应用超声技术研究中心静脉穿刺患者颈内静脉与颈总动脉位置关系的影响因素
2015-04-01秦晓辉刘艳红黄连军
秦晓辉,刘艳红,黄连军
解放军总医院 麻醉手术中心,北京 100853
应用超声技术研究中心静脉穿刺患者颈内静脉与颈总动脉位置关系的影响因素
秦晓辉,刘艳红,黄连军
解放军总医院 麻醉手术中心,北京 100853
目的应用超声技术研究中心静脉穿刺患者颈内静脉与颈总动脉位置关系的影响因素,为提高穿刺成功率提供依据。方法于2014年1 - 6月选择我院需要中心静脉穿刺的择期手术患者150例,应用超声波扫描术,在胸锁乳突肌胸骨头与锁骨头顶点位置,头部偏转0°、30°、60°和最大角度,测定不同转头角度双侧颈内静脉与颈总动脉的夹角和动脉重叠率,并分析不同年龄、性别、体质量指数对其的影响。结果超声影像显示,随患者转头角度的增加,颈内静脉从颈总动脉外侧逐渐移向颈总动脉前面,即双侧颈内静脉与颈总动脉的夹角逐渐减小(P<0.01),动脉重叠率逐渐增加(P<0.01)。相同转头角度下,右侧动静脉夹角均大于左侧(P<0.01),而动脉重叠率均小于左侧(P<0.01)。患者头中立位(0°)和转头30°时,女性动脉重叠率大于男性(P<0.05);高龄患者动脉重叠率大于低龄患者(P<0.05);不同转头角度,大体质量指数患者动脉重叠率均大于小体质量指数患者(P<0.05)。结论颈内静脉与颈总动脉的解剖关系随转头角度而发生位置变化,并受年龄、性别和体质量指数的影响。前、中入路穿刺时,转头30°即可;后路穿刺时,尽可能向对侧做最大转头,更易避开动脉。
中心静脉穿刺;颈内静脉;颈总动脉;超声波检查
颈内静脉(the internal jugular vein,IJV)穿刺置管在麻醉科、外科和危重急诊患者救治中已得到广泛应用。颈内静脉穿刺最常见的并发症是误穿颈总动脉(the common carotid artery,CCA)。虽然误穿颈总动脉大多数不会产生严重不良后果,但对于凝血功能障碍的患者有可能有致命的危险[1-2]。超声扫描技术对于颈内静脉定位和指导穿刺非常重要,然而在中国尚不能普及,传统的以解剖标志为依据的盲探穿刺技术仍占主流。尽管颈内静脉与颈总动脉的解剖标志和相互关系早已在教科书和其他文献中有所描述[3-7],但是其位置和相互关系随众多因素而变化,可能导致误穿颈总动脉而产生严重并发症。本文观察、记录了不同转头角度对颈内静脉和颈总动脉位置关系的影响,不同年龄、性别、体质量指数(body mass index,BMI)的患者颈总动脉重叠率的差异,寻找提高穿刺成功率的途径。
对象和方法
1研究对象 随机选择我院2014年1 - 6月根据美国麻醉医师协会病情分级Ⅰ~Ⅱ级,需做中心静脉穿刺置管的择期非心脏手术患者进行前瞻性研究。所有患者术前禁食8 ~ 12 h,去枕平卧,咪唑安定、异丙酚、芬太尼、爱可松麻醉诱导后气管插管,七氟醚、异丙酚、瑞芬太尼静吸复合维持麻醉。机械通气,潮气量8 ml/kg,调整呼吸频率以维持呼气末二氧化碳于30 ~ 40 mmHg(1 mmHg= 0.133 kPa)。排除标准:颈部手术史、头颈部肿物、颈部活动受限的病人。数据收集时,没有病人处于低血压或血流动力学不稳定的状态。
2研究方法 应用便携式超声波扫描仪(iLOOKTM25,Sonosite Company,USA),超声探头垂直皮肤并垂直气管轴,无明显压迫皮肤以维持血管正常的形状和位置。使患者转头角度分别为0°、30°、60°和最大转头角度,测定双侧胸锁乳突肌胸骨头与锁骨头顶点位置颈内静脉与颈总动脉夹角和动脉重叠率,并分组比较不同年龄(≤60岁组和>60岁组)、性别、体质量指数(BMI≤25 kg/m2组和BMI>25 kg/m2组)的患者动静脉位置关系的差异(图1)。动脉重叠率%=[动静脉重叠量(cm)/颈总动脉横径(cm)]×100[8]。所有操作和观察由同一位医生完成。
