Continuous regional arterial infusion for the treatment of severe acute pancreatitis: a meta-analysis
2015-02-07
Chengdu, China
Continuous regional arterial infusion for the treatment of severe acute pancreatitis: a meta-analysis
Feng-Jiao Yong, Xuan-Yue Mao, Li-Hui Deng, Ming-Ming Zhang and Qing Xia
Chengdu, China
BACKGROUND:Continuous regional arterial infusion (CRAI) is a drug delivery system, which dramatically increases the drug concentration in the pancreas. Previous clinical and basic studies have demonstrated the possible therapeutic effcacy of CRAI for severe acute pancreatitis (SAP). This meta-analysis of all published randomized controlled trials (RCTs) was conducted to assess the effcacy and safety of CRAI for the treatment of SAP.
DATA SOURCES:Up to August 10, 2014, RCTs comparing CRAI with intravenous infusion for SAP in PubMed, Embase, EBSCO, MEDLINE, Science Citation Index Expanded, Cochrane Library, China Academic Journals Full-Text Database, Chinese Biomedical Literature Database, and Chinese Scientifc Journals Database were selected by two independent reviewers. The relative risk (RR) and their 95% confdence intervals (CI) for duration of elevated serum amylase and urine amylase, duration of abdominal pain, infection rate, incidence of complication, overall mortality, curative rate, hospital stay and details of subgroup analysis were extracted. Meta-analyses were made using the software Review Manager (RevMan version 5.10).
RESULTS:Six RCTs with 390 patients meeting the inclusion criteria were included in the fnal analysis. Compared with intravenous infusion route, CRAI signifcantly shortened the duration of elevated urine amylase (MD=-2.40, 95% CI=-3.20, -1.60;P<0.00001) and the duration of abdominal pain (MD=-1.46, 95% CI=-1.94, -0.98;P<0.00001), decreased the incidence of complication (RR=0.35, 95% CI=0.15, 0.81;P=0.01) and overall mortality (RR=0.25, 95% CI=0.08, 0.78;P=0.02), shortened the duration of hospital stay (MD=-10.36, 95% CI=-17.05, -3.68;P=0.002), and increased the curative rate (RR=1.66, 95% CI=1.13, 2.46;P=0.01). No mortality and catheter-related infections due to CRAI administration was reported in these studies. Subgroup analysis showed that the combination of drug administration via CRAI did not signifcantly improve the outcomes.
CONCLUSION:CRAI is effective for the treatment of SAP, and the combination of drug administration via CRAI did not have a signifcant effect on the improvement of the outcomes.
(Hepatobiliary Pancreat Dis Int 2015;14:10-17)
severe acute pancreatitis; continuous regional arterial infusion; meta-analysis
Introduction
Acute pancreatitis (AP) is the infammation of the exocrine pancreas. There is no specifc treatment for this common abdominal emergency. In 80% of AP patients, pancreatic injury is mild and self-limiting, requiring only brief hospitalization. The remaining 20% develop to have severe acute pancreatitis (SAP) with a mortality varying from 7% to 50%.[1-3]Despite efforts and rapid progress in treatment measurements, the mortality of SAP has not substantially changed during the past two decades.
Continuous regional arterial infusion (CRAI) was initially reported in Japanese clinical trials in 1996.[4]It is a drug delivery system which dramatically increases the drug concentration in the pancreas by using a catheter placed in one of the arteries supplying the infamed pancreas. The catheter used for CRAI was the same as the one used for angiography. The catheter tip was located in the artery perfusion area containing the main lesion of hypoperfusion of the pancreas. Protease inhibitor (PI), antibiotics (A) and microcirculatory promoters (MP) are three categories of agents commonly used inCRAI. A series of clinical and basic studies found that CRAI relieved symptoms, reduced laboratory indicators earlier, decreased mortality, prevented septic complications and shortened hospital stay in SAP,[5-9]especially when applied within 72 hours from the onset of SAP.[10]But the study of Hamada et al[11]showed that CRAI was not effective in reducing in-hospital mortality rate in AP patients, and was associated with longer hospital stay and higher costs. In a study, adverse reactions of CRAI was also reported,[12]such as hyperkalemia, temporary arterial vasospasm and puncture bleeding. So the effcacy and safety of CRAI for SAP have not been determined. A rigorous evidence-based assessment of CRAI for SAP is necessary. Therefore, in this study we made a meta-analysis to evaluate the effcacy of CRAI for the treatment of SAP.
Methods
Literature search
Up to August 10, 2014, a comprehensive literature search was conducted in PubMed, Embase, EBSCO, MEDLINE, Science Citation Index Expanded, Cochrane Library, China Academic Journals Full-Text Database, Chinese Biomedical Literature Database, and Chinese Scientifc Journals Database. MeSH terms and key words used to identify relevant articles included (“pancreatitis“ OR“pancreatitis, acute necrotizing“ OR “pancreatitis, alcoholic“) AND (“arterial infusion“ OR “infusion, intra-arterial“ OR “arterial perfusion“ OR “continuous regional artery infusion“ OR “CRAI“). No language restriction was imposed. Relevant papers were also identifed from the bibliographies of papers obtained through the search.
Two reviewers (Yong FJ and Mao XY) independently selected the articles initially based on titles, key words and abstracts. Studies that did not meet the inclusion criteria were discarded during the initial review. When uncertainty existed, we retrieved and assessed the full-text article. Any disagreements were resolved through discussion or consultation with the third and fourth author (Deng LH and Zhang MM) to reach a consensus. When published data were insuffcient, we contacted the authors.
Inclusion criteria
Studies included in this meta-analysis had to meet the following criteria: (1) study design: randomized controlled clinical trials; (2) study population: patients were confrmatively diagnosed by SAP; (3) intervention: protease inhibitor, antibiotics, and microcirculatory promoters via CRAI versus intravenous infusion (IV) route.
Exclusion criteria
The following studies were not considered for metaanalysis: (1) abstracts, letters, editorials, expert opinions, reviews, and case reports; (2) non-randomized studies; (3) improper outcome measures.
Outcome of interest
The primary outcomes covered duration of elevated serum amylase and urine amylase, infection rate, overall mortality, and duration of hospital stay. Secondary outcome measures were duration of abdominal pain, the incidence of complications, and curative rate.
