缺血后适应对老龄大鼠心肌缺血再灌注损伤的保护作用
2014-04-23张存泰李彩萍全小庆
杨 艺,张存泰,李彩萍,全小庆,阮 磊
缺血后适应对老龄大鼠心肌缺血再灌注损伤的保护作用
杨 艺,张存泰,李彩萍*,全小庆,阮 磊
(华中科技大学同济医学院附属同济医院综合科,武汉 430030)
研究缺血后适应能否减轻老龄大鼠急性心肌缺血再灌注损伤,比较缺血后适应的心脏保护作用在成年和老龄大鼠之间有无差别。32只雄性F344大鼠分为成年(6~8月龄)和老龄(20~22月龄)组,每组再分为缺血再灌注(I/R)组(缺血30min,再灌注2h,8只)和缺血后适应(IPost)组(缺血30min,给予4轮10s再通/10s缺血后再灌注2h,8只),监测平均动脉压(MAP)、心率收缩压乘积(RPP)等血流动力学参数和心电图,测定心肌梗死面积,再灌注2h后检测血清肌酸激酶(CK)和乳酸脱氢酶(LDH)浓度。再灌注2h时,成年IPost组MAP和RPP均高于I/R组(<0.05),而老龄IPost组与I/R组间差异无统计学意义(>0.05)。再灌注初30min内,成年IPost组和I/R组心律失常评分分别为1分和3.5分,两者间差异有统计学意义(<0.05);老龄IPost组和I/R组心律失常评分分别为2分和3分,两者间差异无统计学意义(>0.05)。成年和老龄IPost组心肌梗死面积较I/R组分别减少52%和44%(均<0.05)。成年和老龄IPost组CK和LDH浓度较I/R组均有明显降低(<0.05)。缺血后适应能缩小老龄大鼠心肌梗死面积、减少心肌酶释放,且其程度与成年大鼠相似;同时缺血后适应能改善成年大鼠心肌顿抑、减少再灌注心律失常,但此作用在老龄大鼠未观察到。
大鼠;再灌注损伤;缺血后适应;心肌保护
2003年Zhao等[1]发现在长时间缺血后、恢复再灌注前进行数次短暂重复的心肌缺血再灌注能保护心肌对抗随后的再灌注损伤,进而提出了缺血后适应(ischemic post-conditioning,IPost)这一概念。多种动物模型已经证明其在减少梗死面积和保护内皮细胞功能等方面与缺血预适应(ischemic pre-conditioning,IP)有相同的功效,但它有更强的临床可操作性,成为近来急性心肌梗死(acute myocardial infarction,AMI)治疗的研究热点。然而,目前关于IPost对衰老心脏是否具有保护作用国内外相关报道较少,本课题以20~22月龄的F344老龄大鼠建立在体心脏急性缺血再灌注(ischemia/reperfusion,I/R)损伤模型,观察IPost对老龄大鼠心脏再灌注损伤有无保护作用,为IPost在老年AMI患者冠状动脉介入治疗中的应用提供动物实验依据。
1 材料与方法
1.1 材料
1.1.1 实验动物 成年雄性F344大鼠(6~8月龄),体质量190~220g;老龄雄性F344大鼠(18~20月龄),体质量310~340g,华中科技大学同济医学院实验动物中心。本实验遵循《实验动物保护条例》。
1.1.2 主要仪器及试剂 HX-300小型动物呼吸机,成都泰盟,GY-6328生理参数分析记录仪,华南医电,血管扩张球囊(¢2.5-L14),伊文思蓝和氯化三苯基四氮唑(triphenyltetrazolium chloride,TTC)Sigma,肌酸激酶(creatine kinase,CK)和乳酸脱氢酶(lactate dehydrogenase,LDH)试剂盒,南京凯基。
1.2 动物建模及分组
