老年恶性肿瘤患者甲状腺功能状态及化学药物疗法对其的影响
2014-07-19邹春华黄涛金谢勇久
邹春华,黄涛金,谢勇久,林 争,王 绎,明 华
老年恶性肿瘤患者甲状腺功能状态及化学药物疗法对其的影响
邹春华,黄涛金,谢勇久,林 争,王 绎,明 华
目的 探讨老年恶性肿瘤患者的甲状腺功能状态及化学药物疗法(简称化疗)对其甲状腺功能的影响。方法 选取2010-01至2014-02确诊的老年恶性肿瘤患者398例,并选择400例体检老年人群作为健康对照组,进行甲状腺激素(thyroid hormone,TH)和促甲状腺激素(thyroid stimulating hormone,TSH)水平测定。将激素水平正常,KPS (Karnofsky)评分>60的老年恶性肿瘤患者分为: 肿瘤治疗组132例,肿瘤对照组 129例。两组年龄、KPS评分无统计学差异。肿瘤治疗组患者进行相应化疗,观察治疗前及治疗后6个月的TH和TSH水平,肿瘤对照组仅给予对症治疗,同期比较两组TH和TSH水平,分析化疗对老年恶性肿瘤患者甲状腺功能的影响。结果 398例老年恶性肿瘤患者的TH、TSH与健康对照组相比差异无统计学意义(P>0.05)。肿瘤治疗组患者的TH、TSH与肿瘤对照组相比,TSH的差异存统计学意义(P<0.05)。肿瘤治疗组中甲状腺功能减退(甲减)的比例为7.58%,亚临床型甲减的比例为23.48%。肿瘤对照组中甲减的比例为5.65%,亚临床甲减的比例为5.65%。两组比较,亚临床型甲减的发生率存在统计学差异(P<0.05)。结论 老年恶性肿瘤患者的甲状腺功能异常发生率与健康群体比较无统计学差异,化疗对老年恶性肿瘤患者的甲状腺功能有一定的影响。
恶性肿瘤;老年;甲状腺激素;甲状腺功能亢进;甲状腺功能减退
恶性肿瘤严重威胁着人类的健康,随着人口的老龄化,相当多的老年恶性肿瘤患者被确诊。老年恶性肿瘤患者伴随的多种疾病、内分泌失调等因素对治疗有一定的影响。甲状腺是人体的重要内分泌器官,TH参与机体的新陈代谢[1,2]。本研究对老年恶性肿瘤患者进行TH和TSH水平测定,并就与化疗因素相关的甲状腺功能进行分析,以探讨在老年恶性肿瘤患者的甲状腺功能状态。
1 对象与方法
1.1 对象 选取2010-01至2014-02确诊的老年恶性肿瘤患者 398例,男203例,女195例,平均(72.1±5.1)岁;其中肺癌197例,恶性淋巴瘤 82例,食管癌 14例,胃癌37例,结肠癌 63例,鼻咽癌5例。选择400例正常体检老年人群作为对照组,男208例,女192例,平均(73.9±4.8)岁。对有如下病况者进行排除:有甲状腺功能亢进(甲亢)或甲状腺功能减退(甲减)病史、甲状腺癌、甲状腺手术史;近期服用抗甲状腺药物、乙胺碘呋酮、糖皮质激素;曾进行放射性碘治疗。398例恶性肿瘤患者中,TH水平正常且KPS评分>60的老年恶性肿瘤患者261例,此261例患者根据其意愿分为: 肿瘤治疗组132例,男70例,女62例, 65~79岁,平均(73.5±5.6)岁;肿瘤对照组 129例, 男70例,女59例, 65~78岁,平均(74.7±4.7)岁。其余137例患者存在TH水平异常和(或)KPS评分≤60,则予以排除。
两组年龄、KPS评分差异无统计学意义(P>0.05)。肿瘤治疗组患者进行相应化疗,观察治疗前及治疗后6个月的TH和TSH水平,肿瘤对照组仅给予对症治疗,同期观察TH和TSH水平。
