Combined right hemicolectomy and pancreaticoduodenectomy for locally advanced right hemicolon cancer
2015-02-06
Hangzhou, China
Combined right hemicolectomy and pancreaticoduodenectomy for locally advanced right hemicolon cancer
Qin-Song Sheng, Wen-Bin Chen, Min-Jiang Li, Xiao-Bin Cheng, Wei-Bing Wang and Jian-Jiang Lin
Hangzhou, China
Extracolonic invasion of the duodenum and/or pancreatic head rarely occurs in patients with right hemicolon cancer. However, when necessary, combined radical operation is a challenge to the surgeon. We reported 7 patients with locally advanced right hemicolon cancer who underwent combined right hemicolectomy (RH) and pancreaticoduodenectomy (PD) due to direct involvement of the duodenum or pancreatic head. This study included four males and three females with a mean age of 66.9±5.9 years. Computed tomography (CT) scans revealed right hemicolon cancer with duodenal invasion (5 patients) and pancreatic invasion (2). The mean operation time was 410±64 minutes and the estimated blood loss was 514±157 mL. After the operation, the mean postoperative hospital stay was 22.1±7.2 days. Five patients had postoperative complications. The mean follow-up time was 16.4±5.9 months. During this period, three patients died from tumor recurrence, one from postoperative complications, one from pulmonary disease, and two survived until the last scheduled follow-up. Five patients survived more than one year. Combined RH and PD for locally advanced right hemicolon cancer can be performed safely, thus providing a longterm survival rate in selected patients in a high-volume center.
combined resection;pancreaticoduodenectomy; colectomy; colon cancer; direct invasion
Introduction
Locally advanced colorectal cancers, defned as the invasion of neighboring organs and structures without distant metastases, account for 5.2%-23.6% of all colorectal tumors at the presentation.[1]Extracolonic invasion usually appears in the rectum and sigmoid colon in which pelvic organs and tissues may be invaded, but it rarely occurs in the right colon or proximal transverse colon.[2,3]Especially, right hemicolon cancer with direct infltration of the duodenum and/or pancreatic head usually produces more morbidity, posing a surgical challenge.[3]Combined resection of multiple organs is recognized as the best therapeutic strategy for patients with locally advanced colon carcinoma without distant metastasis. Combined right hemicolectomy (RH) and pancreaticoduodenectomy (PD) is the best radical choice to treat locally advanced right hemicolon cancer.[1,3-5]Locally advanced colorectal cancer seldom appears in the right side of the colon and reports on the occurrence are rare. The morbidity and long-term prognosis of patients with right colon carcinoma who have undergone combined RH and PD are not clear.[6,7]This report is to share our experience in seven patients who successfully underwent combined RH and PD to treat locally infltrative right hemicolon cancer invading the duodenum and/or pancreatic head directly.
Methods
Patients
A total of 2 772 patients with right hemicolon carcinoma who had radical RH with or without multi-organ operation were analyzed. These patients were treated at the First Affliated Hospital, Zhejiang University School of Medicine between January 2000 and December 2013. From the medical records, seven patients who had undergone combined RH and PD due to direct involvementof the duodenum or pancreatic head were identifed.
The seven patients had symptoms of abdominal distension, upper abdominal discomfort, melena, anemia, or a change in bowel habits. One patient had jaundice and three patients had a palpable abdominal mass, but digital rectal examinations were negative. The preoperative cancer antigen 19-9 and carcinoembryonic antigen (CEA) levels were routinely tested in all patients. Preoperative computed tomography (CT) was routinely performed to evaluate local tumor invasion. Preoperative upper endoscopy, colonoscopy, and pathological affrmation of the diagnosis were carried out in all patients.
