老年射血分数保留心力衰竭患者危险因素分析
2014-04-23黄樱硕
黄樱硕,张 健,王 丹,白 丽,杨 旭,黄 蔚,李 敏,孙 颖*
老年射血分数保留心力衰竭患者危险因素分析
黄樱硕1,张 健1,王 丹2,白 丽1,杨 旭1,黄 蔚1,李 敏1,孙 颖1*
(首都医科大学附属北京友谊医院:1医疗保健中心心血管内科,2输血科,北京 100050)
回顾性分析老年射血分数保留心力衰竭(HFpEF)患者的临床及超声心动图参数,与无症状舒张功能不全的非心衰患者比较,明确HFpEF的危险因素。入选2011年12月至2012年12月在首都医科大学附属北京友谊医院医疗保健中心心血管内科就诊的234例患者(年龄≥60岁),分为无症状舒张功能不全组(ADD组)104例和射血分数保留心力衰竭组(HFpEF组)130例。通过回归分析明确HFpEF的独立危险因素。与ADD组相比,HFpEF患者的平均年龄较大,估测的肾小球滤过率较低。logistic回归分析表明冠心病、高血压和慢性阻塞性肺疾病(COPD)是HFpEF的独立危险因素(=0.001,0.031,0.003)。老年患者中,冠心病、高血压和COPD与HFpEF相关。
老年人;射血分数保留心力衰竭;舒张功能不全
心力衰竭(简称心衰)是全世界老年人住院和死亡的主要原因之一。研究表明≥65岁老年人占心衰死亡>80%[1]。目前认为,射血分数保留心力衰竭(heart failure with preserved ejection fraction,HFpEF)在心衰患者中所占的比例约50%(40%~71%)[2],2012年欧洲心脏病学协会(European Society of Cardiology,ESC)心衰指南指出没有证据证明任何治疗能够减少HFpEF患者的发病率和病死率[3]。明确和了解从无症状舒张功能不全发展为心衰的过程尤其重要,通过早期预防和干预危险因素可能降低发病率及病死率[4,5]。既往研究往往将慢性阻塞性肺疾病(chronic obstructive pulmonary disease,COPD)作为排除标准,但临床实际中,COPD是老年HFpEF患者常见的合并疾病[6,7]。本研究旨在通过比较无症状舒张功能不全和HFpEF的临床特点及超声心动图特点,分析包括COPD在内的HFpEF老年患者的危险因素。
1 对象与方法
1.1 研究对象
入选2011年12月至2012年12月在首都医科大学附属北京友谊医院医疗保健中心心血管病房住院的234例老年患者(年龄≥60岁),所有患者入院时行超声心动图检查,基线左室射血分数(left ventricular ejection fraction,LVEF)均≥45%,记录患者的一般情况,合并疾病,实验室指标和用药情况。排除标准:LVEF<45%,瓣膜性心脏病,限制性心肌病,心肌炎,心包疾病。根据HFpEF诊断标准分为无症状舒张功能不全组(asymptomatic left ventricular diastolic dysfunction,ADD组)和射血分数保留心力衰竭组(HFpEF组)。
1.2 实验室检测
实验室检测项目包括血常规,估测肾小球滤过率(estimated glomerular filtration rate,eGFR),血脂,糖化血红蛋白(glycated hemoglobin A1c,HbA1c),血清N端脑钠肽前体(N-terminal pro-brain natriuretic peptide,NT-proBNP),超敏C反应蛋白(high-sensitivity C-reactive protein,hs-CRP)。