3统计学方法 应用SPSS17.0统计软件,数据用表示。两组间比较采用t检验;多组间比较采用方差分析并两两比较;转头、性别、年龄、体质量指数等因素与动脉重叠率的相关性采用多元回归分析,P<0.05为差异有统计学意义。
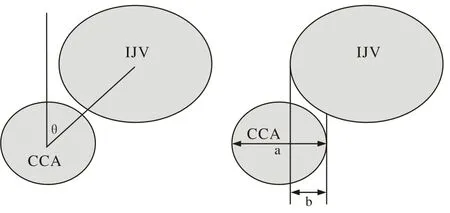
图 1 超声下颈内静脉、颈总动脉测量数据示意图θ=动静脉夹角;a=颈总动脉横径;b=动静脉重叠量Fig. 1 Schematic drawing of relationship between IJV and CCA byultrasonographyθ: the angle between IJV and CCA; a: CCA diameter (mm); b: overlap of CCA and IJV (mm)
结 果
1纳入对象一般情况 本研究共入选150例患者,其中男87例,女63例;年龄18 ~ 82 (53.2±16.8)岁;体质量45 ~ 105 (73±15) kg;身高153 ~ 183 (168± 75) cm;体质量指数16.8 ~ 37.0(26.0±4.8)kg/m2。
2动脉重叠率影响因素的多元回归分析 结果显示,转头角度、性别、年龄和体质量指数是影响动脉重叠率的独立因素。见表1。
3不同转头角度对颈内静脉与颈总动脉解剖关系的影响 胸锁乳突肌胸骨头与锁骨头顶点位置,随患者转头角度的增加,颈内静脉从颈总动脉外侧逐渐移向颈总动脉前面,即双侧颈内静脉与颈总动脉的夹角逐渐减小(P<0.01),动脉重叠率逐渐增加(P<0.01)。相同转头角度下,右侧动静脉夹角均大于左侧(P<0.01),而动脉重叠率均小于左侧(P<0.01)。见表2、表3。
4不同年龄、性别、体质量指数的患者动静脉位置关系的差异 患者头中立位(0°)和转头30°时,女性动脉重叠率大于男性(P<0.05);高龄患者动脉重叠率大于低龄患者(P<0.05);不同转头角度,大BMI患者动脉重叠率大于小BMI患者(P<0.05)。见表4、表5、表6。
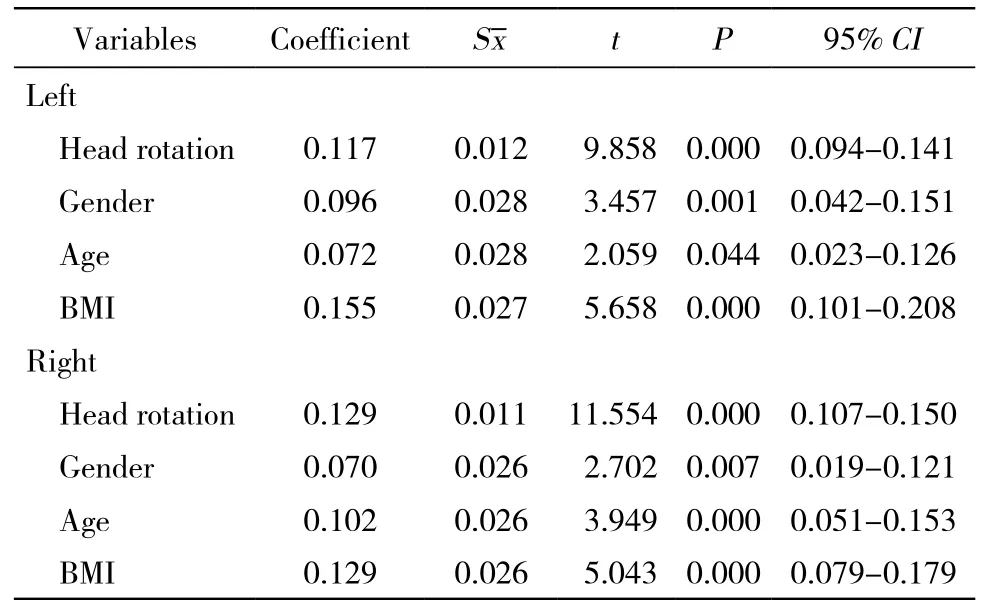
表1 多元回归分析动脉重叠率的独立影响因素Tab. 1 Multivariate regression analysis showing influential factors of CCA overlap
表2 超声下不同转头角度颈内静脉与颈总动脉解剖关系的比较Tab. 2 Effects of head rotation on relationship between IJV and CAA ()

表2 超声下不同转头角度颈内静脉与颈总动脉解剖关系的比较Tab. 2 Effects of head rotation on relationship between IJV and CAA ()
