Enlarged pancreas: not always a cancer
2015-02-07
Bologna, Italy
Enlarged pancreas: not always a cancer
Lucia Calculli, Davide Festi and Raffaele Pezzilli
Bologna, Italy
Pancreatic fat accumulation has been described with various terms including pancreatic lipomatosis, pancreatic steatosis, fatty replacement, fatty infltration, fatty pancreas, lipomatous pseudohypertrophy and nonalcoholic fatty pancreas disease. It has been reported to be associated with type 2 diabetes mellitus, acute pancreatitis, pancreatic cancer and the formation of pancreatic fstula. The real incidence of this condition is still unknown. We report a case of pancreatic steatosis in a non-obese female patient initially diagnosed with a mass in the head of the pancreas. Magnetic resonance imaging (MRI) was carried out to defne the characteristics of the pancreatic mass. MRI confrmed the diagnosis of fat pancreas. Enlarged pancreas is not always a cancer, but pancreatic steatosis is characterized by pancreatic enlargement. MRI could give a defnite diagnosis of pancreatic steatosis or cancer.
pancreatic steatosis;magnetic resonance image; computer tomography; IgG4; differential diagnosis; clinical course
Introduction
The synonyms of pancreatic fat accumulation include pancreatic lipomatosis, pancreatic steatosis, fatty replacement, fatty infltration, fatty pancreas, lipomatous pseudohypertrophy and nonalcoholic fatty pancreas disease.[1]Pancreatic steatosis is thought to be associated with type 2 diabetes mellitus, acute pancreatitis, pancreatic cancer and pancreatic fstula. The incidence of this condition is still not clear. We report herein a case of pancreatic steatosis in a non-obese female patient initially diagnosed with a mass in the head of the pancreas. Magnetic resonance imaging (MRI) made a fnal diagnosis of fat pancreas.
Case report
A 37-year-old Caucasian woman was admitted to the outpatient department because ultrasonographic examination revealed an enlarged pancreas. The patient was not a drinker of alcohol nor a smoker. She was asymptomatic and her body mass index was 22.1 (height 169 cm, weight 63 kg). Her clinical history was normal. Blood examinations revealed that the levels of transaminases, gamma-glutamyl transpeptidase, alkaline phosphatases, amylase, lipase, triglycerides, total cholesterol, high-density lipoprotein (HDL) cholesterol and lowdensity lipoprotein (LDL) cholesterol were within the normal limits. She was negative for hepatitis B and C virus. The oral glucose tolerance test showed nothing abnormal. She underwent MRI of the abdomen, showing the presence of an enlarged pancreatic head [longitudinal diameter 45.0 mm (upper reference value 35.0 mm), transversal diameter 35.0 mm (upper reference value 30.0 mm) and anteroposterior diameter 27.0 mm (upper reference value related to age 21.4 mm][2](Fig. 1). After fat suppression, MRI of the head of the pancreas showed a homogeneous and diffuse reduction of signal intensity (Fig. 2).
The diagnosis of pancreatic steatosis was made. For a better defnition of this radiological picture, the patient was subjected to a genetic evaluation. Analysis of the CFTR gene, SPINK-1, PRSS-1 and hemochromatosis genes showed no mutations. Finally, IgG4 was found within the normal limits (28 mg/dL, normal reference range: 8-140), whereas total IgE was elevated as 336 UI/mL in contrast to normal reference range: <100. No drugs were given to the patient for the treatment of pancreatic steatosis.

Fig. 1.Magnetic resonance of the abdomen showing the presence of an enlarged pancreatic head.
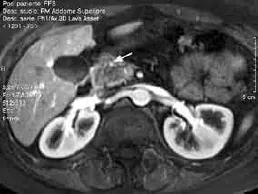
Fig. 2.Magnetic resonance after the fat suppression: the head of the pancreas shows a homogeneous and diffuse reduction of signal intensity (arrow).
Discussion
Ogilvie[3]frst described pancreatic steatosis and found an incidence of 9% in normal weight individuals versus 17% in pancreatic fat individuals in 19 autopsy studies of obese subjects. In addition, the amount of pancreatic fat increases signifcantly with age, in patients with type 2 diabetes mellitus and in those with severe generalized atherosclerosis.[1]Other diseases such as congenital syndromes, hemochromatosis and viral infections were also hypothesized to explain the presence of pancreatic steatosis.[1]In our patient, these conditions were ruled out by specifc examinations. Finally, pancreatic steatosis was found to be related to obesity and that its incidence is increasing in Western countries. Pancreatic steatosis is associated with such diseases as metabolic syndrome, cardiovascular diseases and cancer.[4]Our patient was not obese and her BMI was 22.1. It has been reported that obesity is not necessarily a pre-requisite for pancreatic steatosis as the disease also occurs in non-obese individuals.[1]To the present, the incidence of pancreatic steatosis is obscure. Further studies are necessary to evaluate the incidence of pancreatic steatosis in the general population and to explain its pathophysiology.
Contributors:FD and PR followed clinically the patients. CL carried out the imaging studies. PR drafted the manuscript. All the authors gave their consent for the fnal version. PR is the guarantor.
Funding:None.
Ethical approval:Not needed.
Competing interest:No benefts in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
1 Smits MM, van Geenen EJ. The clinical signifcance of pancreatic steatosis. Nat Rev Gastroenterol Hepatol 2011;8: 169-177.
2 Sato T, Ito K, Tamada T, Sone T, Noda Y, Higaki A, et al. Agerelated changes in normal adult pancreas: MR imaging evaluation. Eur J Radiol 2012;81:2093-2098.
3 Ogilvie R. The island of Langerhans in 19 cases of obesity. J Pathol 1933;37:473-481.
4 Ogden CL, Yanovski SZ, Carroll MD, Flegal KM. The epidemiology of obesity. Gastroenterology 2007;132:2087-2102.
Received May 22, 2014
Accepted after revision August 22, 2014
(Hepatobiliary Pancreat Dis Int 2015;14:107-108)
AuthorAffliations:Departments of Radiology (Calculli L) and Digestive Diseases (Festi D) and Internal Medicine (Pezzilli R), Sant'Orsola-Malpighi Hospital, Via Massarenti 9, Bologna 40138, Italy
Raffaele Pezzilli, MD, Department of Digestive Diseases and Internal Medicine, Sant'Orsola-Malpighi Hospital, Via Massarenti 9, Bologna 40138, Italy (Tel/Fax: +39-51-636-4148; Email: raffaele.pezzilli@ aosp.bo.it)
© 2015, Hepatobiliary Pancreat Dis Int. All rights reserved.
10.1016/S1499-3872(15)60329-0
Published online January 2, 2015.
杂志排行
Hepatobiliary & Pancreatic Diseases International的其它文章
- Meetings and Courses
- Blunt abdominal injury with rupture of giant hepatic cavernous hemangioma and laceration of the spleen
- p38 MAPK inhibition alleviates experimental acute pancreatitis in mice
- Predictors of incidental gallbladder cancer in elderly patients
- Liver, biliary and pancreatic injuries in pancreaticobiliary maljunction model in cats
- Development of hybrid-type modifed chitosan derivative nanoparticles for the intracellular delivery of midkine-siRNA in hepatocellular carcinoma cells