1.3 经胸超声心动图检测
经胸超声心动图检测包括M型、二维、多普勒及组织多普勒(tissue Doppler images,TDI)[8],采用Vivid7超声心动仪(GE Medical Systems,美国)。由同一名有经验的超声心动医师进行检测,患者的临床资料对超声心动医师保密。测量标准参考美国超声协会(American Society of Echocardiography)推荐[9]。左室质量根据Devereux公式计算[10]。左室质量指数(left ventricular mass index,LVMI)以左室质量除以体表面积计算。
1.4 诊断标准
HFpEF的诊断根据2013年美国心脏病学学会基金会(American College of Cardiology Foundation,ACCF)/美国心脏联合会(American Heart Association,AHA)心力衰竭诊治指南[11]:(1)心衰症状或体征;(2)保留或正常的LVEF值;(3)通过多普勒超声或心脏导管证实的异常左室舒张功能不全。COPD根据GOLD指南[12]诊断,冠心病根据冠状动脉造影或冠状动脉CT血管成像术(CTA)诊断。
1.5 统计学处理
所有数据采用SPSS13.0软件进行统计分析。计量资料以均数±标准差表示,组间比较采用检验。计数资料采用频数及百分数表示,组间比较采用2检验。建立logistic回归模型,采用逐步向后法分析HFpEF的独立危险因素。以<0.05为差异有统计学意义。
2 结 果
2.1 两组患者一般情况比较
两组患者间的一般情况、合并疾病、目前用药情况比较见表1。两组患者男女比例、BMI、合并高脂血症、糖尿病、房颤的发生率差异无统计学意义(>0.05)。HFpEF组患者年龄、吸烟比例、合并冠心病、高血压、慢性肾病、COPD发生率以及阿司匹林、硝酸酯类、利尿剂、血管紧张素转换酶抑制剂(angiotensin-converting enzyme inhibitor,ACEI)/血管紧张素受体拮抗剂(angiotensin receptor blockers,ARB)、β阻滞剂、醛固酮拮抗剂、钙通道阻滞剂、他汀类药物应用比率显著高于ADD组,且差异有统计学意义(<0.05,<0.01)。
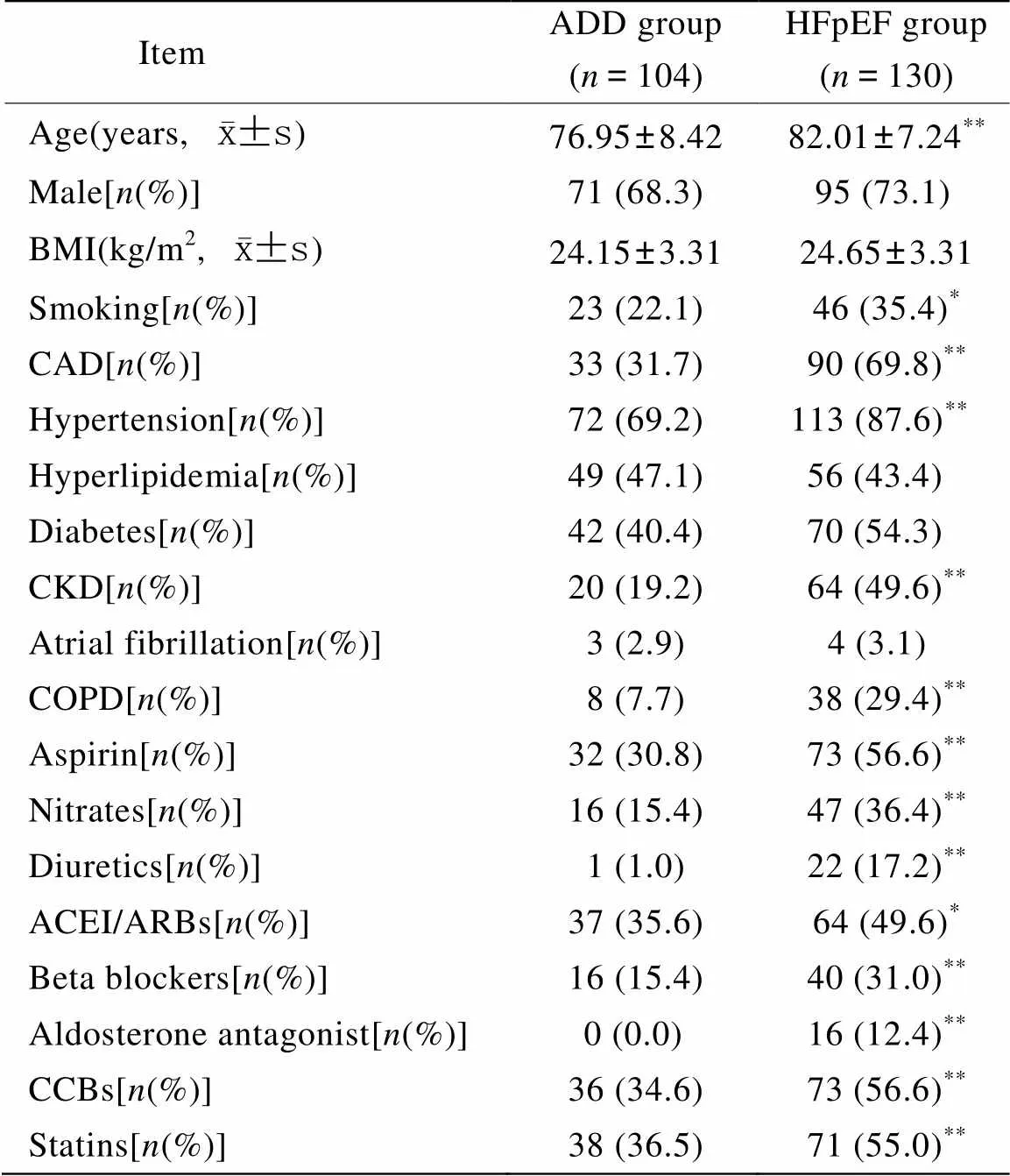
表1 无症状舒张功能不全及射血分数保留心力衰竭患者的一般情况
ADD: asymptomatic left ventricular diastolic dysfunction; HFpEF: heart failure with preserved ejection fraction; BMI: body mass index; CAD: coronary artery disease; CKD: chronic kidney disease; COPD: chronic obstructive pulmonary disease; ACEI: angiotensin-converting enzyme inhibitor; ARBs: angiotensin receptor blockers; CCBs: calcium channel blockers. Compared with ADD group,*<0.05,**<0.01
