喙肱韧带的不断摩擦。早期肌腱发生水肿和肌腱的无菌性炎症,随着病情发展肌腱磨损甚至发生断裂,纤维镜下会发现胶原纤维的萎缩,纤维蛋白坏死和大量纤维细胞的增生,至此肌腱病变已不可逆需要手术治疗。患者一般会感到结节间沟区域持续的疼痛和强烈的压痛,也有一部分患者疼痛区域模糊,大部分患者无明确的外伤史。本研究49例患者术前通过体格检查、X线及MRI检查确诊为肱二头肌腱的近端病损,术中关节镜探查证实所有患者术前诊断明确。肌腱固定术治疗肱二头肌腱近端病损取得了令人鼓舞的结果,目的意在重建肱二头肌腱长头肌腱的止点,清除病变肌腱,避免肌腱在结节间沟的摩擦从而达到治疗的目的。许多文献早已经报道了其广泛的手术适应证[9-14]。在本研究中针对以下病变采取了肌腱固定术:(1)肌腱的顽固性炎症,保守治疗无效;(2)肌腱撕裂约超过直径的25%;(3)肌腱完全脱位患者活动障碍;(4)合并肩袖损伤。肌腱切断术虽然简单易行也能减轻患者的疼痛,但肌腱切断术会造成患者肌腱回缩畸形形成“大力水手征”,也有可能造成患者屈肘力量减弱和不明原因的持续性隐痛。本研究患者中年龄均<60岁且对功能美观要求较高,所以均采取肌腱固定术治疗。全关节镜下肌腱固定术是从小切口联合关节镜的术式发展而来,主要是由于操作器械的发展和手术技能的提高。我们采用的是全关节镜下双缝合带线锚钉固定肌腱的方法,带线缝合锚钉可以达到肌腱固定需要的强度。Mazzocca 等[15]分别评估了关节内外的挤压螺钉和缝线锚钉固定肌腱的生物力学测试,结果显示两种固定方法差异无统计学意义。虽然有尸体的生物力学研究显示经骨的挤压螺钉固定要强于带线缝合锚钉的强度[16-17],但是在临床研究中两种固定方式愈后差异无统计学意义[18],而且还有挤压螺钉固定失败的报道[19-20]。采用带线缝合锚钉还有其特定的优点:(1)可以同时缝合撕裂的肩袖,其操作技术及原理也与肩袖缝合相同;(2)在手术过程中使缝线穿过肌腱增加了固定的强度,可以达到早期锻炼的要求;(3)术中应用了双锚钉更增加了固定的强度。术中不需要钻取骨隧道,避免了肩关节后方神经血管的损伤。我们在术中固定肌腱的位置与先前文献报道的近胸大肌止点处1 cm左右的位置非常符合[21-22],近来也被尸体研究所证实此位置可以达到很好的生物力学[23]。
与传统切开手术相比,关节镜下肌腱固定术有许多优点:(1)镜下对肌腱损伤程度可作出较全面、客观、准确的评估;(2)可对盂肱关节腔进行全面检查并可治疗关节内可能联合的损伤与病变;(3)镜下操作避免了三角肌的剥离,对软组织损伤小;(4)术后伤口恢复快,可以进行早期功能锻炼;(5)关节镜为微创手术理论上可以降低血管神经损伤并发症的发生率;(6)术后瘢痕小,肩部较为美观,患者易于接受。关节镜下治疗肱二头肌腱的近端病损的原因分析如下:(1)采用关节镜技术可彻底评估所有病损,在镜下不仅能处理肩峰下问题,而且能同时处理盂肱关节内病变,最大限度缓解疼痛,改善功能;(2)肩峰下间隙广泛的滑膜清扫,尽可能去除所有退变组织,最大限度避免这些退变组织影响治疗效果。缺点为:(1)采用关节镜技术手术难度大,需较长的学习曲线,并需要一些特殊的设备和器械;(2)术中在寻找肱二头肌腱时还要避免损伤肩袖。本研究术中、术后均无明显并发症发生,但手术中应进行控制性降压,尽量保持收缩压在100 mmHg以下,以保持视野清楚。
本研究49例患者通过关节镜下肌腱固定术取得了良好的临床疗效,1例患者术后仍然感觉严重疼痛,可能与此患者依从关系差,没有按照康复计划进行康复,因而疗效较差。然而本研究纳入病例数较少,随访时间较短,长期疗效有待进一步的随访观察。但近期显著的临床效果表明关节镜下采用缝合锚钉固定技术治疗肱二头肌腱近端病损创伤小、恢复快、临床效果满意。总之,关节镜下采用肌腱固定术治疗肱二头肌腱近端病损是一种较为理想的治疗方法。
[1] Alpantaki K,Mclaughlin D,Karagogeos D,et al.Sympathetic and sensory neural elements in the tendon of the long head of the biceps[J].J Bone Joint Surg Am,2005,87(7):1580-1583.
