Correlative Factors for Organic Psychotic Symptoms in Patients Following Traumatic Brain Injury
2014-05-21HANGRonghuaXUYajunZHUXuyan
HANG Rong-hua ,XU Ya-jun ,ZHU Xu-yan
(1.Department of Psychology,Wannan Medical College,Wuhu 241002,China;2.Department of Forensic Medicine,Wannan Medical College,Wuhu 241002,China)
Introduction
Although in the latest years there are a growing number of applications for jurisdictional assessment of mental disability due to craniocerebral trauma,current criteria for rating of the impairment are affected by many factors[1].How to evaluate the classification,the degree of trauma and influencing factors of the mental disorder is an urgent problem demanding a prompt solution in forensic expertise.
Organic mentaldisordersfollowing traumatic brain injury (TBI) can involve a variety of clinical manifestations such as organic amnesic syndrome,organic intellectual impairment,organic personality change,organic mood disorders,organicneurotic syndrome and psychotic syndrome[2].While organic psychotic syndrome is rare,it is likely to affect the prognosis and social skills more seriously than the other mental disorders[3].Domestically,few researches have been done on the organic psychotic syndrome due to craniocerebral injury;therefore little knowledge is available on the related underlying mechanisms and the influencing factors.In order to supply evidences for forensic appraisal of TBI-related mental impairment,the current study was undertaken to investigate the pertinent influencing factors through the analysis of the data gathered from 52 patients,who had sought for judicial assessment of the mental disease at our center,with organic mental symptoms following TBI.
Subjects and methods
Subjects
The totalpatients soughtforassessmentof mental disorders in the Forensic Science Identification Center of Wannan Medical College were enrolled between January 2010 and December 2012.
Inclusion criteria consisted of organic mental disorder following TBI with history of consciousness disorders to a certain extent and scoring lower than 15 by Glasgow Coma Scale (GCS) as previously described[4].All cases underwent definite imaging diagnosis,and received identification 6-18 months after brain injury.Eligible were 391 patients primarily for organic psychosis as the diagnostic criteria specified in the Chinese Classification of Mental Disorders 3rd version (CCMD-3).The data were collected in the 52 cases diagnosed as organic psychotic symptoms.The patients were excluded if they had any history of psychosis and disease of the central nervous system,a positive family history of psychosis,so were those who were incapable of completing the examination because of severe physical disability or serious somatic trauma.
Methods
The forensic psychiatrist was committed to collecting the demographic information,causes of the accident,post-trauma conditions,and case history and history of auxiliary examinations from the patients.The interview and assessment were carried out based on the information forthe premorbid personality,history of the past illness,daily behavior and social functioning of the examinees supplied by either their relatives or witnesses,with an attempt to exclude the disguise.
Statistical analysis
The total data were analyzed and assessed for the difference using t-test,χ2test and multivariate logistic regression with SPSS 16.0 software for windows,and P values below 0.05 were considered significant.
Results
The incidence rate for organic psychotic symptoms following TBI
In 391 cases with organic mental disorders following TBI,52 cases were identified as organic psychotic symptoms,which accounted for 13.3%of the cases with organic mental disorders.
Of the 52 cases,composed of 39 males and 13 females,aged from 18 to 65 years,41 were villagers and 11 were city dwellers;24 were had little schooling,16,junior schooling and 12,senior high schooling or above;8 were single,39,married,5,divorced or loss of mate.
Of the 52 cases diagnosed as organic psychotic symptoms,5 were characterized by hallucinations,6 by delusions,1 by catatonia and 40 by behavioral disorder.
The correlative factors for organic psychotic symptoms following TBI
A statistical analysis was made of the correlation ofdemographic characteristics with organic psychotic symptoms following TBI (Table 1).The organicpsychoticsymptomsmanifested differently in statistics with the marriage status (P=0.025),and the higher incidence of such symptoms was observed in those divorced or loss of mate than in those characterized by normal marriage,whereas the difference was not significant regarding the gender,age,education and residence.

Table 1 Correlation analysis of the demographic characteristics and incidence of organic psychotic symptoms following TBI [n(%)]
The analysis was made of the association of damage degree,injury severity,location,treatment,assessment schedule with organic psychotic symptoms(Table 2).In the post-TBI patients,the organic psychotic symptoms manifested differently in statistics with damage nature,injury severity and treatment.
The logistic regression analysis was performed to predict the outcomes based on whether there were psychotic symptoms or not as a dependent variable and the factors with statistical differences described previously as independent variables including marriage status,damage nature,injury severity and treatment.Consequently,treatment and injury severity were in goodness of model fit (Table 3).