Data extraction and quality assessment
Two reviewers (Yong FJ and Mao XY) independently extracted information using data extraction form, crosschecked extracted data, and independently assessed quality of the included studies according to theCochrane Handbook for Systematic Reviews of Interventions.[13]
Statistical analysis
Data analysis was made using RevMan 5.10 software. The statistical method referred to theCochrane Handbook for Systematic Reviews of Interventions. The heterogeneity between studies was examined using the Chi-square test and defned at aPvalue less than 0.05. If the test rejected the assumption of homogeneity of studies, then a random-effects analysis was performed. The pooled outcomes are shown in a forest plot and reported as a Mantel-Haenszel relative risk (RR) with a 95% confdence interval (CI). For continuous variables, mean differences (MDs) were calculated with 95% CIs.Ztest was used for the overall effect of RRs and MDs, and aPvalue less than 0.05 was considered statistically signifcant.
Results
Literature selection and characteristics of the studiesFig. 1 shows the process of literature selection using Preferred Reporting Items for Systematic reviews and Meta-Analyses (PRISMA criteria). The initial searching identifed 1743 articles, 1429 of which were excluded for the duplicated studies and irrelevant studies. After reading the abstracts, we excluded 233 non-clinical trials or animal experiment. Among 81 clinical trials for full-text retrieving, 75 did not meet the inclusion criteria or published in local journals (not domestic core journals) were excluded. A total of 6 RCTs were included.[14-19]
Basic characteristics of the included studies are shown in Table 1. A total of 390 patients were enrolled, 203 of which were given CRAI and 187 received IV administration. The administration strategies were PI alone, and the combined use of PI+A, or PI+A+MP. The timing of CRAIapplication varied from 72 hours to 7 days after the onset of pancreatitis.[15,18,19]One study[16]reported CRAI was conducted within 6 hours after the diagnosis, and 2 studies[14,17]did not mention the timing of CRAI application.
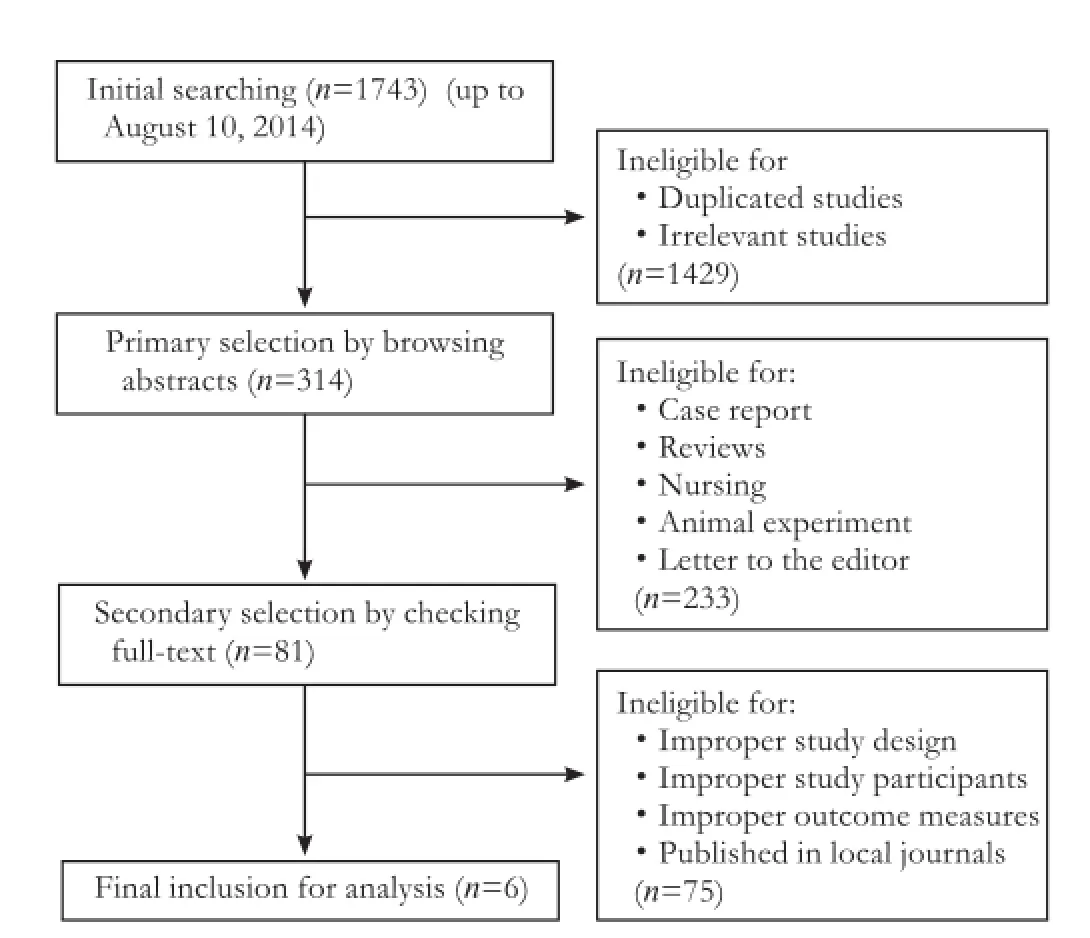
Fig. 1.Flowchart for literature selection.
The quality of the included studies is shown in Table 2. All the included studies mentioned “random“, “randomized“ or “randomization“. Only two studies, however, described the methods of randomization in detail.[14,18]No details of allocation concealment and blinding were reported. One study reported the loss of follow-up.[16]Another study[15]conducted intention-to-treat analysis. There was no selective outcome reporting bias in all studies.
Meta-analysis results
The meta-analysis results of the primary outcomes are shown in Table 3. Two studies reported the duration of elevated serum amylase.[14,17]Subgroup analysis showed that both PI (MD=-0.80; 95% CI=-1.43, -0.17;P=0.01) and PI+A+MP strategy (MD=-2.50; 95% CI=-3.19, -1.81;P<0.00001) shortened the duration of elevated serum amylase. But the test for overall effect (random-effect model meta-analysis) showed that the duration of elevated serum amylase of the CRAI group was not signifcantly shortened compared with the IV group (MD=-1.64; 95% CI=-3.31, 0.02;P=0.05) (Fig. 2).