1.2.1 建立模型 大鼠以3%戊巴比妥钠(50mg/kg)腹腔麻醉后固定,行右侧股动脉插管,监测心率(heart rate,HR)、收缩压(systolic blood pressure,SBP)、舒张压(diastolic blood pressure,DBP)和平均动脉压(mean arterial pressure,MAP),皮下埋入针形电极记录心电图。行气管插管,连接小动物呼吸机,调节潮气量2~3ml/100g,呼吸频率50~60次/min,呼吸比2∶1。经左侧第四肋间开胸暴露心脏,于左心耳下方2mm进针,以6-0线在左冠状动脉前降支后方穿过,将充水球囊垫于血管与结扎线之间,拉紧缝线后可见心电图ST段明显抬高,松开后ST段下降>1/2,表明结扎位置正确。缺血30min后,抽空球囊,再灌注2h。
1.2.2 分组 32只大鼠分为4组,每组8只:(1)老龄缺血再灌注组(I/R aged)及成年缺血再灌注组(I/R adult):大鼠造模,结扎冠状动脉左前降支缺血30min后,直接恢复再灌注2h;(2)老龄缺血后适应组(IPost aged)及成年缺血后适应组(IPost adult):大鼠造模,结扎冠状动脉左前降支缺血30min后,于再灌注即刻给予4轮10s再灌注/10s缺血(4×10)的IPost,再持续灌注2h。
1.3 观察指标
1.3.1 记录缺血和再灌注 记录缺血1min、30min和再灌注1h、2h大鼠的HR、SBP、DBP和MAP,以相应的心率收缩压乘积(rate pressure product,RPP)作为心肌耗氧量指标。
1.3.2 采用评分系统对再灌注初30min内心律失常的严重程度进行定量分析[2]无心律失常为0分;偶发室性期前收缩(premature ventricular beats,PVB)为1分;PVB二联律或PVB连发为2分;1~2次室性心动过速(ventricular tachycardia,VT)为3分;≥3次VT或一过性心室颤动(ventricular fibrillation,VF)为4分;频发或持续性VF甚至导致动物死亡为5分。每个心脏以其出现的最严重的心律失常所对应的分数作为其评分。
1.3.3 再灌注后处理 再灌注2h后,原位结扎冠状动脉左前降支,推注伊文思蓝,染色5min后处死动物,立即取心脏,剪除心房、大血管、右心室,将左心室冻存于-80℃冷冻20min。从心尖至心底垂直长轴水平切片,每片厚2~3mm。将切片浸泡于1%TTC溶液中,37℃避光水浴30min后置于10%甲醛溶液过夜。经伊文思蓝和TTC双染色后[3],正常非缺血心肌为蓝色,缺血未梗死心肌为砖红色,梗死心肌为白色。采用Image-Pro Plus 6.0图像分析软件分析各区域面积。缺血危险区面积(area at risk,AAR)(%)=(红色+白色区域面积)/(蓝色+红色+白色区域面积)×100%;心肌梗死面积(infarct size,IS)(%)=(白色区域面积)/(红色+白色区域面积)×100%。
1.3.4 再灌注2h后采动脉血 采动脉血1ml,3000r/min离心15min后收集血清,冻存于-80℃,使用商业试剂盒按说明书步骤检测血清CK和LDH浓度。
1.4 统计学处理
采用SPSS16.0统计软件,符合正态分布数据以均数±标准差表示,组间比较采用方差分析;不符合正态分布数据以中位数(四分位间距)表示,组间比较采用Kruskal-Wallis检验和Fisher精确检验。<0.05为差异有统计学意义。