2.2 两组患者实验室指标比较
与ADD组比较,HFpEF组患者NT-proBNP水平较高(=0.004),eGFR、总胆固醇、低密度脂蛋白胆固醇和血红蛋白水平较低(分别为=0.000,0.009,0.007及0.001;表2)。
2.3 超声心动图指标
同ADD组相比,HFpEF组患者的左房内径、左室舒张末内径、左室收缩末内径、左室间隔厚度、左室后壁厚度、二尖瓣早期血流速度(E)/二尖瓣环的早期运动速度(e’)比值、左室质量、左室质量指数较高(<0.05,<0.01),LVEF、E/二尖瓣晚期血流速度(A)比值、e’较低(<0.05,<0.01;表2)。

表2 无症状舒张功能不全及射血分数保留心力衰竭患者的实验室指标及超声心动图参数比较
ADD: asymptomatic left ventricular diastolic dysfunction; HFpEF: heart failure with preserved ejection fraction; NT-proBNP: N-terminal pro-brain natriuretic peptide; HbA1c: glycated hemoglobin A1c; eGFR: estimated glomerular filtration rate; TC: total cholesterol; LDL-C: low-density lipoprotein cholesterol; hs-CRP: high-sensitivity C-reactive protein; AAD: ascending aorta diameter; LAD: left atrial diameter; LVEDD: left ventricular end-diastolic diameter; LVESD: left ventricular end-systolic diameter; LVEF: left ventricular ejection fraction; LVST: left ventricular septal thickness; LVPWT: left ventricular posterior wall thickness; RVDD: right ventricular diastolic diameter; E: peak early mitral flow velocity; A: peak late mitral flow velocity; e’: velocity of mitral annulus early diastolic motion; E/A: ratio of E to A; E/e’: ratio of E to e’; LVM: left ventricular mass; LVMI: left ventricular mass index. Compared with ADD group,*<0.05,**<0.01
2.4 HFpEF的危险因素
logistic回归分析结果见表3。经过调整混杂变量,冠心病、高血压和COPD是HFpEF的独立危险因素。