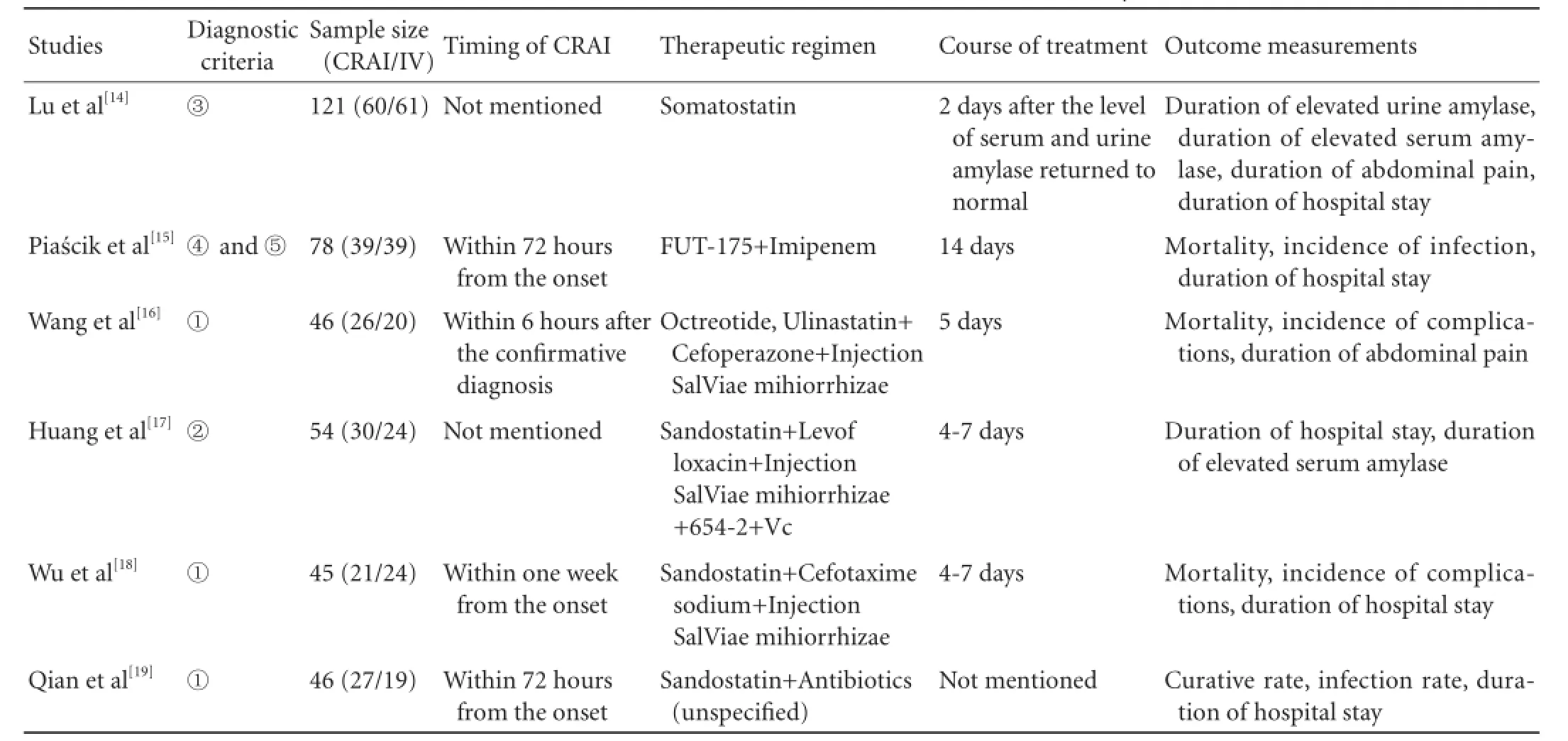
Table 1.Characteristics of the studies included in this meta-analysis
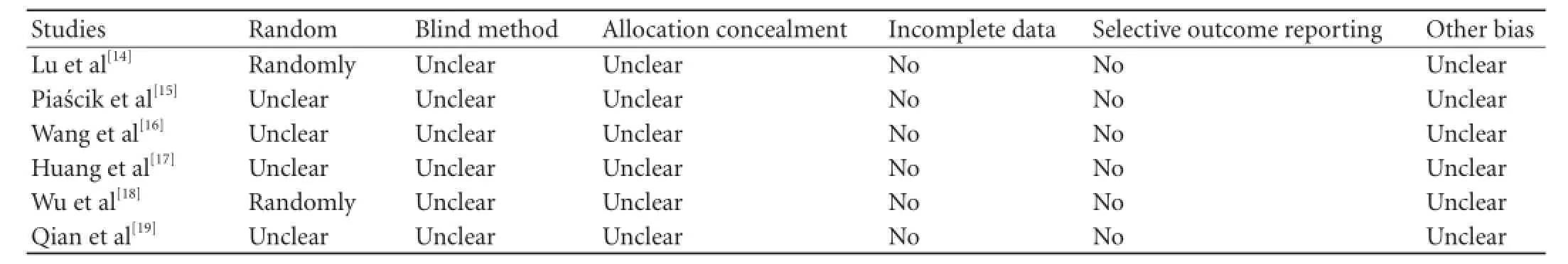
Table 2.Quality assessment of the studies included in this meta-analysis
The infection rate was reported in 2 studies.[15,19]The overall incidence of infection was 30.3% (20/66) in the CRAI group and 50% (29/58) in the IV group. There was heterogeneity among the 2 studies (P=0.05;I2=74%). Results of random-effect model meta-analysis showed that the overall infection rate in the CRAI group was not signifcantly different from that in the IV group (RR=0.53, 95% CI=0.18, 1.56;P=0.25) (Fig. 3).
The pooled outcomes of mortality are shown in Fig. 4 as forest plots and reported as a Mantel-Haenszel RR with a 95% CI. Three studies[15,16,18]reported mortality. The overall mortality was 3.5% (3/86) in the CRAI group and 15.7% (13/83) in the IV group. There was no heterogeneity among the studies (P=0.92;I2=0%). Fixed-effect model meta-analysis showed that the overall mortality ofthe CRAI group was signifcantly lower than that of the IV group (RR=0.25, 95% CI=0.08, 0.78;P=0.02). The results of subgroup analysis showed that mortality was signifcantly reduced by PI+A strategy (RR=0.22; 95% CI 0.05, 0.96;P=0.04), but not PI+A+MP strategy (RR=0.30; 95% CI=0.05, 1.91;P=0.20).
