冠心病合并颈动脉狭窄患者冠状动脉旁路移植术后远期结果
2014-04-23高长青任崇雷肖苍松
刘 帅,高长青,任崇雷,肖苍松,王 嵘,吴 扬
冠心病合并颈动脉狭窄患者冠状动脉旁路移植术后远期结果
刘 帅,高长青*,任崇雷,肖苍松,王 嵘,吴 扬
(解放军总医院心血管外科,北京 100853)
分析不同术式(心脏停跳或不停跳)对行冠状动脉旁路移植术(CABG)后患者脑卒中发生率和生存率的影响。解放军总医院心血管外科2003年6月至2013年6月冠心病合并颈动脉狭窄的159例患者,其中男118例,女41例,年龄为(67.0±7.5)岁,根据心脏是否停跳分为停跳(on-pump)组及不停跳(off-pump)组,并对两组患者行CABG后的脑卒中发生率和生存率进行回顾性分析。随访146例,随访率93.6%,随访时间6~120(46.3±25.3)个月,10例术后出现神经系统症状,其中2例脑出血,8例脑梗死。17例死亡(4例脑部并发症,1例食管癌,1例肺癌,11例为心源性),平均死亡时间为术后41(4~72)个月。停跳组患者术后脑卒中发生率及生存率与不停跳组相比差异无统计学意义(>0.05)。心脏是否停跳对冠心病合并颈动脉狭窄患者术后脑卒中发生率和生存率无明显影响。
冠状动脉分流术;冠状动脉疾病;颈动脉狭窄;卒中;停跳;不停跳
脑卒中是冠状动脉旁路移植术(coronary artery bypass grafting,CABG)后的严重并发症之一,具有较高的致死率与致残率,严重影响了患者的预后及生活质量[1]。对于采用CABG治疗冠心病的方法,目前存在3种意见:一种认为心脏不停跳(off-pump)对冠心病患者更有益,具有更低的术后脑卒中发生率和死亡率[2−4];一种认为心脏停跳(on-pump)更有益[5,6];还有一些研究认为两种术式的结果是一样的[7−9]。所以究竟哪种方法更优目前尚无定论,尤其是对于合并颈动脉狭窄的冠心病患者应该采取哪种手术方式的相关研究就更为罕见[10]。本文针对解放军总医院心血管外科冠心病合并颈动脉狭窄的患者进行统计和随访,并分析了不同术式对行CABG后患者脑卒中的发生率及生存率的影响。
1 对象与方法
1.1 研究对象
2003年6月至2013年6月解放军总医院心血管外科共有159例冠心病合并颈动脉狭窄的患者行CABG,约占同期CABG总数的6.54%,其中男118例,女41例;年龄51~83岁(67.0±7.5)岁。患者均有不稳定型心绞痛史,合并高血压病100例(62.9%),2型糖尿病55例(34.6%),血脂异常27例(17.0%),有脑卒中病史42例(26.4%)。患者均行冠状动脉造影,提示:单支病变4例,双支病变16例,三支病变89例,左主干病变60例,合并室壁瘤3例、二尖瓣疾病4例、主动脉瓣疾病3例、心包炎1例。心功能NYHA Ⅱ−Ⅳ级。所有患者术前常规行颈动脉超声检查,根据美国超声放射学会推荐的颈动脉狭窄判断标准:轻度狭窄(单侧或双侧<50%)12例(7.5%),中度狭窄(50%≤单侧或双侧<70%)89例(56.0%),重度狭窄(70%≤单侧或双侧<99%)55例(34.6%),完全闭塞3例(1.9%)。95例是在心脏停跳下完成的,64例是非停跳下完成的,两组的基本资料详见表1。
1.2 手术方法