Table 2 Correlation analysis of damage nature,injury severity,location,treatment and assessment schedule and incidence of organic psychotic symptoms following TBI [n(%)]
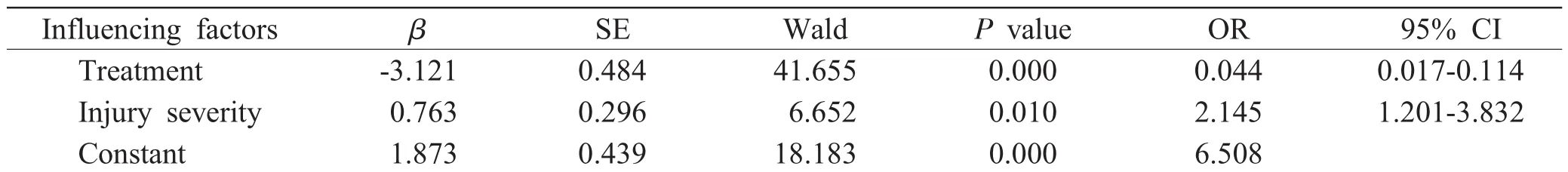
Table 3 Logistic regression analysis for organic psychotic symptoms in patients following TBI
Discussion
Our findings revealed that the organic psychotic symptoms were observed in patients with organic mental disorders following TBI by 13.3%,which was inconsistent with the results reported at home and abroad of 14.20%by Wang[5],8.9%by Gu[6]and 17.8%by Tan et al.[7]The discrepancy may be attributable to the constituent ratio of case origin to injury severity,sample size and judgment of forensic psychiatrist.
The mechanism underlying post-TBI related organic psychotic symptoms still remains unclear,yet resolution of the symptoms over time may vary because the results can be influenced by multi-factors including direct head injury,individual’s constitution and psychosocial adjustment[8].
It was found that marriage status was associated with the organic psychotic symptoms,fora higher incidence of such symptoms was observed in those divorced or loss of mate than those characterized by normal marriage.This can be ascribed to less availability of family supportand emotional difficulties due to dissolved partnership or loss of mate.Social support acted as one of the important psychosocial factor,and this was comparable to the conclusion by Riggio et al.[9]that poor social support availability was one of the potential reasons for organic psychotic symptoms after TBI.
A higher incidence of organic psychotic symptoms was found in those with brain contusion and laceration than in those with concussion,which can be interpreted by the association of such symptoms with the damaged cerebral structure,for impaired structures of the brain tissues are less likely expressed in cases with concussion.However,disorder of the cerebralfunction wasreported to appear temporarily reversible[10].In contrast,impaired brain structures exist to a certain degree in cases with contusion and laceration of the brain,leading to dissolved nerve cellsand degeneration neuroglial cells at the involvement region.Thus,it can be con-cluded that organic psychotic symptoms are more likely to occur in patients with brain contusion.
Other previous studies have described that psychotic symptoms are pertinent to the localization of injury,Ziauddeen et al.[11]reporting negative psychotic symptomsin frontallobe syndrome,and Borek et al.[12]confirming that right-sided injuries were associated with hallucinations,and left-sided injuries were associated with confabulation and lack of insight.
However,the current investigation failed to detect an incidence rate for specific damaged region and manifestation of organic mental symptoms.The dissimilarity may be the consequence of complex neurofunctional localization for the brain in examination,intricate relationship between the bilateral brain hemispheres or undetected injury at a certain site under diagnostic imaging.
The assessment schedule is critical to assessment of the disability in forensic expertise,for an authentic and objective conclusion can be interrupted if planned ahead of time or delayed,considering that the condition tends to be stable approximately six months after the accident,followed by slow and ambiguous recovery.Accordingly,a favorable schedule is to be planned in compliance with the severity of the trauma[13].Despite the fact that we found no association of the assessment schedule with presentation of organic psychotic symptoms,we observed that the assessment event occurred in six months of the injury in general,just at the end of the therapy,because of the eager requests from both the patient himself and his relatives.Given comprehensive factors,nevertheless,we recommend that the assessment program be optimally carried out six months after the accident in those with mild-moderate injury,and nine-twelve or beyond in the severe cases.
The regression analysis demonstrated that the contributing factors of organic psychotic symptoms were associated with the injury severity and treatment.
A few previous investigations have been conducted at home and abroad on whether the incidenceoforganic psychiatricsymptomsfollowing TBI has a positive correlation with the severity of traumatic brain injuries.Molloy et al.[14]reported that there was no dose-response relationship between injury severity and subsequent risk of psychotic symptoms;if ever,serious symptoms tended to be present in cases with more minor brain trauma.Contrarily,Yi et al.[15]insisted that organic psychotic symptoms were primarily present in severe cases.Our findings demonstrated that the incidences of organic psychotic symptoms were lower in those with mild brain injury,and comparable in moderate and severe cases.In general,the incidence appeared higher in those with moderate traumatic brain injuries than in those with severe ones.This may be ascribed to the immediately impaired physiological function and biochemical properties of the cerebral tissues due to either moderate or serious attack,thus causing disturbed mental activities.In addition,complications of cerebral ischemia and edema as well as elevated intracranial pressure secondary to the head injuries were responsible for the pathological changes in primary craniocerebral injury.It was reported thatthe moreseriousbrain injury was likely to result in a wide involvement,facilitating psychotic symptoms[6].Mental disorders in patients with mild traumatic brain injuries were reported to be primarily characterized by neurotic syndrome such as dizziness,debility and fatigue,whereas in severe casesthe symptomsare characterized by consciousness disorders at the acute stage,and psychotic disorders including hallucinations and delusions in the post-acute stage[16].However,the association of injury severity with manifestation of organic psychotic symptoms still needs to be investigated.