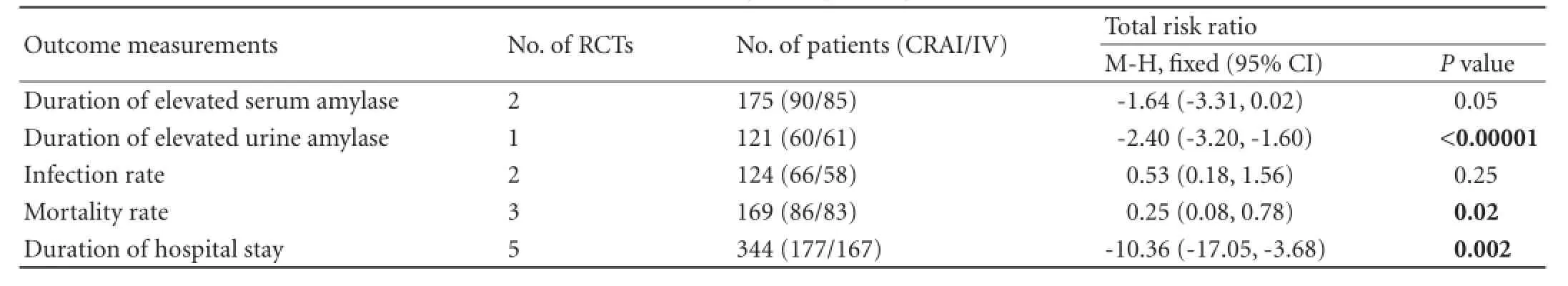
Table 3.Meta-analysis of primary outcomes
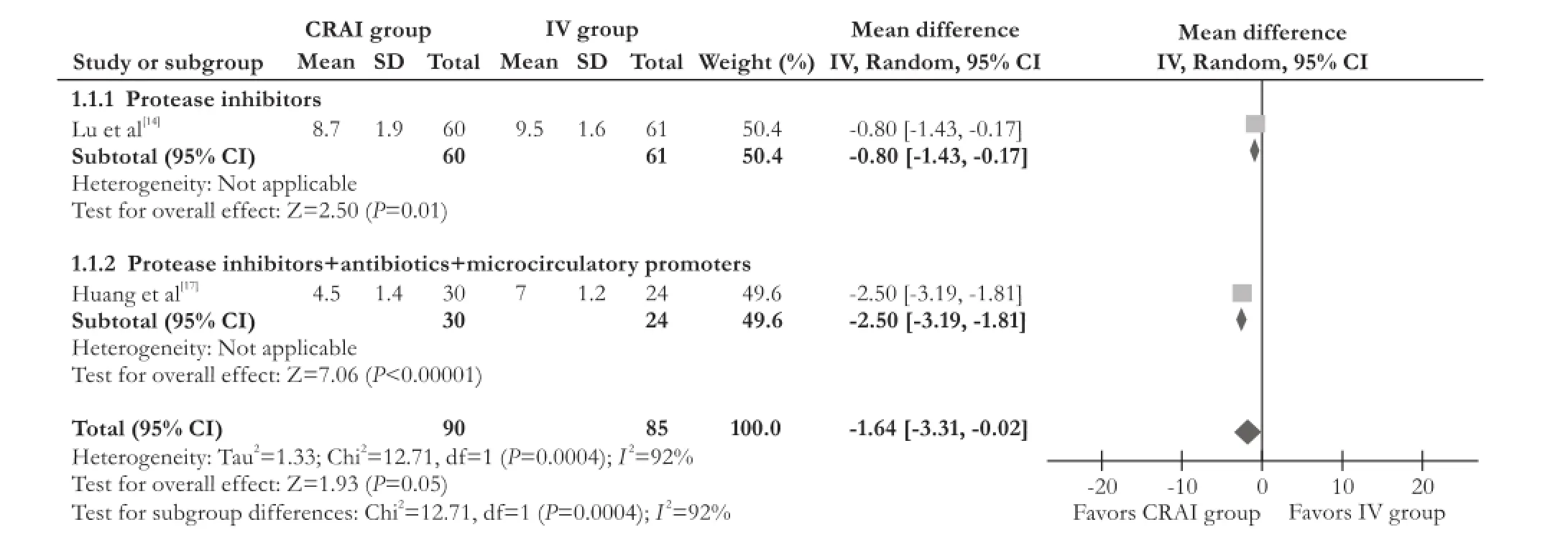
Fig. 2.Forest plot showed that compared with the IV group, the duration of elevated serum amylase of the CRAI group was not signifcantly shortened. CRAI: continuous regional arterial infusion; IV: intravenous infusion.
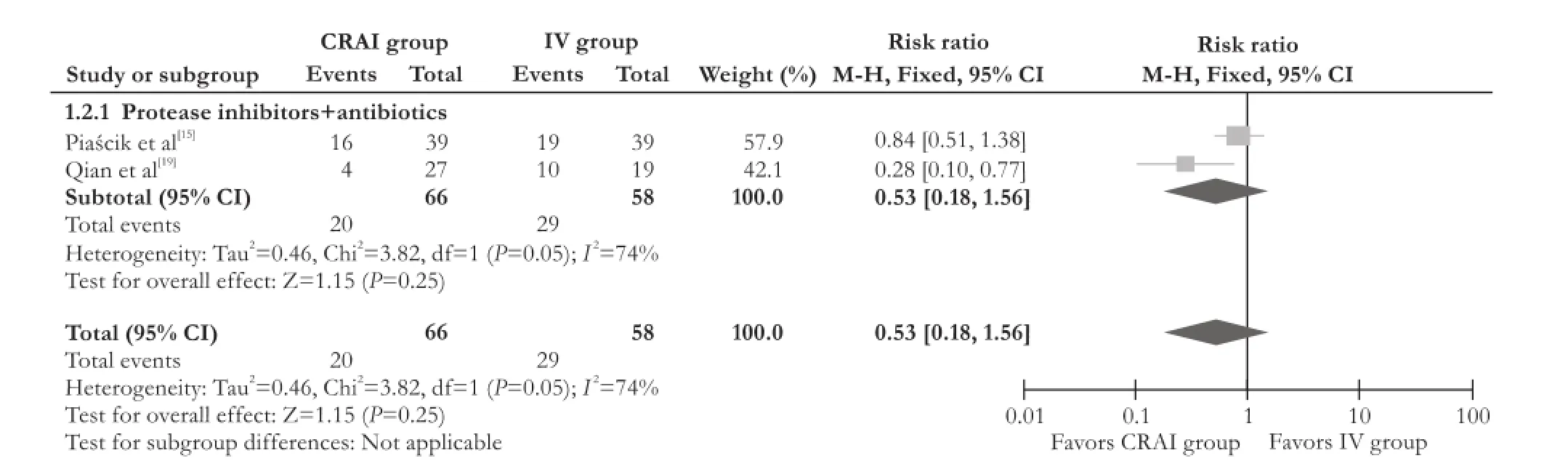
Fig. 3.Forest plot showed that compared with the IV group, the infection rate in the CRAI group was not signifcantly decreased. CRAI: continuous regional arterial infusion; IV: intravenous infusion.