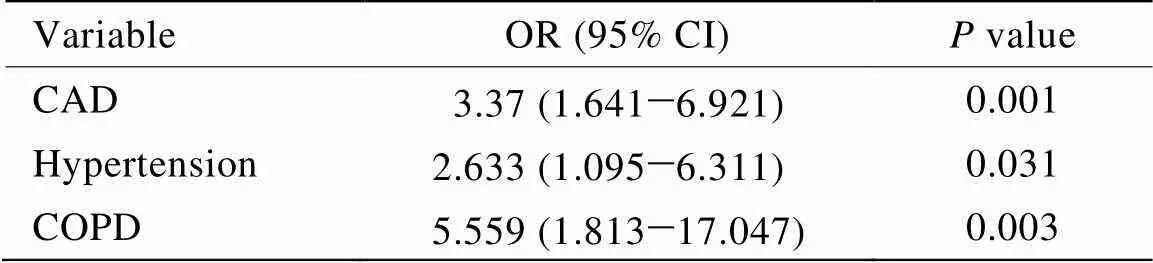
表3 HFpEF的独立危险因素
HFpEF: heart failure with preserved ejection fraction; CAD: coronary artery disease; COPD: chronic obstructive pulmonary disease
3 讨 论
本研究中,HFpEF组患者的年龄偏大(82.01±7.24)岁,舒张功能不全和HFpEF的发生均随增龄而增加。既往研究表明,50~70岁和>70岁患者则分别高达33%和50%左右[13]。在洋地黄研究组试验(the Digitalis Investigation Group trial,DIG)中[14],年龄是HFpEF死亡最重要的预测因素。本研究中,HFpEF组合并高血压、冠心病和糖尿病的比例与既往研究[7]类似,分别为87.6%,69.8%和54.3%。合并用药的差异与合并疾病的差异一致,即HFpEF组高血压、冠心病等疾病比例更高,心功能更差,故服用阿司匹林、硝酸酯类、利尿剂、ACEI/ARB、β阻滞剂、钙通道阻滞剂、醛固酮拮抗剂比例更高。
NT-proBNP与心衰的程度和预后密切相关。本研究中HFpEF组的NT-proBNP水平高于ADD组,符合心衰的进展过程。eGFR的显著差异提示肾功能不全与舒张功能不全及HFpEF有关,在美国医师健康研究(Physicians Health Study,PHS)中[15],早期肾脏疾病与心衰发生率增加相关。HFpEF组的总胆固醇、低密度脂蛋白胆固醇、血红蛋白均低于ADD组(均<0.01),提示血脂代谢异常、贫血等与心衰发生有关。贫血是心衰常见的合并症,CHARM研究的亚组分析中,HFpEF合并贫血的比例为27%[16]。心衰患者通常处于高代谢状态而药物治疗如利尿剂的使用会进一步加重营养不良状态。
在多因素分析中,冠心病和高血压均是HFpEF的独立危险因素,同既往研究[17]及指南[3]一致。由于已有多项研究证明上述结果,在此不做赘述。下面重点讨论COPD与HFpEF。
很多关于HFpEF的研究将COPD作为排除标准[4,18],然而事实上COPD是老年HFpEF患者最常见最重要的合并疾病之一,约1/3的心衰患者合并COPD,并且COPD患者往往合并左室舒张功能不全。本研究中,HFpEF组患者COPD的发生率为29.5%,与既往研究(33.9%)接近[19]。Funk等[20]报道的COPD患者中左室舒张功能不全发生率>50%,Boussuges等[21]报道的发生率为76%,最近1项研究表明[22],COPD患者中轻度左室舒张功能不全发生率更是高达88%,并且独立于COPD严重程度的分级。另一研究[23]发现在门诊的重度COPD患者(FEV130%~50%)中,稳定期重度COPD患者左室舒张功能不全达90%。根据上述研究,COPD对左室舒张功能确实存在影响,与左室舒张功能不全和HFpEF有密切关系,因此,研究包含COPD在内的HFpEF人群有重要意义。
已有研究表明[19],COPD是HFpEF患者全因死亡率的预测因子(OR 1.23,95% CI 1.11~1.37)。因此,既往除外COPD的HFpEF的相关研究不能代表老年群体的实际情况。在本研究中,COPD与HFpEF的风险增加有关,并且是HFpEF的独立危险因素,说明了COPD对HFpEF的重要影响。在分析HFpEF的发展和预后时,应考虑到COPD的因素。反之,对于COPD患者,除了右室功能,也要考虑到左室舒张功能不全的可能性。