The indications for surgery included the following: 1) patients with histologically confrmed colon carcinoma; 2) patients without severe comorbid disease and tolerable to a radical multi-organ excision; 3) colon cancer which could not be dissociated from the pancreatic head or duodenum; 4) R0 resection feasible on account of preoperative evaluation and no distant metastasis; and 5) the surgical team who have suffcient operating skills and clinical experience to perform such a delicate operation.[1,3,6,7]Patients with high surgical risk, distant metastasis, or secondary invasion of the pancreatic head and/or the duodenum rather than direct infltration were excluded. And those who had local duodenal invasion that could be excised radically by a partial duodenal wall resection were also excluded.[1,8]
Operations
After the right hemicolon was dissociated, a Kocher maneuver was made to completely separate the duodenum to create a distinct plane between the tumor and the superior mesenteric artery. Then the terminal common bile duct was separated and retracted for the ligation of the gastroduodenal artery. A tunnel was established in the plane anterior to the portal vein behind the pancreatic neck. The plane was established at the inferior margin of the pancreas medial to the arranged course of the superior mesenteric vein. The resectability of colon cancer was evaluated after entire separation of the right hemicolon and duodenum. The involvement of the duodenum or pancreas was evaluated after liberation of the original adhesions to the right hemicolon. If resection was feasible, RH was done according to a standard procedure. A stapled ileocolic side-to-side anastomosis was made. PD was performed with a standard procedure, and reconstruction was subsequently undertaken according to Child's reconstruction method.[9]After the resection and reconstruction, suction drains were placed into the pelvis and near the anastomotic stomas, and the abdominal wall wounds were closed.
The tumor stage was assessed according to the tumor-lymph node-metastasis (TNM) classifcation recommended by the American Joint Committee of Cancer.[10]Postoperative complications were categorized according to the reported criteria including the presence of pancreatic fstula (PF),[11]delayed gastric emptying (DGE)[12]and acute respiratory distress syndrome (ARDS).[13]
Statistical analysis
Demographic variables, intraoperative parameters, and postoperative data were recorded. In addition, all patients were asked to visit our outpatient department every month after discharge and the complications during the follow-up period were also recorded. Numerical data were presented as mean±standard deviation.
Results
Seven patients (4 males and 3 females) with locally advanced carcinoma of the right hemicolon invading the duodenum or pancreatic head had undergone combined RH and PD. The mean age of the patients was 66.9±5.9 years. The tumor was located at right colic fexure (3 patients) and the ascending colon (4). CT scans revealed duodenal invasion in fve patients and pancreatic invasion in two. Preoperative upper endoscopies revealed colon tumors without mucosal involvement. The pathological results confrmed the diagnosis of right hemicolon cancer in all of the patients, and their preoperative CEA values were 9.3±6.9 ng/mL. The CA19-9 levels were normal in all patients. None of the patients underwent preoperative chemotherapy. The demographic variables of the patients are listed in Table 1.
The operations in all patients were performed successfully. The average operation time was 410±64 minutes, and the estimated blood loss was 514±157 mL. Blood was transfused intraoperatively in all patients with an average amount of 3.7±1.4 U. Pathological examination confrmed the involvement of the duodenum (5 patients) and pancreas (2). In addition, moderately differentiated adenocarcinoma (5 patients) and poorly differentiated adenocarcinoma (2) were confrmed histologically. According to the TNM classifcation system, stage T4bN1bM0(2 patients), stage T4bN0M0(3), stage T4bN2aM0(1), and stage T4bN2bM0(1) were defned. The intraoperative parameters are listed in Table 2.
After the operation, the postoperative hospital stay was 22.1±7.2 days. None of the patients died during the hospital stay. Five patients had postoperative complications including DGE (1 patient), ileus (2), wound infection (3), ARDS (2), and PF (1). The patients recovered after conservative treatments. Among them, fve patientsreceived adjuvant chemotherapy, including modifed folfox 6 (3 patients) and capecitabine plus oxaliplatin treatment (2). The median follow-up time was 16.4±5.9 months. During this period of follow-up, three patients died from tumor recurrence, one from postoperative complications, one from pulmonary disease, but two were alive. Five patients survived more than one year. The survival time of the four patients with lymph node metastasis was 13.8±4.5 months, whereas that of the three patients without lymph node metastasis was 20±6.2 months. The postoperative data of the patients are listed in Table 3.
