Lesson Fifty-eight Is ST elevation in aVR a marker of LMCA or ostial LAD stenosis?
2014-05-16童鸿
●心电学英语
Lesson Fifty-eight Is ST elevation in aVR a marker of LMCA or ostial LAD stenosis?
The lead aVR is oriented to'look'at the right upper side of the heart,and can provide specific information about the right ventricle outflow tract and basal part of the septum.Because of its location and the fact that it displays reciprocal information covered by leads aVL,Ⅱ,V5and V6,lead aVR is often ignored,even when considering complex ECGs.

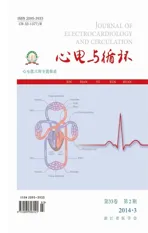
Figure 1Initial(A)and follow-up(B)electrocardiograms of a 44-year-old man presenting with chest heaviness and shortness of breath.Angiogram revealed a total proximal occlusion of the left anterior coronary artery without other significant disease.Note the ST elevation in aVR than V1.Also note the hyperacute T waves in the precardial leads and the ST abnormalities in the inferiolateral leads.
AcuteCoronarySyndromeandSTElevationinaVR
Studies by Engelen et al found that ST segment elevation in aVR strongly predicted LAD occlusion proximal to the first septal perforator(Figure 1).Yamaji et al observed that aVR ST segment elevation greater than the
ST segment elevation in V1predicts acute left main coronary artery(LMCA)occlusion with a sensitivity of
81%and a specificity of 80%(Figure 2).This finding also predicts clinical outcomes.Gaitonde et al demonstrated in a prospective study that in acute myocardial infarction,patients with an ST segment elevation that is greater in lead aVR than in lead V1prompted early angiography,withholding of clopidogrel and early referral to coronary artery bypass grafting,resulting in improved clinical outcomes1.
Kosuge et al found that in patients with non-ST segment elevation myocardial infarction,ST segment elevation of 0.5 mm or greater in aVR was a useful predictor of LMCA or three-vessel coronary artery disease(sensitivity 78%,specificity 86%)(Figure 3).Furthermore,they found that aVR ST segment elevation was the strongest predictor of adverse events at 90 days in patients with non-ST segment elevation myocardial infarction.Barrabes et al,in a study of 775 patients with theirfirst non-ST segment elevation myocardial infarction, showed that aVR ST segment elevation was associated with higher rates of in-hospital death,recurrent ischemia and heart failure.