1.2 方法 抽取研究对象空腹肘正中静脉血3 ml,静置30 min后,常规离心5 min,分离血清备用。采用化学发光法检测,严格按仪器操作手册,用配套试药盒,进行TH和TSH测定。
1.3 评定标准 甲减:血清TH降低伴TSH升高;亚临床甲减:血清TH正常,仅存在TSH升高;甲亢:血清TH升高伴TSH降低;亚临床甲亢:血清TH正常,仅存在TSH降低。

2 结 果
2.1 肿瘤患者与正常体检老年人群比较 肿瘤组游离三碘甲状腺原氨酸(FT3)、游离甲状腺素(FT4)、总三碘甲状腺原氨酸(TT3)、总甲状腺素(TT4)及TSH与健康对照组相比差异无统计学意义(表1)。肿瘤组甲状腺功能异常者45例,其中甲亢7例,亚临床甲亢7例,甲减13例,亚临床甲减18例;对照组甲状腺功能异常者45例,其中甲亢5例,亚临床甲亢9例,甲减15例,亚临床甲减16例。两组患者甲状腺疾病异常率比较差别无统计学意义(P>0.05)。
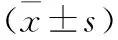
甲状腺功能老年肿瘤组(n=398)健康对照组(n=400)tPTSH(μU/ml)3.78±1.243.65±1.671.250.21FT3(pmol/L)4.45±1.414.63±1.371.830.07FT4(pmol/L17.2±3.6715.8±4.011.470.14TT3(nmol/L)1.96±0.572.03±0.441.940.06TT4(nmol/L)137.04±16.92134.99±13.581.890.06
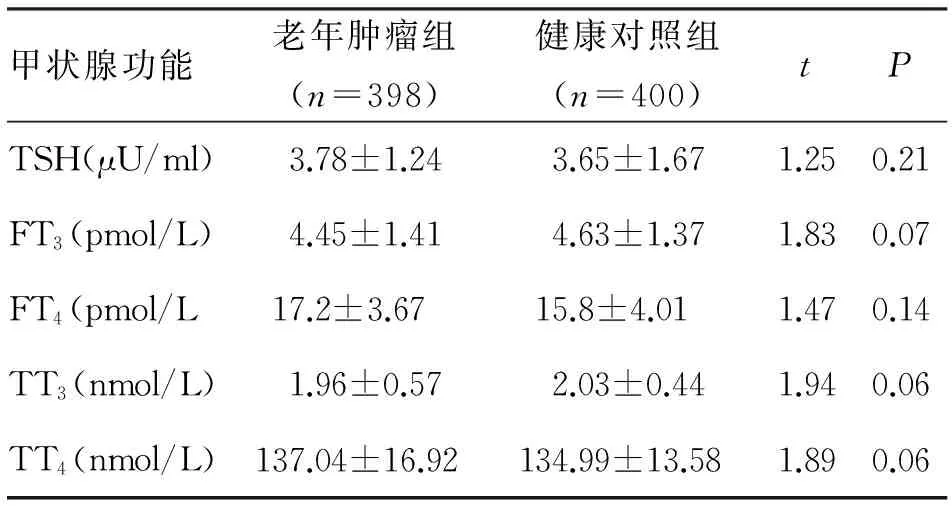
2.2 治疗组与对照组比较 治疗6个月后,肿瘤治疗组与肿瘤对照组比较,FT3、FT4、TT3、TT4差异无统计学意义。TSH差异存统计学意义(P<0.05,表2)。
甲状腺功能肿瘤治疗组(n=132)肿瘤对照组(n=129)tPTSH(μU/ml)4.05±2.272.59±0.916.79<0.001FT3(pmol/L)4.72±0.994.92±0.571.960.067FT4(pmol/L)16.20±4.1517.10±3.631.840.060TT3(nmol/L)2.36±0.992.57±0.771.8910.118
2.3 对完成化疗的132例分析 经检测分析显示,肿瘤治疗组中甲减的比例为7.58%,亚临床型甲减的比例为23.48%,甲亢的比例为1.51%,亚临床型甲亢的比例为2.27%。肿瘤对照组中甲减的比例为5.65%,亚临床甲减的比例为5.65%,甲亢的比例为1.61%,亚临床甲亢的比例为3.23%。两组比较,亚临床型甲减的发生率存在统计学差异(P<0.05)。
3 讨 论
本研究通过对老年恶性肿瘤患者进行TH和TSH水平进行测定,并未发现老年恶性肿瘤患者的甲状腺功能与健康对照组存在统计学差异。通过对KPS评分>60分,甲状腺功能正常老年恶性肿瘤患者进行相应化疗干预,观察治疗前及治疗后TH和TSH水平,分析患者甲状腺功能。结果显示132例可以纳入分析的老年恶性肿瘤患者中甲减为7.58%;亚临床甲减为23.48%;甲亢为1.51%;亚临床甲亢的为2.27%。显示老年恶性肿瘤患者进行化疗干预后甲状腺功能异常以亚临床甲减的患病率最高。老年恶性肿瘤患者进行化疗干预后的甲状腺功能与其对照组存在统计学差异,本研究结果与Huang等[3]的研究结论基本一致,说明化疗对老年患者甲状腺功能有一定的影响。