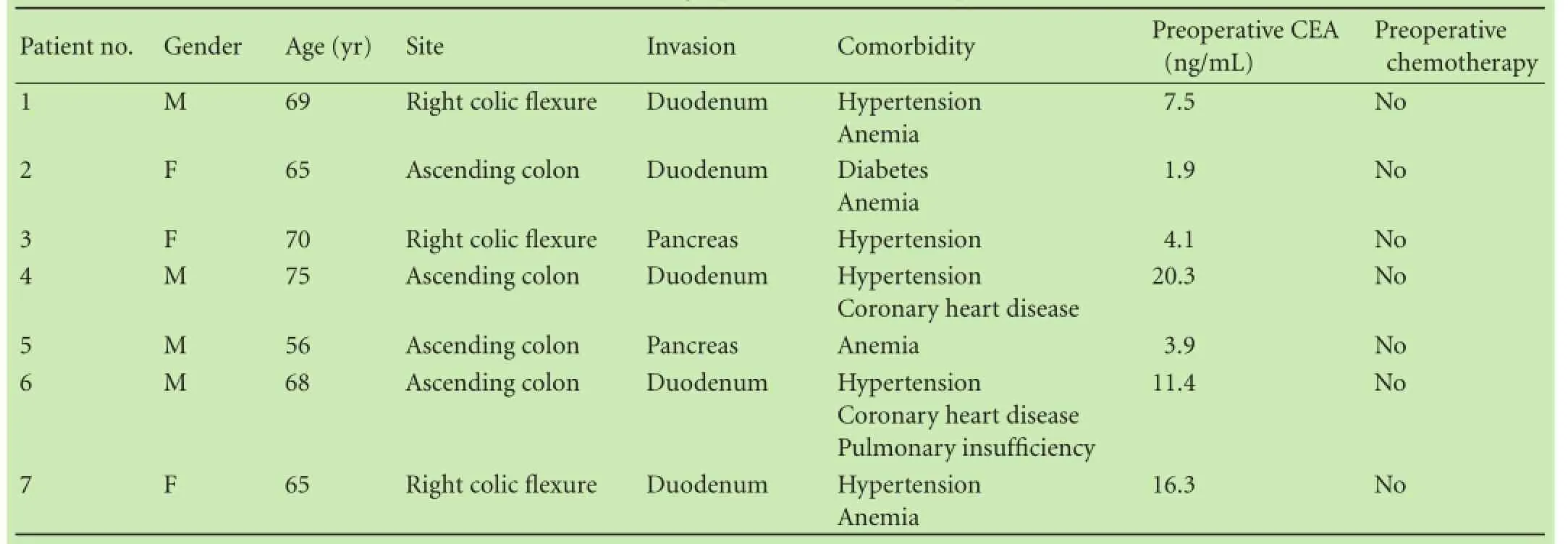
Table 1.Demographic variables of the patients
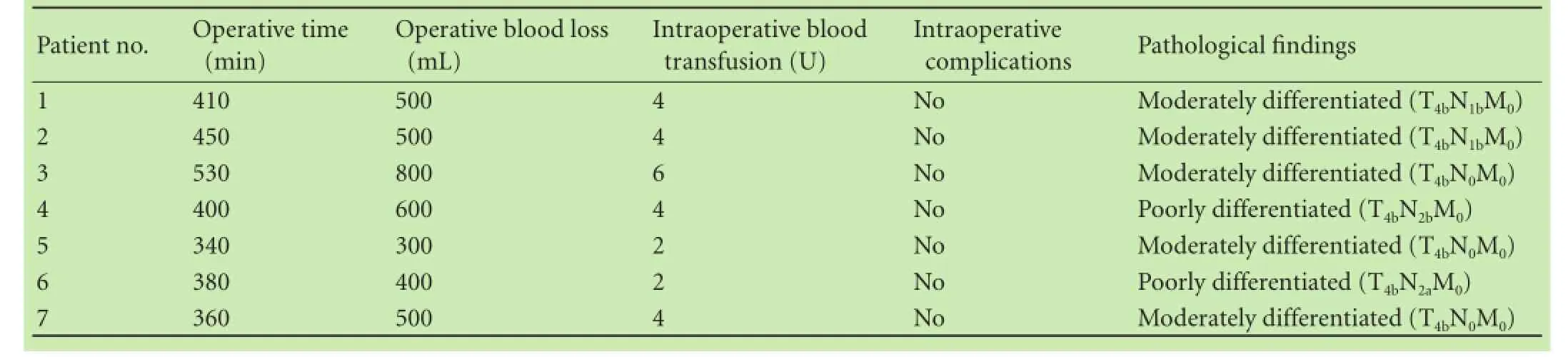
Table 2.Intraoperative parameters of the patients
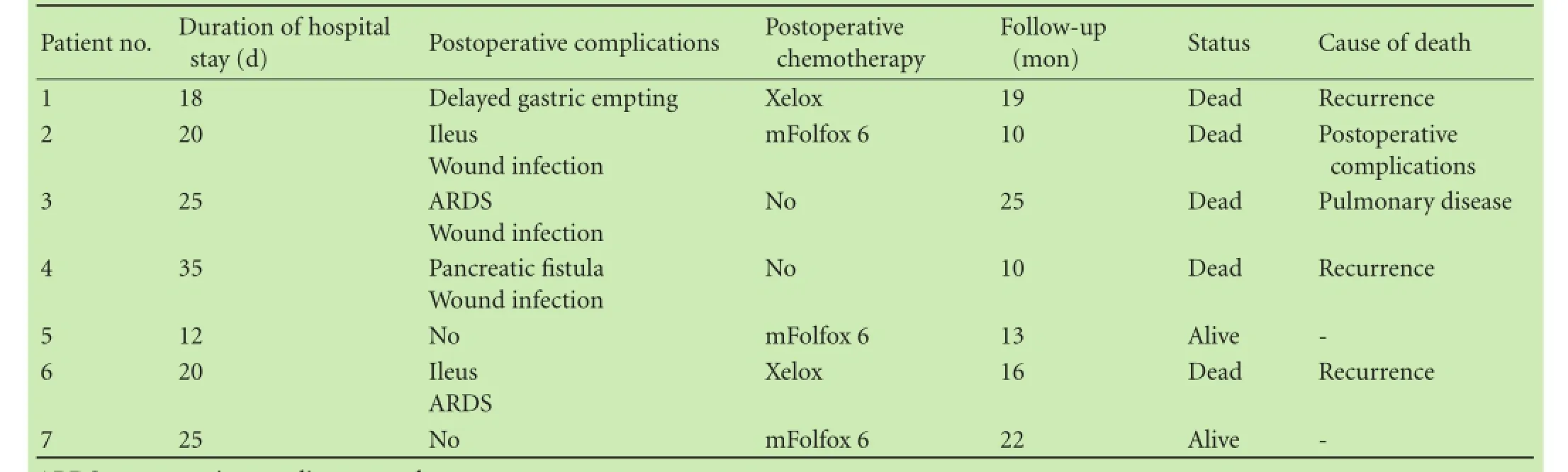
Table 3.Postoperative data of the patients
Discussion
Patients who have received margin negative multiple organ resection usually have a similar survival rate compared with those who have no neighboring structure invasion. However, local recurrence of a tumor is common (70%-100%) in patients without multiple organ resection. Therefore, many researchers[4,6,14]have suggested a combined resection of the colorectal tumor with the neighboring organs and structures. Since right hemicolon cancer is suspected to infltrate the duodenum and/ or pancreatic head, combined RH and PD might be necessary to radically resect the tumor.[1,3]However, some researchers[1]think that combined RH and PD for locally advanced right hemicolon cancer is not the best choice of treatment. First, locally advanced cancers are largely considered to be highly malignant. Second, a combined RH and PD procedure represents a surgical challenge to the surgeon due to its diffculty, complexity, and high postoperative morbidity and mortality. In addition, the surgeon's individual experience and fnancial restrictions also need to be considered.[6]