The duration of hospital stay was evaluated in the pooled 5 studies.[14,15,17-19]The heterogeneity among these studies was signifcant (P<0.00001,I2=98%), therefore the data were analyzed by a random-effect model. The duration of hospital stay of the CRAI group was shortened by 10.36 days in the CRAI group compared with the IV group [MD=10.36, 95 % CI=-17.05, -3.68;P=0.002). Subgroup analysis showed that the duration of hospital stay was shortened by PI strategy (MD=-11.00; 95% CI=-12.71, -9.29;P<0.00001). PI+A strategy (MD=-7.67, 95% CI=-20.89, 5.54;P=0.26) and PI+A+MP strategy (MD=-15.00, 95% CI=-41.44, 11.44;P=0.27) could not statistically reduce the duration of hospital stay (Fig. 5).
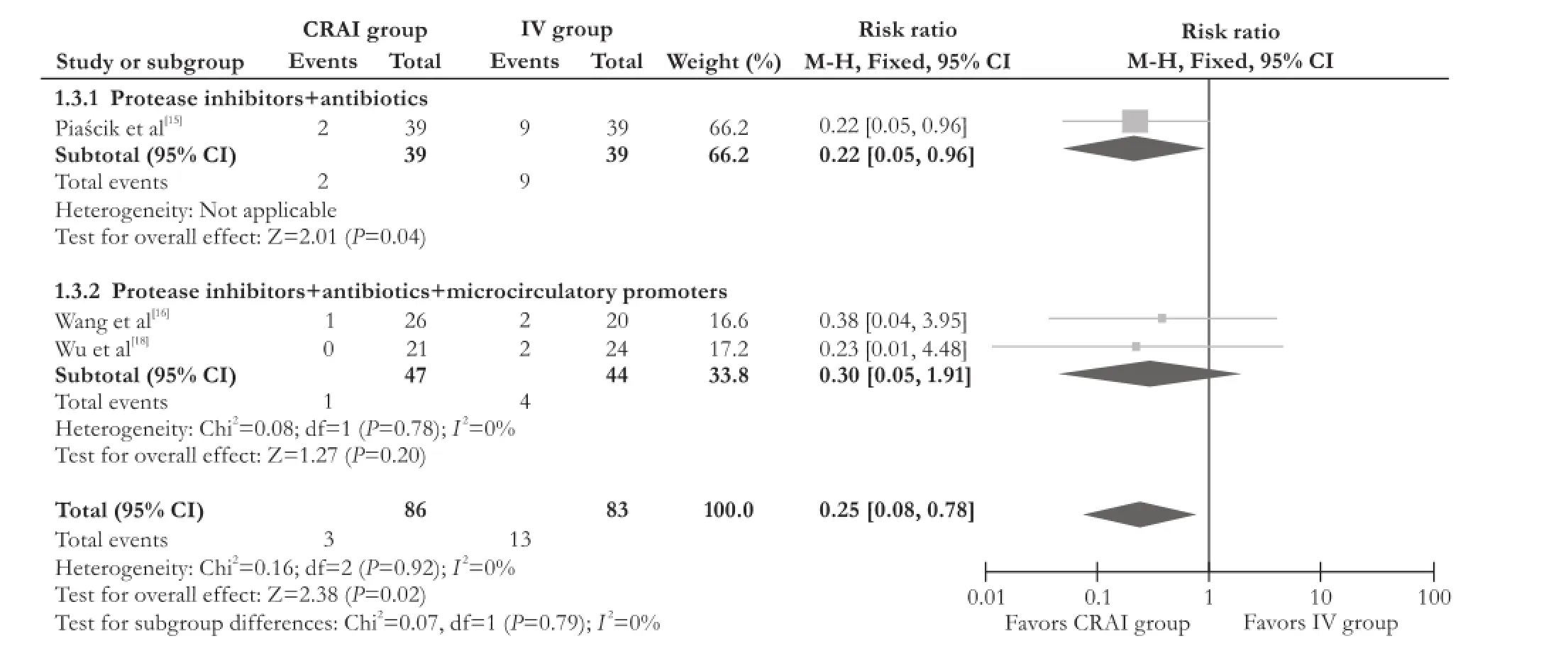
Fig. 4.Forest plot showed that compared with the IV group, the mortality rate of the CRAI group was signifcantly decreased. CRAI: continuous regional arterial infusion; IV: intravenous infusion.