Figure 2Electrocardiogram of a 71-year-old woman presenting with chest pain.Angiogram revealed high-grade stenosis of the distal left main coronary artery involving the take-offs of the left anterior descending and circumflex coronary arteries.Note the ST elevation in aVR and the diffuse ST depressions.
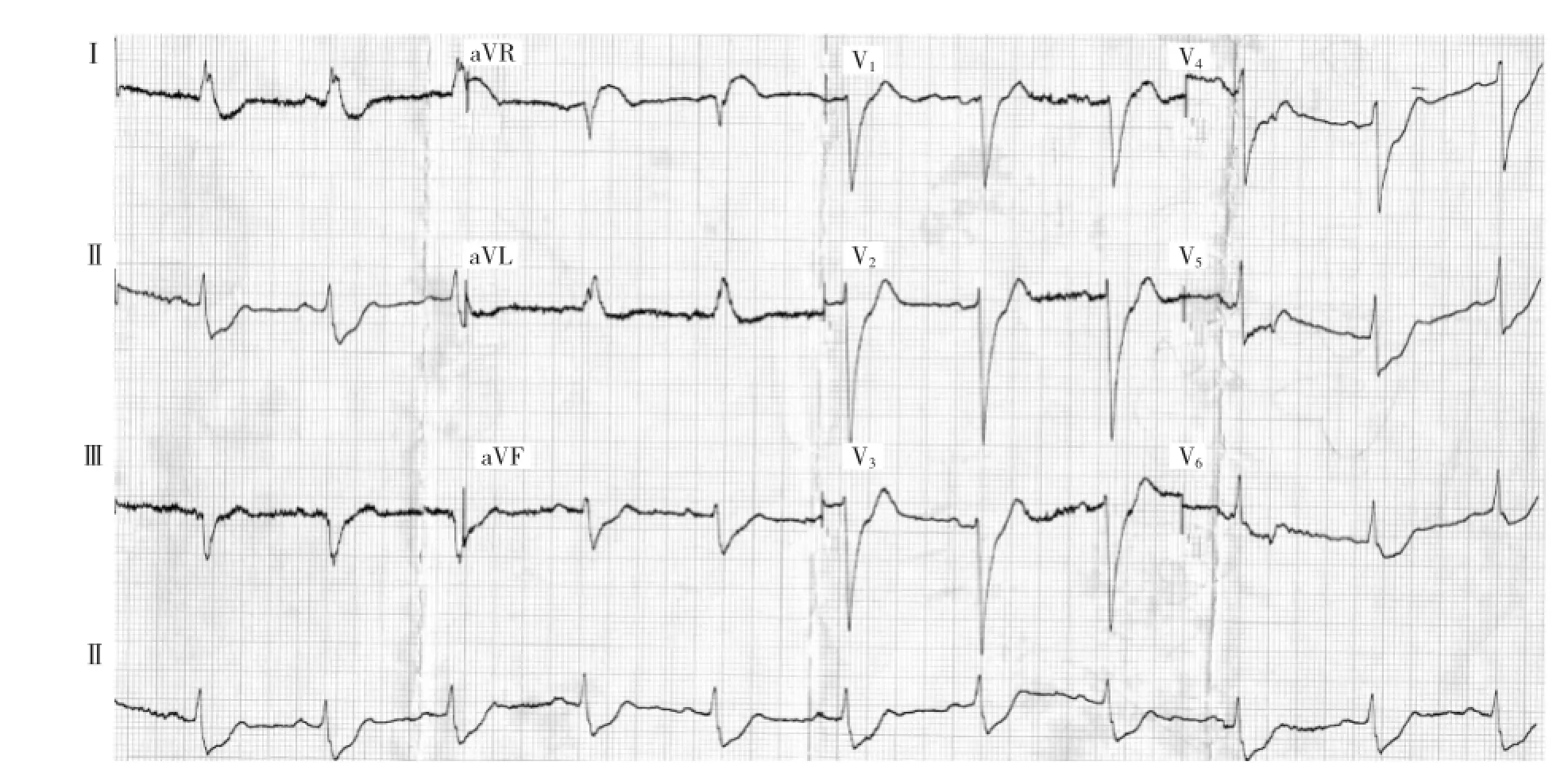
Figure 3Electrocardiogram of a 54-year-old man with chest pain and a history of coronary artery bypass surgery.Angiogram revealed an occluded left main coronary artery,a subtotal occlusion of the left anterior descending coronary artery after the anastamosis of left internal mammary artery,an ostial stenosis of saphenous vein graft to the obtuse marginal artery,and a diffuse moderate disease of the right coronary artery.Note the ST elevation in aVR and the ST depressions in the anterior and inferior leads.
Kotoku et al reported on the relationship between the ST segment level in lead aVR and the length of the LAD.ST segment levels(especially in leadsⅡand V6),the site of LAD occlusion and the length of the LAD affect the ST segment level in lead aVR in patients with a first ST elevation acute anterior wall myocardial infarction.Proximal LAD occlusion is associated with ST segment elevation in lead aVR,while a long LAD occlusion is associated with ST segment depression in lead aVR.Kotoku et al also reported that a prominent Q wave in lead-aVR in anterior wall acute myocardial infarction is related to severe regional wall motion abnormality in the apical and inferior regions,with an LAD wrapping around the apex2.
LMCA occlusion is another clinical situation in which prompt diagnosis by the clinician can help initiate life-saving invasive therapy.The typical electrocardiographic finding in patients with preserved flow through the LMCA is widespread ST segment depression maximally in leads V4to V6,with inverted T waves and ST segment elevation in lead aVR.ST elevation in lead aVR,when accompanied by either anterior ST elevationor widespread ST segment depression,may indicate LMCA occlusion.Figure 4 showed ECG changes of complete ostial occlusion of LMCA determined by emergent angiography.The ECG shows marked ST elevation in aVR>>V1and ST depression in multiple leads(V2~V6,Ⅰ,Ⅱ,aVL,aVF).