COPD与左室舒张功能不全及HFpEF之间的关系尚不十分明确。既往研究多考虑到COPD对右心功能的影响,但事实上,COPD可能对左心功能同样存在影响。可能的病理生理机制主要包括:COPD与HFpEF共同参与炎症反应,炎症反应是COPD发生发展的重要机制,同时也促进粥样硬化斑块的形成,而后者与心肌缺血和左室舒张功能不全密切相关。除了上述机制外,COPD可能导致左室前后负荷的变化:COPD可引起右室压力负荷增加,右室压力增高后能够使室间隔向左室偏移,影响左室结构和降低左室舒张期充盈的顺应性[24,25];肺过度充气(hyperinflation)继发肺气肿,可能影响左室充盈(前负荷)[26];Smith等[27]的研究也证明了COPD和肺气肿患者的肺静脉直径下降,支持上游肺静脉充盈不佳导致左室充盈不良的结论;另有研究表明[28],在轻度气流阻塞(没有肺过度充气)的患者中可以观察到,左房早期折返波能够影响左室后负荷。此外,主动脉舒张压的降低会引起内皮下缺血[29]。这些机制共同作用,影响了心室肌的松弛。
本研究是一项回顾性观察研究,关于HFpEF与COPD内在关系和病理生理机制的相关研究有待大样本量和更加深入的基础研究明确。另外本研究入选患者以男性为主(72.4%),入选者为病例资料齐全的患者,部分房颤患者因未测量e’而未入选,导致本研究中房颤患者比例(3.3%)低于一般老年人群。女性和房颤是HFpEF的重要危险因素,本研究中由于入选女性和房颤比例少而未得到相应结果。总之,本研究的人群中,老年HFpEF的发生率随着增龄而增加,冠心病、高血压和COPD与老年HFpEF患者有关。
[1] Bui AL, Horwich TB, Fonarow GC. Epidemiology and risk profile of heart failure[J]. Nat Rev Cardiol, 2011, 8(1): 30−41.
[2] Owan TE, Hodge DO, Herges RM,. Trends in prevalence and outcome of heart failure with preserved ejection fraction[J]. N Engl J Med, 2006, 355(3): 251−259.
[3] McMurray JJ, Adamopoulos S, Anker SD,. ESC Guidelines for the Diagnosis and Treatment of Acute and Chronic Heart Failure 2012: The Task Force for the Diagnosis and Treatment of Acute and Chronic Heart Failure 2012 of the European Society of Cardiology. Developed in collaboration with the Heart Failure Association (HFA) of the ESC[J]. Eur J Heart Fail, 2012, 14(8): 803−869.