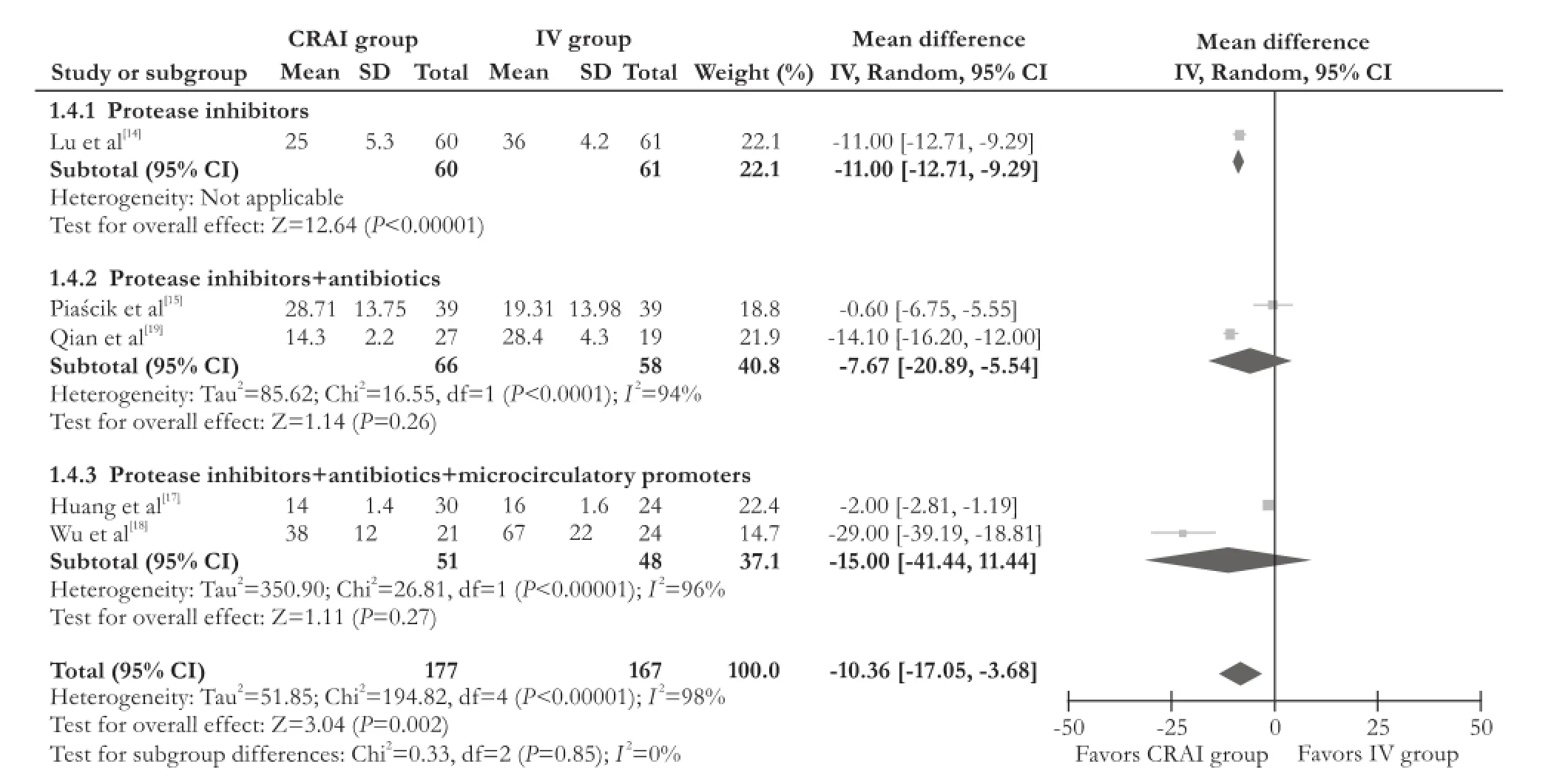
Fig. 5.Forest plot showed that compared with the IV group, the duration of hospital stay of the CRAI group was signifcantly shortened. CRAI: continuous regional arterial infusion; IV: intravenous infusion.
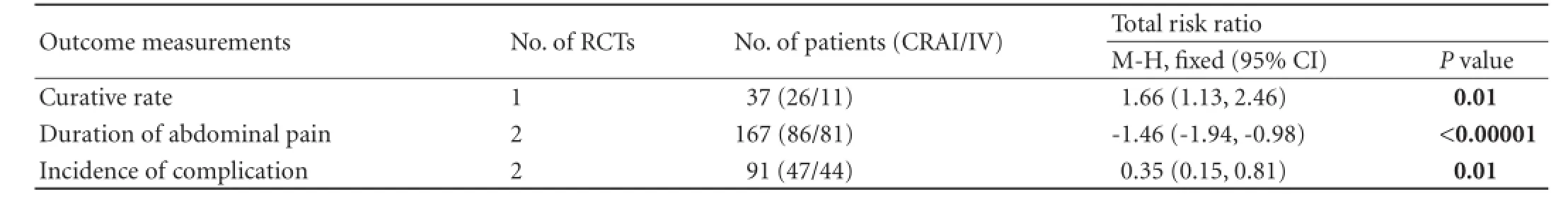
Table 4.Meta-analysis of secondary outcomes
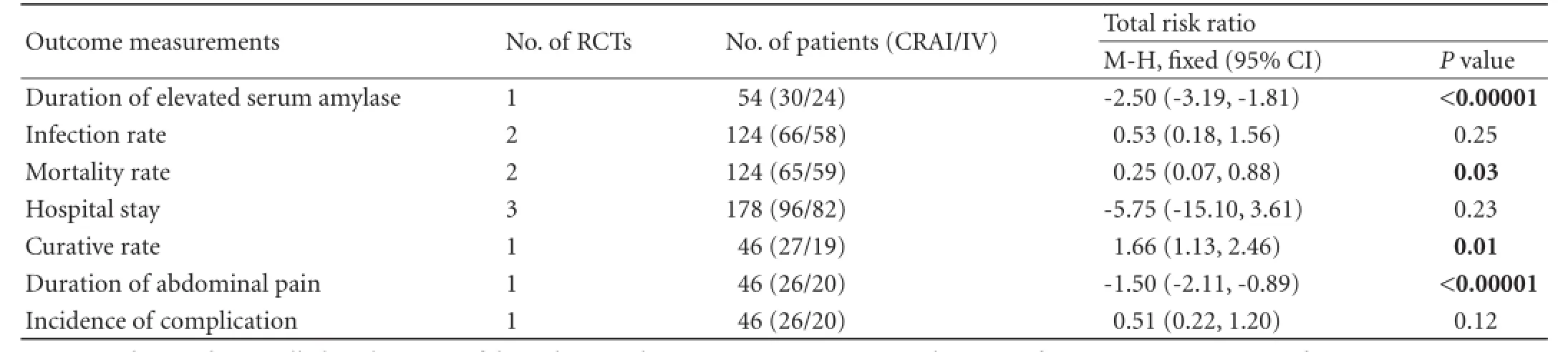
Table 5.Sensitivity analysis
As shown in Table 4, secondary outcomes such as the duration of abdominal pain, incidence of complications were signifcantly reduced in the CRAI group. The overall curative rate was signifcantly increased in the CRAI group.