[2] Busconi BB,Deangelis N,Guerrero PE.The proximal biceps tendon:Tricks and pearls[J].Sports Med Arthrosc,2008,16(3):187-194.
[3] Osbahr DC,Diamond AB,Speer KP.The cosmetic appearance of the biceps muscle after long-head tenotomy versus tenodesis[J].Arthroscopy,2002,18(5):483-487.
[4] Patton WC,Mccluskey GM.Biceps tendinitis and subluxation[J].Clin Sports Med,2001,20(3):505-529.
[5] Crenshaw AH,Kilgore WE.Surgical treatment of bicipital tenosynovitis [J].J Bone Joint Surg Am,1966,48(8):1496-1502.
[6] Constant CR,Murley AH.A clinical method of functional assessment of the shoulder[J].Clin Orthop Relat Res,1987(214):160-164.
[7] Ellman H,Hanker G,Bayer M.Repair of the rotator cuff.End-result study of factors influencing Reconstruction[J].J Bone Joint Surg Am,1986,68(8):1136-1144.
[8] Neviaser TJ.The role of the biceps tendon in the impingement syndrome[J].Orthop Clin North Am,1987,18(3):383-386.
[9] Walch G,Nové-Josserand L,Boileau P,et al.Subluxations and dislocations of the tendon of the long head of the biceps[J].J Shoulder Elbow Surg,1998,7(2):100-108.
[10] Pfahler M,Branner S,Refior HJ.The role of the bicipital groove in tendopathy of the long biceps tendon[J].J Shoulder Elbow Surg,1999,8(5):419-424.
[11] Froimson AI,O I.Keyhole tenodesis of biceps origin at the shoulder[J].Clin Orthop Relat Res,1975,(112):245-249.
[12] Dines D,Warren RF,Inglis AE.Surgical treatment of lesions of the long head of the biceps[J].Clin Orthop Relat Res,1982,164:165-171.
[13] Becker DA,Cofield RH.Tenodesis of the long head of the biceps brachii for chronic bicipital tendinitis:long-term results[J].J Bone Joint Surg Am,1989,71(3):376-381.
[14] Berlemann U,Bayley I.Tenodesis of the long head of biceps brachii in the painful shoulder:improving results in the long term[J].J Shoulder Elbow Surg,1995,4(6):429-435.
[15] Mazzocca AD,Bicos J,Santangelo S,et al.The biomechanical evaluation of four fixation techniques for proximal biceps tenodesis[J].Arthroscopy,2005,21(11):1296-1306.
[16] Ozalay M,Akpinar S,Karaeminogullari O,et al.Mechanical strength of four different biceps tenodesis techniques[J].Arthroscopy,2005,21(8):992-998.
[17] Golish SR,Caldwell PE 3rd,Miller MD,et al.Interference screw versus suture anchor fixation for subpectoral tenodesis of the proximal biceps tendon:a cadaveric study[J].Arthroscopy,2008,24(10):1103-1108.
[18] Millett PJ,Sanders B,Gobezie R,et al.Interference screw vs.suture anchor fixation for open subpectoral biceps tenodesis:Does it matter?[J].BMC Musculoskelet Disord,2008,9(1):121.
[19] Nho SJ,Reiff SN,Verma NN,et al.Complications associated with subpectoral biceps tenodesis:Low rates of incidence following surgery[J].J Shoulder Elbow Surg,2010,19(5):764-768.
[20] Koch BS,Burks RT.Failure of biceps tenodesis with interference screw fixation[J].Arthroscopy,2012,28(5):735-740.
[21] Mazzocca AD,Rios CG,Romeo AA,et al.Subpectoral biceps tenodesis with interference screw fixation[J].Arthroscopy,2005,21(7):e1-896.