2 结 果
2.1 一般情况
老龄组大鼠体质量明显高于成年组大鼠[(327±11)(208±10)g,<0.05],老龄组大鼠心脏质量也是成年组大鼠的1.5倍[(1.14±0.04)(0.77±0.03)g,<0.05],但是心重指数(=心脏质量/体质量×100%)老龄大鼠显著低于成年大鼠[(0.35±0.004)%(0.37±0.004)%,<0.05]。
2.2 血流动力学变化
结扎前4组大鼠间HR、MAP和RPP差异无统计学意义。缺血1min时4组大鼠HR均明显加快,MAP均明显降低(<0.05),除I/R aged组外余3组RPP明显降低。在缺血30min时,各组HR、MAP、RPP又回到基线水平。在再灌注过程中,4组大鼠HR有下降趋势,但各组间无差异,与结扎前也无差异;而MAP和RPP与结扎前相比均明显下降。再灌注2h结束时,IPost adult组的MAP和RPP均高于I/R adult组(<0.05),而IPost aged组与I/R aged组间差异无统计学意义。在缺血30min及再灌注1,2h时,IPost aged组的MAP都低于IPost adult组(<0.05;表1)。
2.3 再灌注心律失常发生情况
再灌注初30min内,I/R aged组和I/R adult组分别有7例(87.5%)和6例(75.0%)发生了VT或VF,心律失常评分分别为3.0(1.75)和3.5(1.75)。IPost aged组和IPost adult组分别发生了3例(37.5%)和1例(12.5%)VT或VF,心律失常评分为2.0(2.0)和1.0(1.5)。可以看出,IPost组VT、VF的发生例数和心律失常评分均较I/R组降低,但仅成年组大鼠两者间差异有统计学意义(<0.05)。成年组大鼠和老龄组大鼠间差异无统计学意义(>0.05;表2)。
2.4 缺血危险区面积及梗死面积
AAR在4组大鼠之间是可比的[I/R adult(54.7±5.6)%;IPost adult(52.5±7.3)%;I/R aged(53.2±5.1)%;IPost aged(55.7±3.7)%;所有>0.05]。IPost adult组的IS较I/R adult组减少52%[分别为(15.2±1.8)%和(31.8±2.7)%,<0.05],IPost aged组IS较I/R aged组减少44%[分别为(16.1±2.6)%和(28.6±3.4)%,<0.05]。成年大鼠和老龄大鼠间IS差异无统计学意义(>0.05;图1)。
2.5 心肌酶学
再灌注2h结束时,IPost组CK和LDH浓度较I/R组明显降低(均<0.05),但I/R adult组和I/R aged组之间、IPost adult组和IPost aged组之间差异无统计学意义(>0.05;图2)。

表1 缺血/再灌注过程中血流动力学变化
HR: heart rate; MAP: mean arterial pressure; RPP: rate pressure product. 1mmHg=0.133kPa. Compared with baseline,*<0.05; compared with I/R adult group,#<0.05; compared with IPost adult group,△<0.05
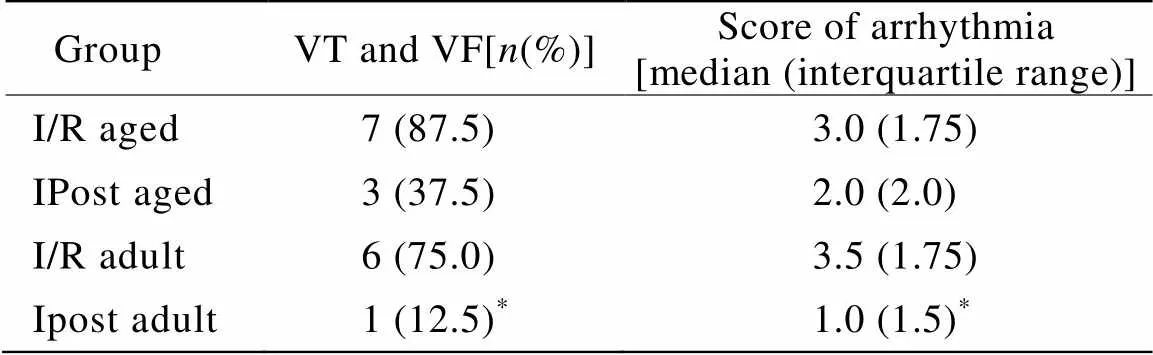
表2 4组大鼠心律失常发生例数和评分