[4] Yancy CW, Lopatin M, Stevenson LW,. Clinical presentation, management, and in-hospital outcomes of patients admitted with acute decompensated heart failure with preserved systolic function: a report from the Acute Decompensated Heart Failure National Registry (ADHERE) Database[J]. J Am Coll Cardiol, 2006, 47(1): 76−84.
[5] Fonarow GC, Stough WG, Abraham WT,. Characteristics, treatments, and outcomes of patients with preserved systolic function hospitalized for heart failure: a report from the OPTIMIZE-HF Registry[J]. J Am Coll Cardiol, 2007, 50(8): 768−777.
[6] Braunstein JB, Anderson GF, Gerstenblith G,. Noncardiac comorbidity increases preventable hospitalizations and mortality among Medicare beneficiaries with chronic heart failure[J]. J Am Coll Cardiol, 2003, 42(7): 1226−1233.
[7] Havranek EP, Masoudi FA, Westfall KA,. Spectrum of heart failure in older patients: results from the National Heart Failure Project[J]. Am Heart J, 2002, 143(3): 412−417.
[8] Aurigemma GP, Gottdiener JS, Shemanski L,. Predictive value of systolic and diastolic function for incident congestive heart failure in the elderly: the cardiovascular health study[J]. J Am Coll Cardiol, 2001, 37(4): 1042−1048.
[9] Sahn DJ, DeMaria A, Kisslo J,. Recommendations regarding quantitation in M-mode echocardiography: results of a survey of echocardiographic measurements[J]. Circulation, 1978, 58(6): 1072−1083.
[10] Devereux RB, Alonso DR, Lutas EM,. Echocardiographic assessment of left ventricular hypertrophy: comparison to necropsy findings[J]. Am J Cardiol, 1986, 57(6): 450−458.
[11] Yancy CW, Jessup M, Bozkurt B,. 2013 ACCF/AHA guideline for the management of heart failure: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines[J]. J Am Coll Cardiol, 2013, 62(16): e147−e239.
[12] Vestbo J, Hurd SS, Agusti AG,. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: GOLD executive summary[J]. Am J Respir Crit Care Med, 2013, 187(4): 347−365.
[13] Zile MR, Brutsaert DL. New concepts in diastolic dysfunction and diastolic heart failure. Part Ⅰ: diagnosis, prognosis, and measurements of diastolic function[J]. Circulation, 2002, 105(11): 1387−1393.
[14] Rich MW, McSherry F, Williford WO,. Effect of age on mortality, hospitalizations and response to digoxin in patients with heart failure: the DIG study[J]. J Am Coll Cardiol, 2001, 38(3): 806−813.
[15] Djousse L, Kurth T, Gaziano JM. Cystatin C and risk of heart failure in the Physicians' Health Study (PHS)[J]. Am Heart J, 2008, 155(1): 82−86.
[16] O’Meara E, Clayton T, McEntegart MB,. Clinical correlates and consequences of anemia in a broad spectrum of patients with heart failure: results of the Candesartan in Heart Failure: Assessment of Reduction in Mortality and Morbidity (CHARM) Program[J]. Circulation, 2006, 113(7): 986−994.
[17] O’Connor CM, Gattis WA, Shaw L,. Clinical characteristics and long-term outcomes of patients with heart failure and preserved systolic function[J]. Am J Cardiol, 2000, 86(8): 863−867.
[18] Komajda M, Carson PE, Hetzel S,. Factors associated with outcome in heart failure with preserved ejection fraction: findings from the Irbesartan in Heart Failure with Preserved Ejection Fraction Study (I-PRESERVE)[J]. Circ Heart Fail, 2011, 4(1): 27−35.
[19] Ather S, Chan W, Bozkurt B,. Impact of noncardiac comorbidities on morbidity and mortality in a predominantly male population with heart failure and preservedreduced ejection fraction[J]. J Am Coll Cardiol, 2012, 59(11): 998−1005.
[20] Funk GC, Lang I, Schenk P,. Left ventricular diastolic dysfunction in patients with COPD in the presence and absence of elevated pulmonary arterial pressure[J]. Chest, 2008, 133(6): 1354−1359.