Sensitivity analysis
We performed a sensitivity analysis to explore the infuence of the two studies describing the specifcally randomized method on the estimation of treatment effect. We repeated the analysis excluding the two studies.[14,18]The results showed that CRAI signifcantly shortened the duration of elevated serum amylase compared with IV route (MD=-2.50, 95% CI=-3.19, -1.81;P<0.00001), the duration of abdominal pain (MD=-1.50, 95% CI=-2.11, -0.89;P<0.00001) and decreased the overall mortality (RR=0.25, 95% CI=0.07, 0.88;P=0.03). CRAI signifcantly increased the curative rate (RR=1.66, 95% CI=1.13, 2.46;P=0.01). The duration of hospital stay (MD=-5.75, 95% CI=-15.10, 3.61;P=0.23), the incidence of complication (RR=0.51, 95% CI=0.22, 1.20;P=0.12), and the infection rate (RR=0.53, 95% CI=0.18, 1.56;P=0.25) were not signifcantly different between the CRAI and IV groups (Table 5).
Adverse reactions
No mortality due to CRAI administration was reported in all these studies. No catheter-related infections were found in all CRAI cases. One study[19]reported that one patient developed temporary arterial vasospasm, 3 developed puncture bleeding, and 2 had thrombus obstruction at the tip of the catheter.
Discussion
Synthetic PIs, a broad inhibitory action on pancreatic enzymes, the coagulation system, the complement system and the production of proinfammatory cytokines, are expected to prevent necrotic changes in the pancreas and to reduce the mortality rate. PIs can directly reach the pancreas via the CRAI delivery system, but intravenous administration cannot reach an effective concentration due to the pharmacokinetic characteristics and impaired microcirculation during the pathophysiologic course of SAP. Yamauchi et al[23]found that the concentration of PI in the pancreatic tissue was fve times higher by using CRAI than IV route. Satoh et al[24]reported that the concentration of nafamostat mesilate in the pancreas infused by CRAI was 32 times higher than that infused intravenously in SAP rats. The concentration of antibiotics or other drugs might also be infuenced because of the reduced vasculature and lowered perfusion of pancreatic tissue in acute necrotizing pancreatitis.[25]So CRAI is regarded as an effective treatment for SAP by dramatically increasing the drug concentration in the pancreas.
Six RCTs involving 390 cases were included for the present meta-analysis. Overall, the results of this metaanalysis show that CRAI drug delivery is effective for SAP. Compared with IV route, CRAI route decreased the overall mortality, shortened hospital stay. Out of six included studies, only one study[14]recorded the duration of elevated urine amylase. The results showed that the duration of elevated urine amylase was shortened by 2.4 days in the CRAI group (MD=-2.40, 95% CI=-3.20, -1.60;P<0.00001). The included studies reported theCRAI drug delivery system decreased the level of C-reactive protein, white blood cell earlier.[15,16]Computed tomography severity index also dramatically decreased after CRAI treatment.[14,15]These provided the indirect evidences for the treatment of SAP by CRAI drug delivery. Subgroup analysis showed no signifcant difference between three strategies. Sensitivity analysis showed that CRAI shortened the duration of elevated serum amylase compared with the IV route. Hospital stay and incidence of complication had no signifcant difference between the two groups. The rest of results of sensitivity analysis are consistent with the overall results.
There are some unavoidable shortcomings in this meta-analysis. First, the diagnostic criteria of SAP were not completely inconsistent among the included studies. The CRAI and IV groups were not completely compared in the baseline conditions and severity of SAP. Thus, there might be selection bias in these studies. Second, we rigorously evaluated the methodological quality of the included studies, and found none of them meet all the criteria. As CRAI is an invasive operation, blinding method would be diffcult for practice. Consequently, observer bias may be present. Among all the studies included, only one study,[16]reported the loss of follow-up. So there was unavoidable loss of follow-up bias. The sample size of the included RCTs were small, so the results of present analysis may be not reliable enough. Third, this metaanalysis found no consensus on the optimal timing of CRAI therapy among the studies. In addition, the dosage of drugs administrated by CRAI and course of treatment were different among the included studies. Forth, there may be a possible publication bias, as 5 of the 6 studies were published in Chinese on domestic core journals and only one study published in English cited by Scientifc Citation Index.
In conclusion, the evidence of the present metaanalysis suggested that CRAI is effective for the treatment of SAP, and the drug combination via CRAI did not have a signifcant impact on the effective in improving outcomes. Due to the lack of highly qualifed RCTs, there might be bias in the evaluation of CRAI for the treatment of SAP in this meta-analysis. Therefore, highquality multicenter trials involving a larger number of patients are needed to obtain more reliable evidence to explore the effectiveness and safety of CRAI.
Acknowledgement:We thank Kathren Sieminski and Yu-Fei Cheng for their help in English language polishing.
Contributors:YFJ and XQ designed the work; YFJ and MXY were responsible for methodology, literatures search and data management; DLH and ZMM did quality assessment of literatures and arbitration of disagreement; YFJ, MXY and DLH wrote the paper. YFJ and MXY contributed equally to this work. XQ is the guarantor.
Funding:This study was supported by a grant from Sichuan Provincial Science and Technology Support Program (2013SZ0078).Ethical approval:Not needed.
Competing interest:No benefts in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
1 Toh SK, Phillips S, Johnson CD. A prospective audit against national standards of the presentation and management of acute pancreatitis in the South of England. Gut 2000;46:239-243.
2 Neoptolemos JP, Raraty M, Finch M, Sutton R. Acute pancreatitis: the substantial human and fnancial costs. Gut 1998;42: 886-891.
3 Mitchell RM, Byrne MF, Baillie J. Pancreatitis. Lancet 2003;361: 1447-1455.
4 Takeda K, Matsuno S, Sunamura M, Kakugawa Y. Continuous regional arterial infusion of protease inhibitor and antibiotics in acute necrotizing pancreatitis. Am J Surg 1996;171:394-398.
