MODS评分与应激性溃疡的相关性研究
2014-10-21林金锋杨志洲邵旦兵刘红梅张炜任艺孙兆瑞唐文杰聂时南
林金锋 杨志洲 邵旦兵 刘红梅 张炜 任艺 孙兆瑞 唐文杰 聂时南

DOI:10.3760/cma.j.issn.1671-0282.2014.08.003
基金项目:中国人民解放军南京军区重点课题(12Z32)
作者单位:210002 南京,解放军南京军区南京总医院急救医学科 南京大学医学院附属金陵医院
通信作者:聂时南,Email:shn_nie@sina.com
【摘要】目的 预测多器官功能障碍综合征(multiple organ dysfunction syndrome,MODS)患者應激性溃疡的发生,为其预防治疗提供依据。
访法 回顾性分析2008年8月至2012年8月入住南京军区南京总医院急诊重症监护病房(emergency intensive care unit, EICU )的符合MODS诊断标准的262例患者的临床资料。根据Marshall的MODS评分标准进行评分,依据应激性溃疡诊断标准判断应激性溃疡的发生,用秩相关分析MODS评分与应激性溃疡发生的相关性,应用受试者工作特征曲线(receiver operating characteristic curve,ROC)评价MODS评分对应激性溃疡的预测作用,计算Youden指数确定最佳临界值。
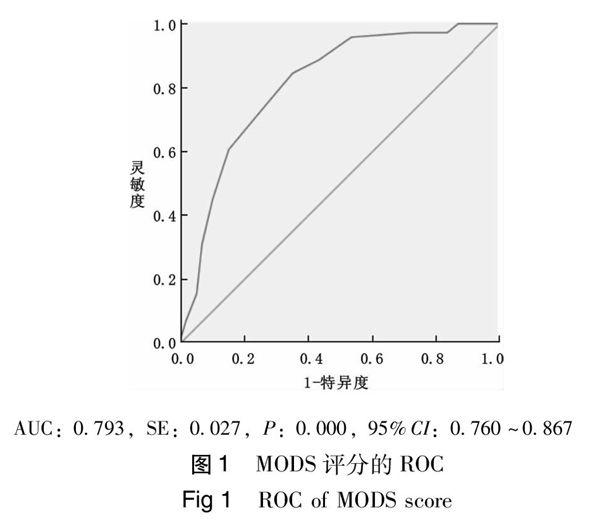
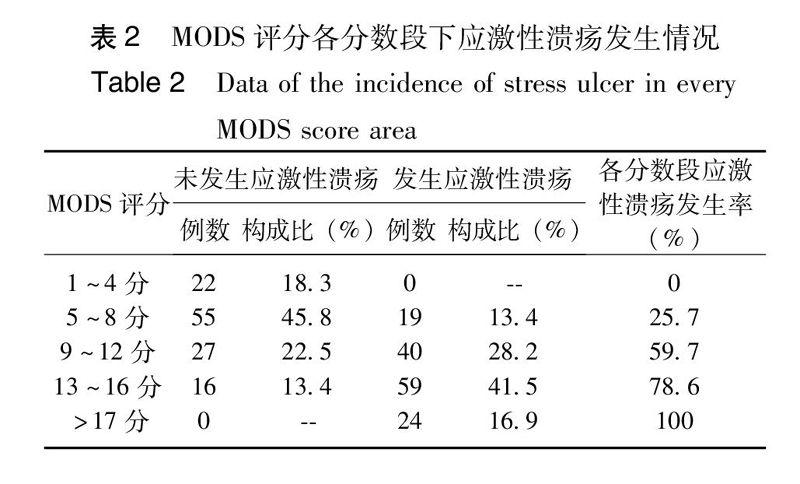
结果 Spearman相关系数为0.693(P<0.01),ROC下面积为0.793(P<0.01),预测应激性溃疡的MODS评分最佳临界值为9分。
结论 MODS评分能在一定程度上预测应激性溃疡的发生,MODS评分>9分时应进行应激性溃疡的预防治疗。
【关键词】 应激性溃疡;多器官功能障碍综合征;病情严重度;评分;相关性;预防;重症监护病房;回顾性研究;发生率
Study of the correlation between MODS score and incidence of stress ulcer Lin Jinfeng,Yang Zhizhou,Shao Danbing, Liu Hongmei, Zhang Wei, Ren Yi, Sun Zhaorui, Tang Wenjie, Nie Shinan. Emergency Medicine,Jinling Hospital, Medical School of Nanjing University, Nanjing,210002China
Corresponding author: Nie Shinan, Email: shn_nie@sina.com
【Abstract】Objective To investigate the incidence of stress ulcer in MODS patients in order to find a rationale for prophylaxis. Methods Clinical data of two hundred and sixty-two patients met the MODS diagnosis criterionadmitted to our EICU from August 2008 to August 2012 were retrospectively analyzed. The MODS score criterion proposed by Marshall was used to estimate all MODS patients. The stress ulcer was identified according to the diagnosis criterion of stress ulcer. Correlation between the score and incidence of stress ulcer was studied by rank test. The validity of MODS score to predict the incidence of stress ulcer was to verify with ROC. Optimization of critical value was obtained by Youden's index. ResultsSpearman correlation coefficient was 0.693 (P<0.01).The area under the ROC was 0.793 (P<0.01). The optimized critical value to predict the incidence of stress ulcer was 9.Conclusions The incidences of stress ulcer can be predicted to a certain extent by MODS score. Stress ulcer prophylaxis is necessary when the MODS score is above 9.