In the current study,we suggest that craniotomy in brain injury can be a risk factor for organic psychotic symptoms.This is possibly associated with the patient’s condition and surgical trauma in procedure.The severe cases generally require craniotomy rather than conservative therapy due to their emergencies.Additionally,risks of psychotic symptoms are attributable to moderate and severe head trauma.Although craniotomy assists in immediate removal of the hematoma and reducing the intracranial pressure,it takes longer time and results in larger trauma during operation,thus potentially damaging the normal brain structure,causing rehaemorrhagia and intracranial infection or other complications[17].Thus,secondary damage in procedure may be one of the causes of the presentation of organic psychotic symptoms.
In summary,TBI is one of the etiological factors for organic psychotic symptoms,and development of organic psychotic symptoms is involved in injury severity,treatment and some other subtle factors.Moreover,it seems difficult to assess the mental disorders and grade the disability for patients following TBI because of the complex etiology of mental symptoms and current lack of impersonal criteria,which has to be addressed in the further research of larger sample size.
Acknowledgements
The research was supported by the Development Fund for Key Scientific Research Project of Wannan Medical College (WK2012Z04).
[1]Zhang DK,Su QR,Zhang HW,et al.Related analy-sis of mental disability and retardation due to traffic brain injury[J].Fa Yi Xue Za Zhi,2009,25(6):428-430.
[2]沈渔邨.精神病学[M].第5版.北京:人民卫生出版社,2009:1016.
[3]陈军,宋晓静,王晓慧,等.56例交通事故颅脑损伤后法医精神病学鉴定分析[J].中国法医学杂志,2011,26(3):232-233.
[4]董为伟.实用临床神经病学[M].北京:中国医药科技出版社,2001:431.
[5]王婧琰.脑损伤所致精神障碍的相关因素研究[D].郑州:郑州大学基础医学院,2010.
[6]顾牛范.脑外伤引起的精神病[J].国外医学参考资料(精神病学分册),1976,(3):131-134.
[7]Tan CW,Wang ZZ,Xu JY,et al.Study of mental disorder due to brain damage[J].Fa Yi Xue Za Zhi,2008,24(5):339-341.
[8]Halbauer JD,Ashford JW,Zeitzer JM,et al.Neuropsychiatric diagnosis and management of chronic sequelae of war-related mild to moderate traumatic brain injury[J].J Rehabil Res Dev,2009,46(6):757-796.
[9]Riggio S,Wong M.Neurobehavioral sequelae of traumatic brain injury[J].Mt Sinai J Med,2009,76(2):163-172.
[10]Zhang JX,Zhai AL,Chen M,et al.Study on the correlative factors for mental disorder in patients with head injury[J].Chinese Journal of Forensic Medicine,2006,21(1):24-27.
[11]Ziauddeen H,Dibben C,Kipps C,et al.Negative schizophrenic symptoms and the frontal lobe syndrome:one and the same?[J].Eur Arch Psychiatry Clin Neurosci,2011,261(1):59-67.
[12]Borek LL,Butler R,Fleminger S.Are neuropsychiatric symptomsassociated with evidence ofright brain injury in referrals to a neuropsychiatric brain injury unit?[J].Brain Inj,2001,15(1):65-69.
[13]Tang T,Zhang QT,Cai WX,et al.Assessment time on mental disability due to brain damage[J].Fa Yi Xue Za Zhi,2009,25(1):27-32.
[14]Molloy C,Conroy RM,Cotter DR,et al.Is traumatic brain injury a risk factor for schizophrenia?A meta-analysis of case-controlled population-based studies[J].Schizophr Bull,2011,37(6):1104-1110.
[15]Yi QZ,Wang JY,Chen Q,et al.A comparative study of the clinical features of the psychiatric disorder after different seriously traumatic brain injury in the psychiatric expert testimony[J].Chinese Journal of Nervous and Mental Diseases,2005,31(6):430-434.
[16]Fleminger S.Neuropsychiatric effects of traumatic brain injury[J].Psychiatric Times,2010,27(3):40-45.
[17]胡斌,唐伟革,刘秀华.高血压脑出血128例临床治疗研究[J].医学信息,2011,24(5):15.