亚临床甲减症(又称轻度甲状腺衰竭)是指血清 TSH水平高于正常值上限,而FT4、FT3在正常范围,不伴或伴轻微非特异的甲减症状[4]。亚临床甲减主要依赖于实验室诊断。近年来,随着激素测定技术水平的提高,亚临床甲减的检出率明显增高。亚临床甲减的患病率4%~10%,随年龄增长而增高[5]。由于亚临床甲减病情隐匿,通常没有或仅有轻微的临床症状,因此老年人甲减诊断相对困难,常引起动脉粥样硬化、血脂异常及心功能不全等不良事件,在原本就存在基础心脏疾病的老年患者这些心血管风险则进一步扩大,造成很多危害[4,6]。本研究发现,老年恶性肿瘤患者甲状腺功能异常的患病率主要以亚临床甲减为主,进行化疗干预后甲状腺功能异常以亚临床甲减的患病率最高。
目前认为,亚临床甲减的病因包括自身免疫性甲状腺疾病,物理性、药物性或放射性因素损伤甲状腺[4]。笔者对激素水平正常老年恶性肿瘤患者进行相应化疗干预,对完成化疗可纳入的患者进行分析,甲状腺功能异常以亚临床甲减最高,其亚临床甲减发生率为23.48%。笔者认为,其原因可能包括药物性甲状腺损伤、自身免疫性甲状腺疾病,即由于较高的药物浓度或药物代谢致免疫系统异常,或老年人免疫功能紊乱引起,尚需进一步进行相关研究。近年有文献[7,8]报告,肿瘤治疗相关性甲减,部分肾细胞癌患者经酪氨酸激酶抑制药舒尼替尼治疗呈现甲减表现,与甲状腺功能正常的患者比较显现其生存期延长。有作者认为,甲减是某些抗癌药物的常见不良反应,对于癌症患者预后的有潜在效果[9]。在头颈部癌的临床研究中,甲减患者比甲状腺功能正常的患者表现为较长的生存期[10]。自发或故意诱发的甲状腺功能减退症可能与更好的临床反应率和患者生存期延长相关。
研究也发现,在老年恶性肿瘤患者中有出现甲状腺功能正常的病态综合征(euthyroid sicyndrome,ESS,低T3综合征)约 49例(12.31%)。甲状腺功能正常的病态综合征实验室检查示T3减低,血清总T4正常或轻度增高,而TSH正常[11]。考虑系因部分老年恶性肿瘤患者为肿瘤4期并存恶病质,可能是机体的一种保护性反应,而非甲状腺本身病变,属非甲状腺疾病综合征。
本研究结果需进一步分层分析,追踪亚临床甲状腺功能减退症是否进展为临床甲状腺功能减退及甲状腺功能与肿瘤预后相关性。总之,对老年恶性肿瘤患者进行甲状腺功能检测对指导治疗及判断预后有一定的意义。
[1] Hellevik A I, Asvold B O, Bjøro T,etal. Thyroid function and cancer risk: a prospective population study [J]. Cancer Epidemiol Biomarkers Prev, 2009, 18(2):570-574.
[2] Moeller L C, Führer D.Thyroid hormone, thyroid hormone, receptors, and cancer: a clinical perspective [J]. Endocr Relat Cancer, 2013, 20(2):19-29.
[3] Huang J, Jin L, Ji G,etal. Implication from thyroid function decreasing during chemotherapy in breast cancer patients: chemosensitization role of triiodothyronine[J]. BMC Cancer, 2013,13:334.