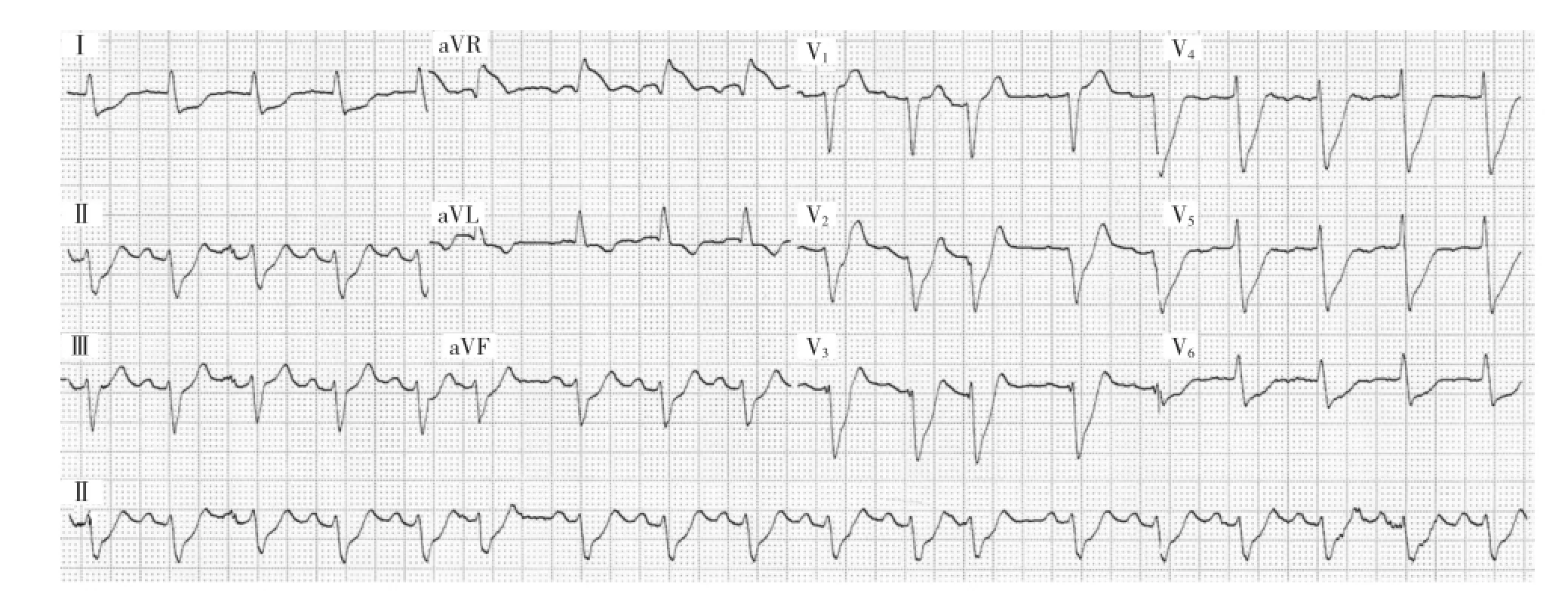
Figure 4This patient presented to ED with severe ischaemic chest pain,vomiting,syncope(due to runs of VT)and cardiogenic shock.He was taken for emergent angiography and found to have a complete ostial occlusion of left main coronary artery.
Kanei et al reported in a study of 106 patients that ST segment depression in lead aVR in inferior wall ST segment elevation myocardial infarction predicts left circumflex infarction or larger right coronary artery infarction involving a large posterolateral branch.
Stress Testing and ST Elevation in aVR
Data regarding the significance of STE in lead aVR in the setting of exercise treadmill testing(ETT)are limited.In the present study,Uthamalingam S et al tested the hypothesis that ETT-induced STE in lead aVR is a useful indicator of hemodynamically significant LMCA or ostial LAD stenosis.
A database search of patients undergoing cardiac catheterization at his institution between January 2008 and July 2009 was performed to identify 3 groups of patients∶1)those with significant LMCA or ostial LAD disease(≥50%luminal diameter reduction)in addition to any other coronary lesions(≥70%luminal diameter reduction for mid and distal LAD segments);2)those with coronary artery disease(CAD)(≥70%luminal diameter reduction)but not LMCA or ostial LAD disease;and 3)those free of significant CAD(LMCA and all 3 major vessels free of any stenosis≥50%). Ostial LAD stenosis included any lesion proximal to the first septal perforator.All patients(n=454)had undergone ETT according to the standard Bruce protocol≤6months beforetheclinicallyindicatedcardiac catheterization.LMCA(n=38)or ostial LAD stenosis(n=42)was present in 75 patients(5 patients had both).The remainder had either CAD of varying severity that did not involve the LMCA or ostial LAD(n= 276)or no significant CAD(n=103).