Angle between IJV and CCA (°)Overlap percentage (%) LeftRightPLeftRightP 0°52.2±22.9b63.2±20.3b0.000 32.5±33.3b14.4±26.7b0.000 30°48.9±20.659.5±17.7 0.000 40.7±34.2b23.5±30.7b0.000 60°43.8±23.553.8±19.4 0.000 53.5±35.8a34.6±33.7a0.000 Maximum 31.2±29.1ab45.8±23.5ab0.000 67.4±31.7ab53.5±34.6ab0.000aP<0.05, vs 30° rotation to the same side of the neck;bP<0.05, vs 60° rotation to the same side of the neck Head rotation
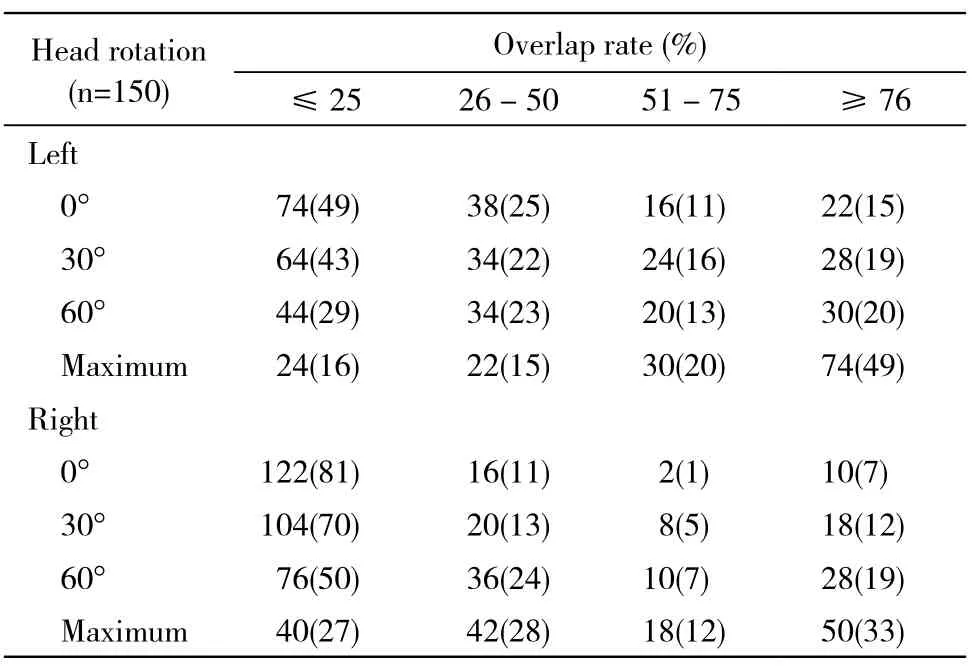
表3 超声下不同动脉重叠率所占人数和比例Tab. 3 Number and percent of patients with different overlap rate of CCA and IJV (n, %)
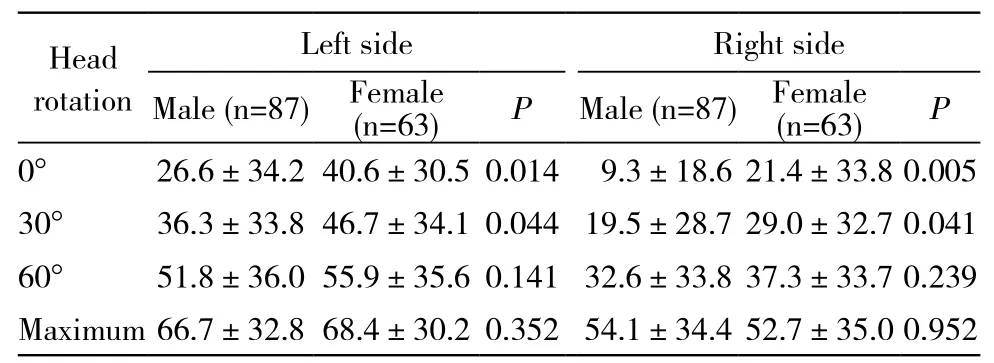
表4 性别与动脉重叠率的关系Tab. 4 Relationship between overlap rate of CCA and gender (%)

表5 年龄与动脉重叠率的关系Tab. 5 Relationship between overlap rate of CCA and age (%)

表6 BMI与动脉重叠率的关系Tab. 6 Relationship between overlap rate of CCA and BMI (%)
讨 论
为提高中心静脉穿刺成功率,减少不良反应的发生,既往对颈内静脉穿刺技术进行了许多研究[7-14]。对于颈部解剖变异和凝血功能障碍的病人,传统的依据外部解剖标志的盲探穿刺技术可能导致严重并发症。虽然误穿颈总动脉的可能性随操作者技术的提高而减小,但这一并发症的风险从未消失。由于超声扫描技术应用于中心静脉穿刺在中国尚未普及,临床实践中行颈内静脉穿刺时,仍多以颈总动脉搏动点或胸锁乳突肌作为标志,因此了解颈内静脉和颈总动脉解剖位置随体位变化及不同人群动静脉位置关系的差异非常重要。
颈内静脉穿刺时将头部偏向对侧可使颈部暴露,方便操作。然而,本实验发现,大多数被检测者头部偏转后,动、静脉的重叠率增加。可能是因为颈内静脉在颈总动脉鞘内,转头引起牵拉作用,使静脉向动脉上方移动,甚至完全覆盖于颈总动脉前面。颈内静脉穿刺时,针尖压迫颈内静脉,使静脉血管塌陷,针尖穿透颈内静脉血管后壁,而不是直接进入血管腔,这种情况发生率报道占50%[15]。当动静脉重叠时,针尖就可能误穿颈总动脉。因此,根据本实验结果,我们推荐:前、中入路穿刺时,尽量避免转头角度过大,转头30°即可,保持动静脉呈平行位置,以减小误穿颈总动脉的可能;颈内静脉后路穿刺时,穿刺针与胸锁乳突肌后缘成15° ~ 30°角,指向胸骨结节,尽可能向对侧做最大转头,使动静脉呈上下关系,更易避开动脉。由于右侧颈内静脉、无名静脉、上腔静脉几乎成一条直线,左侧有胸导管且胸膜顶较右侧高。此外,本组结果显示,颈内静脉和颈总动脉夹角右侧大于左侧,动脉重叠率右侧小于左侧。以上均表明从右侧颈内静脉穿刺置管相对左侧更安全。患者转头0°和30°时,男性颈总动脉重叠率小于女性,这可能就是Schummer等[16]发现在中心静脉穿刺中,男性穿刺失败率较女性低的原因之一。本实验与以往的研究[7]均显示,老年患者动脉重叠率增加,可能与老年人动脉粥样硬化、高血压、血管弹性差导致颈总动脉扩张、伸长和纡曲且颈内静脉内径增粗有关。本研究发现,肥胖患者动脉重叠率增加,与Lieberman等[17]和Fujiki等[18]报道的结果一致。此外,肥胖者因体表解剖标志不清,胸锁乳突肌三角及颈总动脉搏动较难摸清楚,颈内静脉穿刺成功率较低,并发症增多,应避免同一入路反复穿刺。