159例均单纯行CABG,未进行颈动脉干预,其中95例采用心脏停跳术式,64例采用心脏不停跳术式,内包括2例行机器人不开胸全内镜(非体外循环)冠状动脉旁路移植术(totally endoscopic coronary artery bypass graft,TECABG),5例行机器人乳内动脉(internal mammary arteries)游离、小切口直接(心脏跳动下)冠状动脉旁路移植术(minimally invasive direct coronary artery bypass graft,MIDCABG),机器人手术均为全麻下右侧单肺通气后于左侧胸腔入路,TECABG为全内镜下行CABG,MIDCABG在左第四肋间前外侧小切口(约6cm)进胸,直视下行CABG。其余均为胸骨正中切口,常规游离左胸廓乳内动脉,off-pump CABG借助于冠状动脉内分流器和心脏固定器,on-pump CABG借助于体外循环机及阻断钳完成手术。关胸前常规行“血管桥”血流量测定。在完成远端吻合后,经右心房、房间隔暴露并处理二尖瓣或切开主动脉处理主动脉瓣;合并室壁瘤者,切除瘤体后,采用“三明治”法或左心室内补片法修补。

表1 冠心病合并颈动脉狭窄患者基本资料
BMI: body mass index; CAD: coronary artery disease; COPD: chronic obstructive pulmonary disease; PCI: percutaneous coronary intervention; IMA: internal maxillary artery; LAD: left anterior descending coronary artery; MBP: mean blood pressure. 1mmHg=0.133kPa
1.3 随 访
出院后采取住院、门诊或电话随访,随访时间6~120个月,观察指标主要包括:死亡、心肌梗死、脑卒中。
1.4 统计学处理
采用SPSS13.0统计学软件进行分析,绘制脑卒中及死亡率与随访时间的关系趋势图。<0.05为差异有统计学意义。
2 结 果
2.1 手术结果
64例行off-pump CABG,95例行on-pump CABG,其中3例同期行室壁瘤切除术、2例行二尖瓣置换术、2例行二尖瓣成形术、3例行主动脉瓣置换术、1例行心包剥脱术。停跳组平均冠状动脉搭桥(2.9±0.7)支,术中平均动脉压(60.4±6.9)mmHg(1mmHg=0.133kPa);不停跳组平均冠状动脉搭桥(2.4±0.6)支,术中平均动脉压(70.6±6.9)mmHg。住院期间术后两组共出现脑梗死2例,死亡3例(1例肺部感染,1例脑出血,1例桥血管出血)。余156例康复出院。
2.2 随 访
146例(93.6%)患者得到随访,随访期间8例出现脑梗死,2例出现脑出血,共有17例患者死亡(4例脑卒中,1例食管癌,1例肺癌,余均为心源性)。
2.3 不同术式的患者术后再发脑卒中风险及生存率的关系
停跳组患者术后脑卒中发生率及生存率与不停跳组相比差异无统计学意义(=0.388,=0.765),详见图1,图2。
3 讨 论