Patients with acute coronary syndromes or prior coronary artery bypass grafting were excluded.Patients who had undergone pharmacological stress also were excluded,as were those whose baseline ECG studies indicated left bundle branch block,intraventricular conduction delays≥120ms,left ventricular hypertrophy with marked strain pattern(down-sloping ST-segment depression[STD]≥1 mm with biphasic or inverted T waves),or marked anterior T-wave inversions(the Wellens pattern3)concerning for active ischemia or possible LMCA or proximal LAD stenosis.
ECG data(rest and stress)
In addition to lead aVR,lead aVL,the inferior leads(Ⅱ,Ⅲ,and aVF),and pre-cordial leads V1and V4to V6were evaluated,and the amount of STD or STE at 80 ms after the J point both at rest and during peak stress was tested in univariate regression analysis.In lead aVR,only horizontal or up-sloping STE was con-sidered indicative of ischemia.J-point elevation only with down-sloping ST segment was not.
Univariate logistic regression analysis was performed of patients with 1VD,2VD,and 3VD without LMCA or ostial LAD stenosis to determine the correlation of each with STE in lead aVR.There was no significant correlation between 1VD,2VD,or 3VD without LMCA or ostial LAD stenosis and STE in lead aVR.In contrast,STE in lead aVR was a significant(P<0.0001,AUC∶0.76)positively correlated predictor of selected cases of pure,isolated LMCA or ostial LAD stenosis(n=34).Because leads V5and V6are reciprocal to lead aVR,STD in either of these leads as a univariate predictor of LMCA or ostial LAD stenosis was determined.Although both were correlated strongly(lead V5:P<0.0001,AUC∶0.69;lead V6:P<0.0001,AUC:0.70),the AUC for each was significantly less than that for STE in lead aVR(0.82)(both P<0.001).Finally, although stress-induced STE in lead V1was also a significant predictor of LMCA or ostial LAD stenosis(P<0.0001,AUC∶0.59)it too was significantly less than that for STE in lead aVR(P<0.0001 for AUC comparison)and did not add independent information in multivariate analysis.
Using a cut-point of 1-mm STE in lead aVR, chi-square tests were used to compare the prediction of LMCA or ostial LAD stenosis with 1VD,2VD,and 3VD without LMCA or ostial LAD stenosis.Thus,76%of patients with LMCA or ostial LAD stenosis had 1-mm STE in lead aVR with stress,compared with 17%,27%,and 39%,respectively,with 1VD,2VD,and 3VD without LMCA or ostial LAD stenosis Only 8 patients(8%)without significant CAD had 1-mm STE in lead aVR with stress.
Optimal ECG lead aVR cut-point and Bayesian analysis
The optimal cut-point for the amount of stress-induced STE in lead aVR was defined by the greatest sum of sensitivity and specificity for the detection of significant LMCA or ostial LAD stenosis.Cut-points of 0.5-, 1.0-,1.5-,and 2.0-mm horizontal STE were tested. The greatest sensitivity-specificity sum(1.56)was reached at 1.0-mm STE.Thus,sensitivity was 75%, specificity was 81%,positive predictive accuracy was 44%,negative predictive accuracy was 94%,and overall predictive accuracy was 80%.
词汇
ignore v.忽视,不顾,不理会,驳回
withhold v.克制,使...停止,把...留下,拒给
wrap n.&v.包裹物,包装,披肩,毯子,外衣;包,包上,包扎,缠绕,覆盖,用...包
circumflex adj.&v.音调符号的,卷曲的,弯曲的;使...弯曲
univariate adj.单变量的
logistic n.&adj.算术;逻辑的,计算的
注释
1.句子“Gaitonde et al demonstrated…prompted early angiography,withholding of clopidogrel and early referral to coronary artery bypass grafting,resulting in improved clinical outcomes.”中,“withholding”是动名词作prompted的宾语,而“resulting…”是分词短语用作伴随状语。
2.句子“Kotoku et al also reported…the apical and inferior regions,with an LAD wrapping around the apex.”中的“wrapping…”分词短语是with宾语“LAD”的补语,而“with…”整个介词短语是“anterior wall acute myocardial infarction”的名词修饰语。
3.Wellens pattern指前降支严重狭窄的特异性心电图表现,V2~V3上出现对称性T波深倒置(>2mm)(A型Wellens T波),或T波呈先正后负的正负双相改变(B型Wellens T波)。
参考译文
第58课aVR ST段抬高是左冠状动脉主干或前降支开口狭窄的特征吗?