[21] Boussuges A, Pinet C, Molenat F,. Left atrial and ventricular filling in chronic obstructive pulmonary disease. An echocardiographic and Doppler study[J]. Am J Respir Crit Care Med, 2000, 162(2 Pt 1): 670−675.
[22] Caram LM, Ferrari R, Naves CR,. Association between left ventricular diastolic dysfunction and severity of chronic obstructive pulmonary disease[J]. Clinics(Sao Paulo), 2013, 68(6): 772−776.
[23] Lopez-Sanchez M, Munoz-Esquerre M, Huertas D,. High prevalence of left ventricle diastolic dysfunction in severe COPD associated with a low exercise capacity: a cross-sectional study[J]. PLoS One, 2013, 8(6): e68034.
[24] Minai OA, Chaouat A, Adnot S. Pulmonary hypertension in COPD: epidemiology, significance, and management: pulmonary vascular disease: the global perspective[J]. Chest, 2010, 137(6 Suppl): 39S−51S.
[25] Kohama A, Tanouchi J, Hori M,. Pathologic involvement of the left ventricle in chronic cor pulmonale[J]. Chest, 1990, 98(4): 794−800.
[26] Watz H, Waschki B, Meyer T,. Decreasing cardiac chamber sizes and associated heart dysfunction in COPD: role of hyperinflation[J]. Chest, 2010, 138(1): 32−38.
[27] Smith BM, Prince MR, Hoffman EA,. Impaired left ventricular filling in COPD and emphysema: is it the heart or the lungs? The Multi-Ethnic Study of Atherosclerosis COPD Study[J]. Chest, 2013, 144(4): 1143−1151.
[28] Barr RG, Bluemke DA, Ahmed FS,. Percent emphysema, airflow obstruction, and impaired left ventricular filling[J]. N Engl J Med, 2010, 362(3): 217−227.
[29] Laurent S, Cockcroft J, Van Bortel L,. Expert consensus document on arterial stiffness: methodological issues and clinical applications[J]. Eur Heart J, 2006, 27(21): 2588−2605.
(编辑: 周宇红)
Risk factors for heart failure with preserved ejection fraction in the elderly
HUANG Ying-Shuo1, ZHANG Jian1, WANG Dan2, BAI Li1, YANG Xu1, HUANG Wei1, LI Min1, SUN Ying1*
(1Department of Geriatric Cardiology,2Department of Blood Transfusion, Beijing Friendship Hospital, Capital Medical University, Beijing 100050, China)
To determine the risk factors for heart failure with preserved ejection fraction (HFpEF) in the elderly by retrospectively analyzing their clinical features and echocardiographic parameters of HFpEF patients and comparing with those of non-heart failure patients with asymptomatic diastolic dysfunction.A total of 234 consecutive patients (≥60 years old) admitted in our department from December 2011 to December 2012 were enrolled in this study. They were divided into asymptomatic left ventricular diastolic dysfunction group (ADD group,=104) and HFpEF group (=130). Risk factors of HFpEF were analyzed by logistic regression.Compared with ADD group, the patients in HFpEF group were older and had a lower estimated glomerular filtration rate (eGFR) (<0.05). Logistic regression analysis indicated that coronary artery disease(CAD), hypertension, and chronic obstructive pulmonary disease (COPD) were independent risk factors of HFpEF (=0.001, 0.031, 0.003, respectively).CAD, hypertension and COPD are associated with HFpEF in this cohort.
elderly; heart failure with preserved ejection fraction; diastolic dysfunction
(13JL48)(2011D003034000026).
R541.6; R592
A
10.3724/SP.J.1264.2014.000156
2014−06−03;
2014−08−21
首都医科大学基础-临床合作基金(13JL48);北京市优秀人才培养基金(2011D003034000026)
孙 颖, E-mail: ysun15@163.com