VT: ventricular tachycardia; VF: ventricular fibrillation. Compared with I/R adult group,*<0.05
3 讨 论
2003年,Zhao等[1]首次在犬心肌I/R模型上提出IPost的概念,后被应用到其他物种[4],继而推广到临床研究[5]中以期减少AMI患者的IS。相对预适应,IPost有更好的临床可操作性,因此研究其对衰老心脏是否具有保护作用有重要的临床价值。
IPost减少IS的程度与血管再闭塞的次数和持续时间密切相关。李敏等[6]对成年大鼠(8~10月龄)行3轮5s I/5s R(3×5)、3轮10s I/10s R(3×10)或3轮30s I/30s R(3×30)IPost均能减少IS;对老龄大鼠(22~24月龄)3×10和3×30的方法有保护作用,而3×5的方法却没有,提示对衰老心脏刺激强度的重要性。本实验选择的是4轮10s I/10s R(4×10)的IPost方式,结果显示该方式能明显减少成年及老龄大鼠在体心脏IS(52%和44%),与国内外相关报道一致[7]。
除IS外,本研究同时选择IPost临床研究常用的终点指标心肌酶CK和LDH间接反映IS的大小[8]。与IS染色结果一致,本研究发现IPost较I/R能明显降低血清CK和LDH释放水平,此效果在成年大鼠和老龄大鼠中均存在,提示CK和LDH可作为评估IPost对衰老心脏保护作用的良好间接指标。IPost的心肌保护作用可能由ROS、NO、Ca2+、腺苷、缓激肽、ANP/BNP等介导[9],其具体机制尚有待进一步研究。
I/R导致的心肌可逆性或不可逆性损伤均造成心肌舒缩功能降低,其中可逆性的心功能降低称为心肌顿抑(myocardial stunning)。本实验通过观察再灌注过程中HR、MAP、RPP等血流动力学参数的变化间接反映心功能的改变。恢复再灌注2h后,IPost组MAP和RPP水平较I/R组有所升高,但仅在成年组大鼠两者间有统计学差异,对老龄组大鼠无明显作用。提示IPost抗梗死和抗顿抑效果在不同年龄组不尽一致。尽管IPost对改善老龄大鼠心肌顿抑没有明确效果,但IPost减少IS仍可能间接改善左室功能。大鼠心脏离体实验表明IPost对心功能恢复的作用与其减少IS的能力是平行的[10]。临床实验中也观察到,能减少IS的IPost干预对左室功能改善能获得短期及长期的益处[11]。
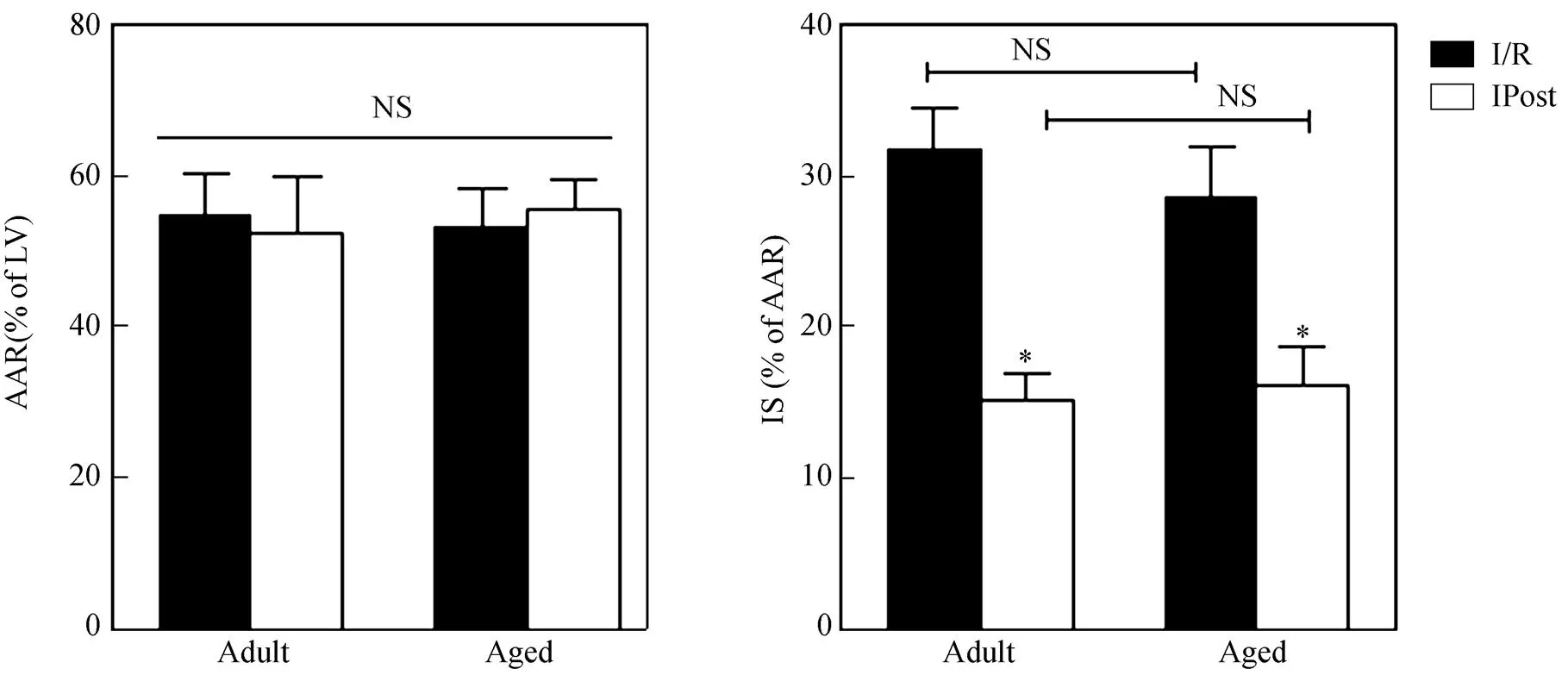
图1 成年及老龄大鼠缺血危险面积和梗死面积
Figure 1 AAR and IS in adult and aged rats
NS: not statistically significant; AAR: area at risk; LV: left ventricle; IS: infarct size. Compared with I/R group,*<0.05
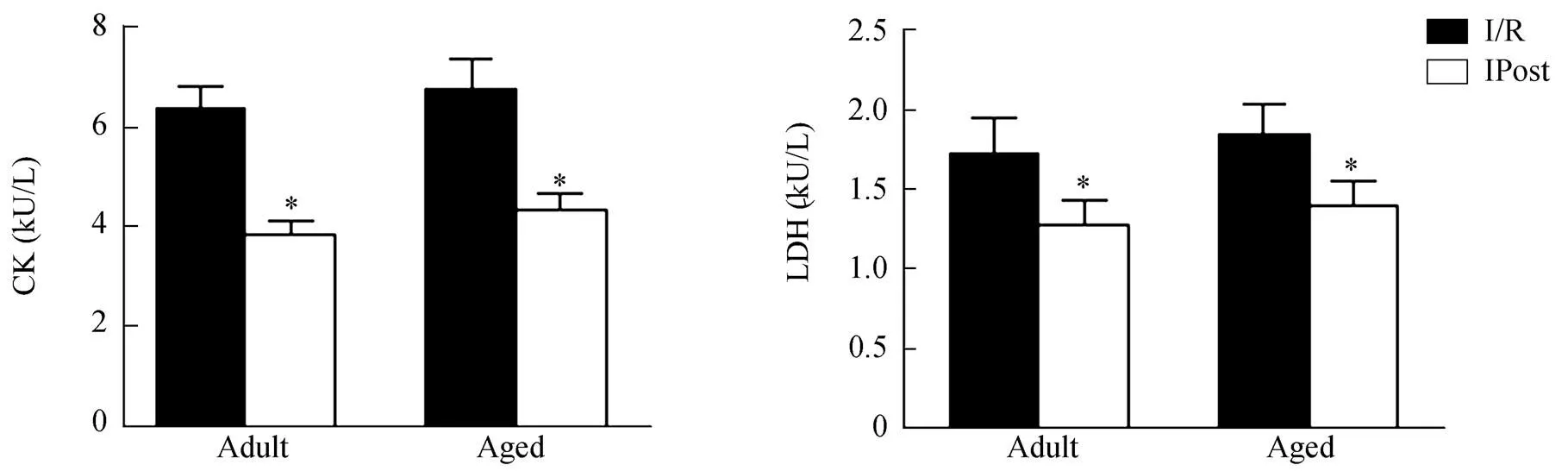
图2 再灌注2h时成年组和老龄组大鼠血清CK和LDH浓度
Figure 2 Serum levels of CK and LDH in adult and aged rats at 2 hours post reperfusion
CK: creatine kinase; LDH: lactate dehydrogenase. Compared with I/R group,*<0.05