In the past, extracolonic invasion was usually frst discovered at the time of laparotomy. The results of preoperative abdominal CT often indicated imprecise information about the degree of pancreatic or duodenal invasion due to right hemicolon cancer.[2,3]With the development of CT technology, however, a recent metaanalysis showed that CT precisely stage colonic tumors preoperatively and provide information about cancer involvement exceeding the muscularis propria.[15]In the current study, preoperative CT accurately revealed duodenal invasion in fve and pancreatic invasion in two patients, which were consistent with the intraoperative fndings. However, a study[7]found that imaging often cannot distinguish infammatory adhesions from direct tumor infltration. Even in surgical exploration, it is often diffcult to determine whether gross adhesions to the carcinoma represent true malignant infltration or an infammatory reaction.[1]Moreover, a histological study showed that 55%-70% of adhesions are tumor invasions while the remainder are tumor-related infammatory adherence.[3]Therefore, the adherences between the tumor and adjacent structures should be considered malignant. When a right hemicolon cancer is staged as T4bNxM0, combined multiple organ operation should be performed once the patient is suitable for a radical surgery.[1]In the current study, all the patients were confrmed to have dense adherences between right hemicolon cancer and the duodenum or pancreas, and were candidates for a combined radical resection. The fnal histological results confrmed duodenal or pancreatic invasion in all patients.