【Key words】Stress ulcer;Multiple organ dysfunction syndrome;Severity;Score;Correlation;Prophylaxis;Intensive care unit;Retrospective study;Incidence
据统计,每年约440万患者入住重症监护病房(ICU),ICU患者的病死率约为12%[1]。危重症患者的应激性溃疡的发生率从6%至100%不等[2]。在危重症患者发病的1至3天,使用胃镜检查可发现大约75%至100%的患者出现胃黏膜损伤[3]。以粪隐血试验阳性或不明原因的血红蛋白下降作为诊断标准,危重症患者的应激性溃疡的发生率在15%至50%[3-4]。未接受预防治疗的危重症患者的应激性溃疡伴明显出血(呕血或引流液为鲜红色)的发生率在5%至25%[4, 6, 8],这使应激性溃疡的预防和治疗显得十分重要。要对应激性溃疡进行有效的预防,首先要准确预测应激性溃疡的发生。呼吸衰竭、凝血功能障碍、低血压、脓毒症、肝衰竭、肾衰竭、手术、烧伤、严重创伤可导致应激性溃疡的发生[6],因此,对伴有器官功能障碍的患者需提高警惕。1995年加拿大学者Marshall提出的MODS评分标准能准确地反映器官功能障碍的严重程度且评分参数少、程序简单,被广泛应用于临床[7]。本科自2000年以来将该评分标准应用于临床,取得了较好的效果。本文通过回顾性研究分析南京军区南京总医院EICU的262例MODS患者的临床资料,计算应激性溃疡的发生率,并结合患者入院时的MODS评分进行分析,探讨MODS评分在预测应激性溃疡发生中的作用,为临床早期预防提供理论依据。
多器官功能障碍的患者容易并发应激性溃疡,但目前尚无多器官功能障碍的严重程度与应激性溃疡发生的相关性研究。Marshall的MODS评分系统涉及呼吸、肾脏、肝脏、心血管、凝血、神经等系统,通过量化氧合指数、格拉斯哥评分、肌酐、总胆红素浓度等指标进行评分,能准确反映MODS患者病情严重程度[7]。MODS患者处于严重的应激状态,导致MODS的原发疾病和MODS本身可作为应激源引发应激性溃疡,MODS越严重,应激性溃疡的发生率越高[11]。本文通过回顾性研究分析本院EICU的262例MODS患者的临床资料,发现MODS评分与应激性溃疡的发生存在正相关关系(Spearman相关系数为0.693,P<0.01), MODS评分越高,发生应激性溃疡的风险越大,MODS评分能较准确的预测应激性溃疡的发生(ROC 下面积为0.793),能在一定程度上为临床合理的早期预防提供理论依据。对于MODS评分>9分的患者,应积极采取措施预防应激性溃疡。
参考文献
[1]Fennerty MB. Pathophysiology of the upper gastrointestinal tract in the critically ill patient: rationale for the therapeutic benefits of acid suppression[J]. Crit Care Med, 2002, 30(6): S351-S355.
[2]Choung RS, Talley NJ. Epidemiology and clinical presentation of stress-related peptic damage and chronic peptic ulcer[J]. Curr Mol Med, 2008, 8(4): 253-257.
[3]Shuman RB, Schuster DP, Zuckerman GR. Prophylactic therapy for stress ulcer bleeding: a reappraisal[J]. Ann Intern Med, 1987, 106(4): 562-567.
[4]Duerksen DR. Stress-related mucosal disease in critically ill patients[J]. Best Pract & Res Clin Gast, 2003, 17(3): 327-344.
[5]Mutlu GkM, Mutlu EA, Factor P. GI complications in patients receiving mechanical ventilation[J]. Chest, 2001, 119(4): 1222-1241.