[22] Provencher MT,LeClere LE,Romeo AA.Subpectoral biceps tenodesis[J].Sports Med Arthrosc,2008,16(3):170-176.
[23] Denard PJ,Dai X,Hanypsiak BT,et al.Anatomy of the biceps tendon:implications for restoring physiological Length-Tension relation during biceps tenodesis with interference screw fixation[J].Arthroscopy,2012,28(10):1352-1358.
(本文编辑:李静)
高庆峰,鄂刚,何耀华,等.关节镜下肌腱固定术治疗肱二头肌腱近端病损[J/CD].中华肩肘外科电子杂志,2015,3(1):24-29.
Arthroscopic tenodesis in the treatment of long head of biceps tendon lesions
GaoQingfeng,EGang,HeYaohua,ZhangYao,ZhaoJinzhong,HuangfuXiaoqiao,ShenJi,LiuWenxin.
DepartmentofOrthopaedics,KailuanGeneralHospital,Tangshan063000,China
HeYaohua,Email:heyaohua@vip.163.com
Background The purpose of this study is to evaluate operative technique and clinical results of Arthroscopic Biceps Tenodesis for proximal lesion of the long head of biceps tendon.Methods Inclusion criteria:patient was younger than 60 years old; confirmed diagnosis of proximal lesion of biceps brachii tendon; conservative treatment was failed; biceps tendon lesion was supposed to be the main cause of shoulder symptoms.Exclusion criteria:other shoulder diseases such as neuropathy.From January 2010 to June 2012,49 patients underwent arthroscopic biceps Tenodesis for proximal lesion of long head of biceps tendon using suture anchor technique.There were 21 males and 28 females.Thirty-nine cases were diagnosed as bicipital tendinitis; 5 cases as tendon tear; 2 cases as biceps tendon instability and tendinitis with tears in 3 cases.Operatiive technique:patients were positioned in lateral decubitus position with 40 degrees of abduction,15 degrees of flexion and 4KG longitudinal traction.The viewing portal was routine posterior portal.Arthroscopic gleno-humeral joint examination was performed.Biceps lesion was confirmed after examination.Anterior working portal was established and debridement was performed if necessary.Then scope was transferred to subacromial space.Anterior lateral portal was then established.Subacromial decompression and anterior acromioplasty was done.Rotator interval was opened to identify biceps tendon.Inter-tuberosity groove was opened along biceps tendon.Two suture anchors were screwed into the narrowest part of the groove.Tenodesis was performed by the two suture anchors.The scope was transferred into joint again and intra-articular part of biceps tendon was removed under direct visualization.The portals were closed routinely.Rehabilitation protocol:all patients were protected in shoulder immobilizer.Pain free range of motion was allowed immediately after operation.Active flexion of elbow was not allowed until 6-8 weeks after operation.Then after,active flexion of elbow began to exercise gradually.Strengthening exercise began from 3 months after operation.Patients were followed up at 6 weeks,3 months,6 months and final review.Pain and range of motion was evaluated at each time.Shoulder function was evaluated according to Constant-Murley score and UCLA score (University of California,Los Angeles score).The preoperative and postoperative scores was analyzed by the paired t test using SPSS 13.0 statistical software,all the data was expressed by Mean ± SD.P<0.05 was statistical significant difference level.Results The mean follow-up time was 18 months (12-34 months).29 patients were well recovered without complications.They were satisfied with their shoulder function.Only 1 patient had residual pain because of uncontrolled active exercise during rehabilitation.All patients were satisfied with their elbow function.No pop-eye deformity was found.The strength of elbow flexion was slightly decreased compared with the healthy side.The preoperative Constant score was 39.4 on average,the average UCLA score was 15.4; after operation,the average Constant score was 89.1,the average UCLA score was 31.2.This means that the arthroscopic biceps tenodesis can improve pain relief,range of motion,elbow flexion,muscle strength,functional score significantly.Conclusion Arthroscopic biceps tenodesis is a convenient technique.Patients suffered from biceps problems can benefit from this procedure.
Biceps tenodesis;Shoulder joint;Arthroscopic;Suture anchors
10.3877/cma.j.issn.2095-5790.2015.01.006
院级特色专业——肩关节运动损伤专科(1687)
063000唐山,开滦总医院骨科1;200233上海交通大学附属第六人民医院关节镜外科2
何耀华,Email:heyaohua@vip.163.com
2014-12-05)