According to previous reports, 25%-60% of cases of colon cancer that invades the neighboring duodenum and/or pancreas do not have lymphatic metastasis.[1]These results indicate that neoplasms spread in a locally advanced manner rather than lead to hematogenous or lymphatic metastasis, which is an important prognostic factor for local recurrence, distant metastasis, and survival in patients with colon carcinoma.[3]Therefore, patients with locally aggressive colon cancer without lymphatic metastasis have a longer postoperative survival time than those with lymphatic metastasis.[4,6]The present report showed similar results.
According to previous reports, the prognosis of patients with colorectal cancer who have undergone a combined RH and PD is promising.[1,4,6]The long-term outcomes after the combined operation for right hemicolon cancer invading the pancreas resemble those after the operation for colorectal carcinoma invading other organs or structures. It remains to be answered whether radical and combined operation of the neoplasm can improve the survival time of the patients. Especially, in patients with stage T4 right hemicolon cancer who accept combined resection with PD, the average disease-free survival may reach 54 months.[2]In the current study, the average survival time was 16.4±5.9 months, whereas the overall one-year survival rate of patients was 5/7. Two patients in this series were alive after the scheduled follow-up.
However, information from this particular subsection of patients might not refect the actual situation. First, the incidence of colorectal cancer invading neighboring organs might not be representative because stagematched patients with right hemicolon cancer infltrating the duodenum or pancreas who rejected surgical treatment or only chose bypass surgery were not included in this study. Second, other researchers had different indications for the combined resection. Finally, many studies have suggested that these patients should be studied for a long-term period.[1,4]Since perioperative care and surgical skills keep improving, a long-term study might increase the variety of the data, making comparison of some variables between studies diffcult.
Contributors:SQS and CWB proposed the study. SQS performed the research and wrote the frst draft. LMJ, CXB and WWB collected and analyzed the data. All authors contributed to the design and interpretation of the study and to further drafts. CWB is the guarantor.
Funding:None
Ethical approval:Not needed.
Competing interest:No benefts in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
1 Zhang J, Leng JH, Qian HG, Qiu H, Wu JH, Liu BN, et al.En blocpancreaticoduodenectomy and right colectomy in the treatment of locally advanced colon cancer. Dis Colon Rectum 2013;56:874-880.
2 Costa SR, Henriques AC, Horta SH, Waisberg J, Speranzini MB.En-blocpancreatoduodenectomy and right hemicolectomy for treating locally advanced right colon cancer (T4): a series of fve patients. Arq Gastroenterol 2009;46:151-153.
3 Lee WS, Lee WY, Chun HK, Choi SH.En blocresection for right colon cancer directly invading duodenum or pancreatic head. Yonsei Med J 2009;50:803-806.
4 Saiura A, Yamamoto J, Ueno M, Koga R, Seki M, Kokudo N. Long-term survival in patients with locally advanced colon cancer afteren blocpancreaticoduodenectomy and colectomy. Dis Colon Rectum 2008;51:1548-1551.