总之,超声扫描技术对于颈内静脉定位和指导穿刺非常重要,然而在中国尚不普及,特别是在急诊或床旁需做中心静脉穿刺时,传统的以解剖标志和颈总动脉搏动为依据的盲探穿刺技术仍占主流。对颈内静脉和颈总动脉解剖位置和关系多变性的掌握有助于临床医生的操作,减少并发症的发生。
1 Lorchirachoonkul T, Ti LK, Manohara S, et al. Anatomical variations of the internal jugular vein: implications for successful cannulation and risk of carotid artery puncture[J]. Singapore Med J, 2012, 53(5):325-328.
2 Domino KB, Bowdle TA, Posner KL, et al. Injuries and liability related to central vascular catheters: a closed claims analysis[J]. Anesthesiology, 2004, 100(6): 1411-1418.
3 Saitoh T, Satoh H, Kumazawa A, et al. Ultrasound analysis of the relationship between right internal jugular vein and common carotid artery in the left head-rotation and head-flexion position[J]. Heart Vessels, 2013, 28(5): 620-625.
4 Bellazzini MA, Rankin PM, Gangnon RE. Ultrasound validation of maneuvers to increase internal jugular vein cross-sectional area and decrease compressibility[J]. Am J Emerg Med, 2009, 27(4):454-459.
5 Turba UC, Uflacker R, Hannegan C, et al. Anatomic relationship of the internal jugular vein and the common carotid artery applied to percutaneous transjugular procedures[J]. Cardiovasc Intervent Radiol, 2005, 28(3): 303-306.
6 Asouhidou I, Natsis K, Asteri T, et al. Anatomical variation of left internal jugular vein: clinical significance for an anaesthesiologist[J]. Eur J Anaesthesiol, 2008, 25(4): 314-318.