[6]Cook DJ, Fuller HD, Guyatt GH, et al. Risk factors for gastrointestinal bleeding in critically ill patients[J]. N Engl J Med,1994, 330(6): 377-381.
[8]Marshall JC, Cook DJ, Christou NV, et al. Multiple organ dysfunction score: a reliable descriptor of a complex clinical outcome[J]. Crit Care Med, 1995, 23(10): 1638-1652.
[9]Cook DJ, Griffith LE, Walter SD, et al. The attributable mortality and length of intensive care unit stay of clinically important gastrointestinal bleeding in critically ill patients[J]. Crit Care, 2001, 5(6): 368-375.
[10]Skillman J, Silen W. Acute gastroduodenal" stress" ulceration: barrier disruption of varied pathogenesis [J]. Gastro, 1970, 59(3): 478-482.
[11]Ali T, Harty RF. Stress-induced ulcer bleeding in critically ill patients[J]. Gastroenterol Clin North Am, 2009, 38(2): 245-265.
[12]Ellison RT, Perez-Perez G, Welsh CH, et al. Risk factors for upper gastrointestinal bleeding in intensive care unit patients: role of helicobacter pylori[J]. Crit Care Med, 1996, 24(12): 1974-1981.
[13]楊兴易, 谢伟峰, 王东. 多器官功能障碍综合征的诊治[J]. 中华急诊医学杂志, 2007, 16(12): 1343-1344.
[14]柴家科, 盛志勇. 烧伤脓毒症与多器官功能障碍综合征临床防治的现状与思考[J]. 中华烧伤杂志, 2008, 24(5): 378-380.
[15]贾林, 李瑜元. 应激性溃疡及其防治策略[J]. 中华急诊医学杂志, 2002, 11(5): 358-359.
[16]McCarthy DM. Sucralfate[J]. N Engl J Med, 1991, 325(14): 1017-1025.
[17]Tryba M, Cook D. Current guidelines on stress ulcer prophylaxis[J]. Drugs, 1997, 54(4): 581-588.
[18]Hastings PR, Skillman JJ, Bushnell LS, et al. Antacid titration in the prevention of acute gastrointestinal bleeding: a controlled, randomized trial in 100 critically ill patients[J]. N Engl J Med, 1978, 298(19): 1041-1047.
[19]Feldman M, Burton M. Histamine2-receptor antagonists. Standard therapy for acid-peptic diseases. 1[J]. N Engl J Med, 1990, 323(24): 1672-1678.
[20]Baghaie AA, Mojtahedzadeh M, Levine RL, et al. Comparison of the effect of intermittent administration and continuous infusion of famotidine on gastric pH in critically ill patients: results of a prospective, randomized, crossover study[J]. Crit Care Med, 1995, 23(4): 687-691.
[21]Cook DJ, Witt LG, Cook RJ, et al. Stress ulcer prophylaxis in the critically Ⅲ: a meta-analysis[J]. Am J Med,1991, 91(5): 519-527.
[22]孙洁, 曾霈君, 魏惠芳. 电针不同经穴对束缚应激模型大鼠行为学影响的实验观察[J]. 医学研究生学报, 2012, 25(10): 1027-1031.
[23]Moore JG, Coburn JW, Sanders MC, et al. Effects of sucralfate and ranitidine on aluminum concentrations in elderly volunteers[J]. Pharm, 1995, 15(6): 742-746.
[24]Burgess E, Muruve D, Audette R. Aluminum absorption and excretion following sucralfate therapy in chronic renal insufficiency[J]. Am J Med,1992, 92(5): 471-475.
[25]Laheij RJ, Sturkenboom MC, Hassing R-J, et al. Risk of community-acquired pneumonia and use of gastric acid–suppressive drugs[J]. JAMA, 2004, 292(16): 1955-1960.
[26]Cunningham R, Dale B, Undy B, et al. Proton pump inhibitors as a risk factor for Clostridium difficile diarrhoea[J]. J Hosp Infect, 2003, 54(3): 243-245.
[27]Tryba M. Risk of acute stress bleeding and nosocomial pneumonia in ventilated intensive care unit patients: sucralfate versus antacids[J]. Am J Med, 1987, 83(3): 117-124.
[28]Driks MR, Craven DE, Celli BR, et al. Nosocomial pneumonia in intubated patients given sucralfate as compared with antacids or histamine type 2 blockers[J]. N Engl J Med, 1987, 317(22): 1376-1382.
(收稿日期:2014-02-14)
(本文編辑:何小军)
P847-851