aVR面对心脏右上方,可提供右心室流出道和间隔基底部的特别信息。由于它的位置及其显示的信息与aVL、Ⅱ、V5和V6所覆盖的彼此相反,因此,即使分析复杂的心电图时,也常常忽视aVR。
急性冠状动脉综合征与aVR ST段抬高
Engelen等研究发现aVR ST段抬高强烈预示前降支(LAD)阻塞部位位于第一穿间隔支之前(图1)。Yamaji等观察到aVR ST段抬高超过V1预测急性左冠状动脉主干(LMCA)阻塞的敏感性为81%,特异性为80%(图2)。这种表现还能预测临床预后。Gaitonde等在一前瞻性研究中证实,急性心肌梗死时aVR ST段抬高超过V1者,促使早期造影、停用波利维及早期转向冠状动脉搭桥术,结果是临床预后得到改善。
Kosuge等发现非ST段抬高患者aVR ST段抬高0.5mm或以上是LMCA或多支冠状动脉病变的有效预测指标(敏感性78%,特异性86%)(图3)。此外,他们发现aVR ST段抬高是非ST段抬高心肌梗死患者90d不良事件的最强预测指标。Barrabes等对775例首次发生非ST段抬高心肌梗死患者的研究表明,aVR ST段抬高患者的住院死亡、再发心肌缺血及心力衰竭发生率较高。
Kotoku等对ST段水平与LAD长度之间的关系作了报道。对于首次ST段抬高急性前壁心肌梗死患者,ST段水平(特别是Ⅱ和V6)、LAD阻塞部位及LAD长度影响aVR ST段水平。LAD近端阻塞与aVR ST段抬高有关,而长的LAD阻塞与aVR ST段压低有关。Kotoku等也报道,在LAD包绕心尖部的急性前壁心肌梗死,aVR上明显的Q波与心尖及下壁区域严重局部心室壁运动异常相关。
LMCA阻塞是另一种临床状态,临床医师的即时诊断将有助于启动挽救生命的创伤性治疗。保留LMCA血流的患者,典型心电图表现为广泛ST段压低,V4~V6最明显,伴随aVR T波倒置和ST段抬高。aVR ST抬高,如伴随前壁ST段抬高或广泛ST段压低,提示LMCA阻塞。图4为经紧急血管造影证实LMCA开口完全阻塞的心电图变化。心电图显示aVR ST段明显抬高,明显超过V1,同时多个导联(V2~V6,Ⅰ,Ⅱ,aVL,aVF)ST段压低。
Kanei等对106例下壁ST段抬高心肌梗死患者研究显示,aVR ST段压低预示左旋支梗死或右冠状动脉梗死累及粗大的后外侧分支血管。
应力测试与aVR ST段抬高
有关运动平板试验(ETT)中涉及aVR ST段抬高意义的资料有限。本研究中,Uthamalingam等对ETT诱发的aVR ST段抬高是血流动力学上显著的LMCA或LAD开口狭窄的有效预测指标这一假设作了测试。
检索2008年1月至2009年7月他所在机构进行心导管检查的患者资料库,确定3组患者:(1)除其他冠状动脉病变LAD中远段狭窄≥70%外,有显著的LMCA或LAD开口病变(管腔狭窄≥50%);(2)有冠状动脉病变(狭窄≥70%),但无LMCA或LAD开口病变;(3)无明显冠状动脉病变(LMCA和所有三支血管无任何≥50%的狭窄)。LAD开口狭窄是指第一穿间隔支之前的任何LAD病变。所有患者(n=454)于临床心导管检查前≤6个月内按照Bruce方案进行ETT测试。LMCA(n=38)或LAD开口狭窄(n=42)者共75例(其中5例两者并存)。其余为未累及LMCA或LAD开口的各种严重程度的冠状动脉病变者(n=276),或无明显冠状动脉病变者(n=103)。
排除急性冠状动脉综合征或以前冠状动脉搭桥术。接受药物应力测试的、基础心电图提示左束支传导阻滞、室内传导延迟≥120ms、左心室肥大伴明显劳损性改变(下斜型ST段压低≥1mm伴T波双相或倒置)、或明显前壁T波倒置提示活动性缺血或LMCA或LAD近端狭窄可能的患者也排除在外。
ECG资料(静息与应力)