目前已有研究报道IPost抗再灌注心律失常作用。Galagudza等[12]将离体大鼠心脏缺血30min后,于再灌注15min后行单次全心缺血2min的IPost可使持续性VF转复为窦律。Kloner等[13]采用在体大鼠模型,在缺血5min后行更经典的IPost方法(4轮20s I/20s R),发现IPost能够降低室性心律失常的发生率,并且VT的平均持续时间也明显减少。本研究采用全程心电监护,通过心律失常评分系统对心律失常发生的严重程度进行定量分析,发现IPost可使成年大鼠再灌注30min内VT、VF的发生率和心律失常评分降低,但老龄大鼠未获得相似的效果,推测可能与老龄大鼠心肌老化、本身心律失常发生率升高[14]有关;也可能本研究样本数量偏少,未能发生差异。既往研究[15,16]提示IPost抗心律失常作用不依赖于抗心肌细胞凋亡作用,具体机制尚有待进一步研究。
[1] Zhao ZQ, Corvera JS, Halkos ME,. Inhibition of myocardial injury by ischemic postconditioning during reperfusion: comparison with ischemic preconditioning[J]. Am J Physiol Heart Circ Physiol, 2003, 285(2): H579−H588.
[2] Xiong J, Wang Q, Xue FS,. Comparison of cardioprotective and anti-inflammatory effects of ischemia pre- and postconditioning in rats with myocardial ischemia-reperfusion injury[J]. Inflamm Res, 2011, 60(6): 547−554.
[3] Schwarz ER, Somoano Y, Hale SL,. What is the required reperfusion period for assessment of myocardial infarct size using triphenyltetrazolium chloride staining in the rat[J]? J Thromb Thrombolysis, 2000, 10(2): 181−187.
[4] Yang XM, Liu Y, Liu Y,. Attenuation of infarction in cynomolgus monkeys: preconditioning and postconditioning[J]. Basic Res Cardiol, 2010, 105(1): 119−128.
[5] Hahn JY, Song YB, Kim EK,. Ischemic postconditioning during primary percutaneous coronary intervention: the effects of postconditioning on myocardial reperfusion in Patients with ST-segment Elevation Myocardial Infarction (POST) randomized trial[J]. Circulation, 2013, 128(17): 1889−1896.