5 Takeda K, Matsuno S, Ogawa M, Watanabe S, Atomi Y. Continuous regional arterial infusion (CRAI) therapy reduces the mortality rate of acute necrotizing pancreatitis: results of a cooperative survey in Japan. J Hepatobiliary Pancreat Surg 2001;8:216-220.
6 Imaizumi H, Kida M, Nishimaki H, Okuno J, Kataoka Y, Kida Y, et al. Effcacy of continuous regional arterial infusion of a protease inhibitor and antibiotic for severe acute pancreatitis in patients admitted to an intensive care unit. Pancreas 2004;28:369-373.
7 Mikami Y, Takeda K, Matsuda K, Qiu-Feng H, Fukuyama S, Egawa S, et al. Rat experimental model of continuous regional arterial infusion of protease inhibitor and its effects on severe acute pancreatitis. Pancreas 2005;30:248-253.
8 Yasuda T, Ueda T, Takeyama Y, Shinzeki M, Sawa H, Nakajima T, et al. Treatment strategy against infection: clinical outcome of continuous regional arterial infusion, enteral nutrition, and surgery in severe acute pancreatitis. J Gastroenterol 2007;42: 681-689.
9 Ino Y, Arita Y, Akashi T, Kimura T, Igarashi H, Oono T, et al. Continuous regional arterial infusion therapy with gabexate mesilate for severe acute pancreatitis. World J Gastroenterol 2008;14:6382-6387.
10 Takeda K, Yamauchi J, Shibuya K, Sunamura M, Mikami Y, Matsuno S. Beneft of continuous regional arterial infusion of protease inhibitor and antibiotic in the management of acute necrotizing pancreatitis. Pancreatology 2001;1:668-673.
11 Hamada T, Yasunaga H, Nakai Y, Isayama H, Horiguchi H, Matsuda S, et al. Continuous regional arterial infusion for acute pancreatitis: a propensity score analysis using a nationwide administrative database. Crit Care 2013;17:R214.
12 Ishikawa T, Imai M, Kamimura H, Ushiki T, Tsuchiya A, Togashi T, et al. Therapeutic effcacy of continuous arterial infusion of the protease inhibitor and the antibiotics and via celiac and superior mesenteric artery for severe acute pancreatitispilot study. Hepatogastroenterology 2009;56:524-528.
13 Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. Available from www.cochrane-handbook.org.
14 Lu JH, Kang ZC, Lu FW, Zhang WJ, Qi J, Pang YL, et al. CT associated with clinical indices to evaluate therapeutic effcacy of continuous regional intra-arterial infusion of somatostatin for treatment of severe acute pancreatitis. Clinical Focus 2013;28: 49-52.
15 Piaścik M, Rydzewska G, Milewski J, Olszewski S, Furmanek M, Walecki J, et al. The results of severe acute pancreatitis treatment with continuous regional arterial infusion of protease inhibitor and antibiotic: a randomized controlled study. Pancreas 2010;39:863-867.
16 Wang LC, Yao XX. The value of regional arterial perfusion for acute pancreatitis. Hebei Med J 2010;32:1378-1380.
17 Huang Z, Luo L, Lin SH, Su YQ. Celiac artery perfusion in the treatment of 30 cases with severe acute pancreatitis. J Guiyang Coll Tradit Chin Med 2007;29:24-25.
18 Wu XQ, Yu YS, Cheng YC, Lu W, Wu WX. The clinical effectiveness observation of regional arterial infusion for severe acute pancreatitis. Zhejiang Med J 2005;27:682-683.
19 Qian ZY, Liu XL, Miao Y, Feng YL, Xu ZK, Dai CC, et al. Clinical research of regional intra-arterial infusion and whole body infusion in the treatment of severe acute pancreatitis. Chin J Pancreatol 2001;1:40-42.
20 Study Group of the Pancreas, Chinese Medical Association Society of Surgery. Diagnosis and grading criteria of acute pancreatitis (second program, 1996). Chin J Surg 1997;35:773-775.
21 Zhang TP, Zhao YP, Wang L. The seventh Minutes of Pancreatic Surgery Seminar. Chin J Gen Surg 1999;14:139-140.
22 Study Group of the Pancreas, Chinese Medical Association Society of Surgery. The guideline of diagnosis and treatment of severe acute pancreatitis. Chin J Surg 2007;45:727-729.
23 Yamauchi J, Takeda K, Shibuya K, Sunamura M, Matsuno S. Continuous regional application of protease inhibitor in the treatment of acute pancreatitis. An experimental study using closed duodenal obstruction model in dogs. Pancreatology 2001;1:662-667.
24 Satoh H, Harada M, Tashiro S, Shiroya T, Imawaka H, Machii K. The effect of continuous arterial infusion of gabexate mesilate (FOY-007) on experimental acute pancreatitis. J Med Invest 2004;51:186-193.
25 Inoue K, Hirota M, Beppu T, Ishiko T, Kimura Y, Maeda K, et al. Angiographic features in acute pancreatitis: the severity of abdominal vessel ischemic change refects the severity of acute pancreatitis. JOP 2003;4:207-213.
Received December 6, 2013
Accepted after revision August 27, 2014
AuthorAffliations:Sichuan Provincial Pancreatitis Center, Department of Integrated Traditional and Western Medicine (Yong FJ, Deng LH and Xia Q); Chinese Evidenced-Based Medical Center (Mao XY and Zhang MM), West China Hospital, Sichuan University, Chengdu 610041, China
Qing Xia, MD, Director of Sichuan Provincial Pancreatitis Center, Department of Integrated Traditional and Western Medicine, West China Hospital, Sichuan University, No. 37 Guoxue Rd, Chengdu 610041, China (Tel/Fax: +86-28-85423373; Email: xiaqing@ medmail.com.cn)
© 2015, Hepatobiliary Pancreat Dis Int. All rights reserved.
10.1016/S1499-3872(14)60290-3
Published online December 30, 2014.
杂志排行
Hepatobiliary & Pancreatic Diseases International的其它文章
- Meetings and Courses
- Blunt abdominal injury with rupture of giant hepatic cavernous hemangioma and laceration of the spleen
- Enlarged pancreas: not always a cancer
- p38 MAPK inhibition alleviates experimental acute pancreatitis in mice
- Predictors of incidental gallbladder cancer in elderly patients
- Liver, biliary and pancreatic injuries in pancreaticobiliary maljunction model in cats