评估aVR及aVL、下壁导联(Ⅱ,Ⅲ,aVF)和胸前V1、V4~V6。对静息和峰值负荷时J点后80ms处ST段压低或ST段抬高数值作单因素回归分析。aVR上,认为只有水平型或上斜型ST段抬高为缺血表现。仅有J点抬高伴下斜型ST段抬高不考虑缺血。
对无LMCA或LAD开口狭窄的单支、双支和三支血管病变与aVR ST段抬高之间的相关性作单因素逻辑回归分析。无LMCA或LAD开口狭窄的单支、双支和三支血管病变与aVR ST段抬高之间无明显相关性。相反,aVR ST段抬高是所选患者(n=34)单纯LMCA或LAD开口狭窄的显著正相关指标(P<0.0001,AUC∶0.76)。因为V5和V6与aVR互为对应,因此,其中任一导联的ST段压低是LMCA或LAD开口狭窄的单变量预测指标。虽然两者均高度相关(V5:P<0.0001,AUC:0.69;V6:P<0.0001,AUC:0.70),但各自的AUC均显著低于aVR的ST段抬高(0.82)(均P<0.001)。最后,虽然应力诱发的V1ST段抬高也是LMCA或LAD开口狭窄的重要指标(P<0.0001,AUC∶0.59),但也是显著低于aVR ST段抬高(P<0.0001,由AUC对照),且不能为多变量分析增加独立的信息。
采用aVR ST段抬高1-mm作为分割点,作χ2检验来比较LMCA或LAD开口狭窄与无LMCA或LAD开口狭窄的单支、双支和三支血管病变的预测。这样,76%LMCA或LAD开口狭窄患者应力测试时出现1-mm ST段抬高。相比之下,无LMCA或LAD开口狭窄的单支、双支和三支血管病变患者分别为17%,27%和39%。只有8例无冠状动脉病变患者(8%)应力测试时aVR出现1-mm ST段抬高。
最佳心电图aVR分割点和贝叶斯分析
通过计算探测严重LMCA或LAD开口狭窄的敏感性和特异性的最大合计值确定应力测试诱发的aVR ST段抬高的最佳分割点。测试水平型ST段抬高0.5-,1.0-,1.5-,和2.0-mm的分割点。于ST段抬高1.0-mm点,敏感性和特异性合计值达到最大(1.56)。这样,敏感性为75%,特异性为81%,阳性预测准确性44%,阴性预测准确性94%,总体预测准确性80%。
图11例44岁男性因胸部沉闷和呼吸短促就诊时初始(A)和随访(B)心电图。造影显示LAD近端完全阻塞而无其他明显病变。注意aVR ST段抬高大于V1。另外,注意胸导联超急期T波和下壁导联ST段异常。
图271岁女性因胸痛就诊时的心电图。造影显示LMCA远端高度狭窄,累及LAD和LCX起始部位。注意aVR ST段抬高和广泛ST段压低。
图31例胸痛并有冠状动脉搭桥史的54岁男性心电图。造影显示LMCA阻塞、LAD内乳动脉吻合口远端次全阻塞,钝缘支大隐静脉口狭窄,RCA弥漫性中度病变。注意aVR ST段抬高及前壁和下壁ST段压低。
图4患者因严重缺血性胸痛、呕吐、晕厥(短阵室性心动过速所致)和心源性休克急诊。立即行血管造影检查发现LMCA开口完全阻塞。
[1]George A,Arumugham P S,Figueredo V M,et al.aVR-the forgotten lead[J].Exp Clin Cardiol,2010,15(2):e36-e44.
[2]Uthamalingam S,Zheng H,Leavitt M,et al.Exercise-Induced ST-Segment Elevation in ECG Lead aVR Is a Useful Indicator of Significant Left Main or Ostial LAD Coronary Artery Stenosis[J].J Am Coll Cardiol Img,2011,4(2):176-186.
(童鸿)