[6] Li M, Zhang J, Liang YH,. Effects of ischemic postconditioning on myocardial infarction sizes and protein kinase C expression in aged rats with post-ischemia reperfusion injury[J]. Chin J Geriatr, 2010, 29(5): 420−423. [李 敏, 张 健, 梁艳红, 等. 缺血后处理对心肌缺血再灌注大鼠心肌梗死面积和细胞蛋白激酶Cα表达的影响[J]. 中华老年医学杂志, 2010, 29(5): 420−423.]
[7] Yin Z, Gao H, Wang H,. Ischaemic post-conditioning protects both adult and aged Sprague-Dawley rat heart from ischaemia-reperfusion injury through the phosphatidylinositol 3-kinase-AKT and glycogen synthase kinase-3beta pathways[J]. Clin Exp Pharmacol Physiol, 2009, 36(8): 756−763.
[8] Staat P, Rioufol G, Piot C,. Postconditioning the human heart[J]. Circulation, 2005, 112(14): 2143−2148.
[9] Ovize M, Baxter GF, Di Lisa F,. Postconditioning and protection from reperfusion injury: where do we stand? Position paper from the Working Group of Cellular Biology of the Heart of the European Society of Cardiology[J]. Cardiovasc Res, 2010, 87(3): 406−423.
[10] Tawa M, Fukumoto T, Yamashita N,. Postconditioning improves postischemic cardiac dysfunction independently of norepinephrine overflow after reperfusion in rat hearts: comparison with preconditioning[J]. J Cardiovasc Pharmacol, 2010, 55(1): 6−13.
[11] Wang G, Zhang S, Joggerst SJ,. Effects of the number and interval of balloon inflations during primary PCI on the extent of myocardial injury in patients with STEMI: does postconditioning exist in real-world practice[J]? J Invasive Cardiol, 2009, 21(9): 451−455.