5 Paquette IM, Swenson BR, Kwaan MR, Mellgren AF, Madoff RD. Thirty-day outcomes in patients treated withen bloccolectomy and pancreatectomy for locally advanced carcinoma of the colon. J Gastrointest Surg 2012;16:581-586.
6 Song XM, Wang L, Zhan WH, Wang JP, He YL, Lian L, et al. Right hemicolectomy combined with pancreatico- duodenectomy for the treatment of colon carcinoma invading the duodenum or pancreas. Chin Med J (Engl) 2006;119:1740-1743.
7 Cirocchi R, Partelli S, Castellani E, Renzi C, Parisi A, Noya G, et al. Right hemicolectomy plus pancreaticoduodenectomy vs partial duodenectomy in treatment of locally advanced right colon cancer invading pancreas and/or only duodenum. Surg Oncol 2014;23:92-98.
8 Fuks D, Pessaux P, Tuech JJ, Mauvais F, Bréhant O, Dumont F, et al. Management of patients with carcinoma of the right colon invading the duodenum or pancreatic head. Int J Colorectal Dis 2008;23:477-481.
9 Yang YL, Xu XP, Wu GQ, Yue SQ, Dou KF. Prevention of pancreatic leakage after pancreaticoduodenectomy by modifed Child pancreaticojejunostomy. Hepatobiliary Pancreat Dis Int 2008;7:426-429.
10 Edge SB, Compton CC. The American Joint Committee on Cancer: the 7th edition of the AJCC cancer staging manual and the future of TNM. Ann Surg Oncol 2010;17:1471-1474.
11 Xu M, Wang M, Zhu F, Tian R, Shi CJ, Wang X, et al. A new approach for Roux-en-Y reconstruction after pancreaticoduodenectomy. Hepatobiliary Pancreat Dis Int 2014;13:649-653.
12 Wente MN, Bassi C, Dervenis C, Fingerhut A, Gouma DJ, Izbicki JR, et al. Delayed gastric emptying (DGE) after pancreatic surgery: a suggested defnition by the International Study Group of Pancreatic Surgery (ISGPS). Surgery 2007;142:761-768.
13 Pitoyo CW. Acute respiratory distress syndrome. Acta Med Indones 2008;40:48-52.
14 Mora-Pinzon MC, Francescatti AB, Luu MB, Millikan KW, Deziel DJ, Hayden DM, et al.En blocright hemicolectomy/ pancreaticoduodenectomy for cancer: one institution's experience. Am Surg 2013;79:E238-239.
15 Dighe S, Purkayastha S, Swift I, Tekkis PP, Darzi A, A'Hern R, et al. Diagnostic precision of CT in local staging of colon cancers: a meta-analysis. Clin Radiol 2010;65:708-719.
(Hepatobiliary Pancreat Dis Int 2015;14:320-324)
AuthorAffliations:Department of Colorectal and Anal Surgery, The First Affliated Hospital, Zhejiang University School of Medicine, Hangzhou 310003, China (Sheng QS, Chen WB, Cheng XB, Wang WB and Lin JJ); Department of Colorectal and Anal Surgery, First People’s Hospital of Wenlin, Wenlin 317500, China (Li MJ)
Wen-Bin Chen, MD, Department of Colorectal and Anal Surgery, The First Affliated Hospital, Zhejiang University School of Medicine, Hangzhou 310003, China (Tel: +86-571-87236882; Email:cwbin@hotmail.com)
© 2015, Hepatobiliary Pancreat Dis Int. All rights reserved.
10.1016/S1499-3872(15)60374-5
Published online May 21, 2015.
Received November 30, 2014
Accepted after revision February 11, 2015
杂志排行
Hepatobiliary & Pancreatic Diseases International的其它文章
- Meetings and Courses
- Adjuvant chemotherapy after liver transplantation for hepatocellular carcinoma
- Letters to the Editor
- miR-215 overexpression distinguishes ampullary carcinomas from pancreatic carcinomas
- Endoscopic ultrasound-guided fne-needle aspiration cytology in pancreaticobiliary carcinomas: diagnostic effcacy of cell-block immunocytochemistry
- Omental faps reduces complications after pancreaticoduodenectomy