7 Qin XH, Zhang H, Mi WD. Anatomic relationship of the internal jugular vein and the common carotid artery in Chinese people[J]. Chin Med J (Engl), 2010, 123(22):3226-3230.
8 秦晓辉,张宏,米卫东.不同穿刺点颈内静脉和颈总动脉解剖关系变化的研究[J].北京医学,2013,35(8):657-660.
9 Rando K, Castelli J, Pratt JP, et al. Ultrasound-guided internal jugular vein catheterization: a randomized controlled trial[J]. Heart Lung Vessel, 2014, 6(1):13-23.
10 P Souza Neto E, Grousson S, Duflo F, et al. Ultrasonographic anatomic variations of the major veins in paediatric patients[J]. Br J Anaesth, 2014, 112(5):879-884.
11 Ray BR, Mohan VK, Kashyap L, et al. Internal jugular vein cannulation: A comparison of three techniques[J]. J Anaesthesiol Clin Pharmacol, 2013, 29(3): 367-371.
12 Ozbek S, Apiliogullari S, Kıvrak AS, et al. Relationship between the right internal jugular vein and carotid artery at ipsilateral head rotation[J]. Ren Fail, 2013, 35(5):761-765.
13 Chang WK, Wang YC, Ting CK, et al. Optimal shoulder roll height for internal jugular venous cannulation: a study of awake adult volunteers[J]. J Clin Anesth, 2012, 24(3): 179-184.
14 Maecken T, Marcon C, Bomas S, et al. Relationship of the internal jugular vein to the common carotid artery: implications for ultrasound-guided vascular access[J]. Eur J Anaesthesiol, 2011,28(5): 351-355.
15 Keenan SP. Use of ultrasound to place central lines[J]. J Crit Care,2002, 17(2):126-137.
16 Schummer W, Schummer C, Rose N, et al. Mechanical complications and malpositions of central venous cannulations by experienced operators. A prospective study of 1794 catheterizations in critically ill patients[J]. Intensive Care Med, 2007, 33(6): 1055-1059.
17 Lieberman JA, Williams KA, Rosenberg AL. Optimal head rotation for internal jugular vein cannulation when relying on external landmarks[J]. Anesth Analg, 2004, 99(4): 982-988.
18 Fujiki M, Guta CG, Lemmens HJ. Is it more difficult to cannulate the right internal jugular vein in morbidly obese patients than in nonobese patients?[J]. Obes Surg, 2008, 18(9): 1157-1159.
Influential factors of relationship between internal jugular vein and common carotid artery: An ultrasonic study on central venous access
QIN Xiaohui, LIU Yanhong, HUANG Lianjun
Anesthesia and Operation Center, Chinese PLA General Hospital, Beijing 100853, China
ObjectiveTo evaluate the influential factors of relationship between internal jugular vein (IJV) and common carotid artery (CCA) by ultrasonography in order to increase the success rate of puncture.MethodsOne hundred and fifty elective surgical patients in our hospital from January to June in 2014 who required central venous access were included in this study. The angle between IJV and CCA and the overlap of CCA at the apex of triangle formed by sternocleidomastoid muscle at 0°, 30°, 60° and maximum head rotation were analyzed by ultrasonography. The effects of age, gender and body mass index (BMI) on the CCA overlap were also analyzed.ResultsWith the increased head rotation, the IJV moved from the lateral to the front of CCA, so the angle between IJV and CCA became smaller (P<0.01) and the percent overlap of CCA and IJV were gradually increased at both sides (P<0.01). Compared with the left side at the same degree of head rotation, the angle between IJV and CCA was greater and the percent overlap of CCA was lower on the right side (P<0.01). Female and elderly patients were associated with more overlap of CCA at head rotations of 0° or 30° (P<0.05). The overlap rate of CCA in high BMI patients at any head rotations were higher than that of low BMI patients (P<0.05).ConclusionThe relationship between IJV and CCA changes with head rotation and is easily influenced by age, gender and BMI. Head rotation should be limited to 30° when using the anterior or central approach and head should be rotated to maximum degree when using posterior approach in order to avoid inadvertent puncture of CCA.
central venous catheterization; internal jugular vein; common carotid artery; ultrasonography
R 323.1
A
2095-5227(2015)05-0466-04
10.3969/j.issn.2095-5227.2015.05.016
时间:2015-02-13 10:02
http://www.cnki.net/kcms/detail/11.3275.R.20150213.1002.003.html
2014-10-22
秦晓辉,女,博士,副主任医师。研究方向:麻醉基础与临床。Email: qxh301@126.com
The first author: QIN Xiaohui. Email:qxh301@126.com