[12] Galagudza M, Kurapeev D, Minasian S,. Ischemic postconditioning: brief ischemia during reperfusion converts persistent ventricular fibrillation into regular rhythm[J]. Eur J Cardiothorac Surg, 2004, 25(6): 1006−1010.
[13] Kloner RA, Dow J, Bhandari A. Postconditioning markedly attenuates ventricular arrhythmias after ischemia- reperfusion[J]. J Cardiovasc Pharmacol Ther, 2006, 11(1): 55−63.
[14] Wang XF, Zhang CT, Xu RD,. Effect of aging-related changes in gap junction protein on arrhythmia in rats[J]. Chin J Geriatr, 2011, 30(5): 427−430. [王杏芬, 张存泰, 徐仁德, 等. 大鼠心室肌缝隙连接蛋白增龄性变化对心律失常发生率的影响[J]. 中华老年医学杂志, 2011, 30(5): 427−430.]
[15] Dow J, Bhandari A, Kloner RA. The mechanism by which ischemic postconditioning reduces reperfusion arrhythmias in rats remains elusive[J]. J Cardiovasc Pharmacol Ther, 2009, 14(2): 99−103.
[16] Kolettis TM, Vilaeti AD, Tsalikakis DG,Effects of pre- and postconditioning on arrhythmogenesis in therat model[J]. J Cardiovasc Pharmacol Ther, 2013, 18(4): 376−385.
(编辑: 李菁竹)
Ischemic post-conditioning protects aged rat hearts against ischemia/reperfusion injury
YANG Yi, ZHANG Cun-Tai, LI Cai-Ping*, QUAN Xiao-Qing, RUAN Lei
(Department of Geriatrics, Tongji Hospital, Tongji Medical College, Huazhong University of Science and Technology, Wuhan 430030, China)
To investigate whether ischemic post-conditioning (IPost) can ameliorate acute myocardial ischemia/reperfusion (I/R) injury in senescent rats and to compare the cardioprotective effects of ischemic post-conditioning between aged and adult rats.A total of 32 male F344 rats were divided into adult (6 to 8 months) group and aged (18 to 20 months) group. After the rats were subjected to 30min ischemia by ligating the left anterior descending coronary artery (LAD), their hearts from each group were further randomized to receive standard, abrupt reperfusion (I/R group), or were post-conditioned with 4 cycles of 10s ischemia interspersed by 10s reperfusion immediately at the end of the ischemia (IPost group). Hemodynamic changes, such as mean arterial pressure (MAP) and rate-pressure product (RPP), and electrocardiogram (ECG) were recorded. Infarct size was measured by Evans blue and triphenyltetrazolium chloride (TTC) staining. At 120min of reperfusion, serum levels of creatine kinase (CK) and lactate dehydrogenase (LDH) were assayed.After 2 hours reperfusion, MAP and RPP were significantly higher in IPost group than in the corresponding I/R group for adult rats (<0.05). However, no significance was achieved in aged rats (>0.05). During the first 30min reperfusion, in adult rats, the arrhythmia scores were 1.0 and 3.5 respectively for the IPost group and I/R group with significant difference (<0.05). However, in aged rats, the arrhythmia scores were 2.0 and 3.0 for the IPost group and I/R group, but without significant difference (>0.05). Post obviously decreased the infarct size in the IPost group than in corresponding I/R group in both adult (by 52%) and aged cohorts (by 44%;<0.05 for both). The serum levels of CK and LDH were markedly lower in IPost group than in I/R group from both adult and aged rats (<0.05 for both).IPost, as same powerful as to adult rats, reduces infarct size and decreases the release of myocardial enzymes in aged rats. What’s more, the post-conditioning attenuates myocardial stunning and reperfusion arrhythmia in adult rats, but these effects are not seen in the aged rats.
rats; reperfusion injury; ischemic post-conditioning; cardioprotection
(81300141).
R543
A
10.3724/SP.J.1264.2014.000141
2014−05−08;
2014−06−02
国家自然科学基金青年基金(81300141)
李彩萍, E-mail: yangyigracy@gmail.com