[4] Cooper D S, Biondi B. Subclinical thyroid disease [J]. Lancet, 2012, 379(9821): 1142-1154.
[5] 徐家琴,康冬梅,胡世莲. 老年亚临床甲状腺功能减退临床研究进展[J].国际老年医学杂志,2010,31(1):29-33.
[6] 陈少华,蒋群湘,杨 坤. 亚临床甲状腺功能减退症与特殊人群[J].中国医师杂志,2013,15(1):138-140.
[7] Sabatier R, Eymard J C, Walz J,etal. Could thyroid dysfunction influence outcome in sunitinib-treated metastatic renal cell carcinoma? [J]. AnnOncol, 2012,23(3):714-721.
[8] Clemons J, Gao D, Naam M,etal. Thyroid dysfunction in patients treated with sunitinib or sorafenib[J]. Clin Genitourin Cancer, 2012, 10(4):225-231.
[9] Hamnvik O P, Larsen P R, Marqusee E. Thyroid dysfunction from antineoplastic agents [J]. J Natl Cancer Inst, 2011, 103(21):572-1587.
[10] Nelson M, Hercbergs A, Rybicki L,etal.Association between development of hypothyroidism and improved survival in patients with head and neck cancer[J]. Arch Otolaryngol Head Neck Surg, 2006,132(10):1041-1046.
[11] 杨丹英,赵咏桔.正常甲状腺功能病态综合征在不同疾病状态中的表现及治疗进展[J]. 国际内科学杂志,2009,36(12):710-714 .
(2014-07-17收稿 2014-10-22修回)
(责任编辑 岳建华)
Thyroid functional status in aged patients with malignant tumors and relationship with chemotherapy
ZOU Chunhua,HUANG Taojin,XIE Yongjiu,LIN Zheng,WANG Yi,and MING Hua.
Department of Oncology, Chengdu Hospital of Sichuan Provincial Corps, Chinese People’s Armed Police Forces, Chengdu 610041, China
Objective To study thyroid functional status of the aged patients with malignant tumors and the relationship between thyroid function with chemotherapy. Methods 398 aged patients with malignant tumors were recruited as the pathological group. At the same time, 400 aged healthg subjects served as the control group. The thyroid hormones (thyroid hormone, TH), and thyrotropin (thyroid stimulating hormone, TSH) levels were measured. The thyroid function in the groups was analyzed and compared. When KPS score is over 60, the aged patients with malignant tumors in normal hormone levels were divided into the observation group (132 cases) and the control group (129 cases).Two groups had no significant difference in the age and KPS score. The patients in the observation group were treated by chemotherapy and TH and TSH levels observed before treatment and 6 moths post-treatment. The patients in the control group were given symptomatic treatment, TH and TSH levels were observed over the same period. We compared thyroid hormone and thyroid hormone levels and analyzed the relationship between thyroid function with chemotherapy in the aged patients with malignant tumor. Results The thyroid hormone and thyroid stimulating hormone in 398 aged patients with malignant tumor were compared with those in the healthy control group, the difference was not statistically significant (P<0.05). The aged patients with malignant tumors in normal hormone levels were divided into the observation group and the control group. In observation group the hypothyroidism (hypothyroidism) ratio was 7.58%, the proportion of subclinical hypothyroidism was 23.48%, hyperthyroidism (hyperthyroidism) ratio was 1.51%, and subclinical hyperthyroidism ratio was 2.27%. In control group, the proportion of hypothyroidism was 5.65%, subclinical hypothyroidism ratio was 5.65%, hyperthyroidism ratio was 1.61% and subclinical hyperthyroidism ratio was 3.23%. In the observation group, the thyroid disease incidence rate was higher. Incidence of subclinical hypothyroidism in the two groups was significantly different (P<0.05). Conclusions The thyroid dysfunction in the aged patients with malignant tumor was not significantly different compared with the health control group. Chemotherapy in the aged patients with malignant tumor harms the thyroid function to some extent. The detection of thyroid function in the aged patients with malignant tumor has clinical significance.
malignant tumor; the aged; thyroid hormone; hyperthyroidism; hypothyroidism
邹春华,博士,主任医师, E-mail: zouchun_hua06@163.com
610041,武警四川总队成都医院肿瘤科
R730