我科资料显示心脏是否停跳对冠心病合并颈动脉狭窄患者术后脑卒中发生率和生存率无明显影响。(1)目前认为,CABG术后脑卒中的独立危险因素包括高龄、不稳定型心绞痛、周围血管病、慢性阻塞性肺疾病、再次手术、糖尿病、颈动脉病变等[11,12]。本研究中两组患者的上述情况均无明显差异。(2)有研究表明,术前脑梗死也是术后发生脑卒中的危险因素之一,其术后苏醒时间、ICU及住院时间均延长;术后谵妄、脑卒中及二次插管的发生率较术前无脑梗死的患者高[13]。但本研究中停跳组术前合并脑梗死有26例(27.3%),不停跳组有16例(25.0%),值为0.740,差异无统计学意义。(3)CABG术中平均血压的高低对于术后脑卒中的发生是有一定影响的,尤其是对合并颈动脉狭窄的冠心病患者。本研究中停跳组术中最低平均血压(60.4±6.9)mmHg,不停跳组血压最低时为近端吻合侧壁钳钳夹主动脉,当时平均血压是(70.6±6.9)mmHg,值为0.592,两组的平均血压均>60mmHg,且差异无统计学意义。
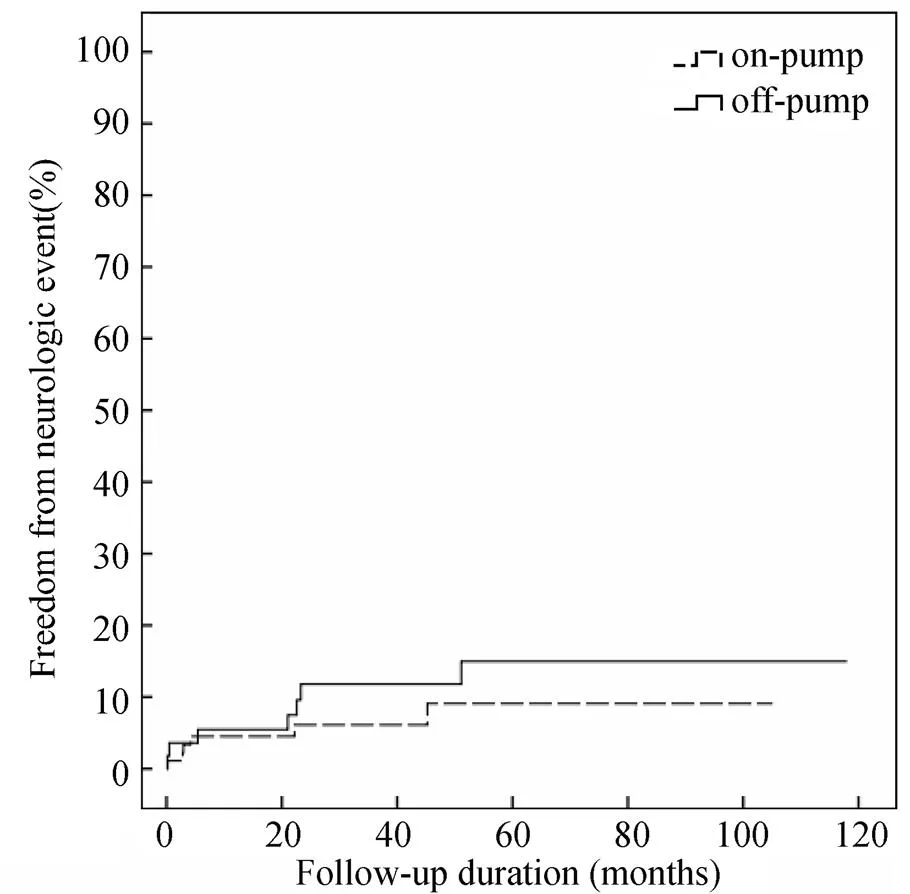
图1 停跳组与不停跳组患者术后脑卒中发生率与随访时间的关系
Figure 1 Relationship postoperative cerebral complications with follow-up duration between on-pump and off-pump procedures
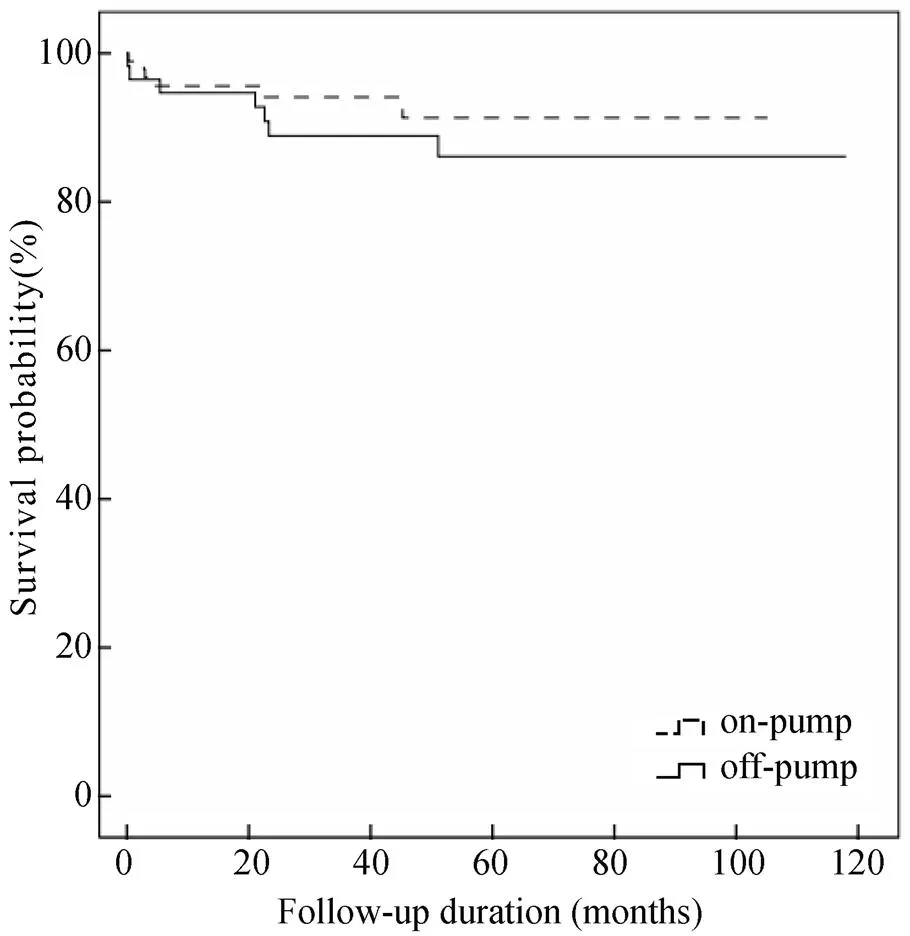
图2 停跳组与不停跳组患者生存率与随访时间的关系
Figure 2 Relationship of postoperative mortality with follow-up duration between on-pump and off-pump procedures
虽然本组研究中停跳组患者术后脑卒中发生率及生存率与不停跳组相比差异无统计学意义,但由图1和图2可得知,停跳组术后脑中风发生率和死亡率整体趋势均低于不停跳组,因本组例数较少,并且为回顾性研究,结果仅供参考和讨论,至于哪种术式更适合于冠心病合并颈动脉狭窄的患者,仍需大样本多中心的前瞻性研究。
[1] Li GW, Zheng GY, Li JG,. Relationship between carotid atherosclerosis and cerebral infarction[J]. Chin Med Sci J, 2010, 25(1): 32−37.
[2] Fareed KR, Rothwell PM, Mehta Z,. Synchronous carotid endarterectomy and off-pump coronary bypass: an updated, systematic review of early outcomes[J]. Eur J Vasc Endovasc Surg, 2009, 37(4): 375−378.
[3] Filardo G, Grayburn PA, Hamilton C,. Comparing long-term survival between patients undergoing off-pump and on-pump coronary artery bypass graft operations[J]. Ann Thorac Surg, 2011, 92(2): 571−577.
[4] Angelini GD, Culliford L, Smith DK,. Effects of on- and off-pump coronary artery surgery on graft patency, survival, and health-related quality of life: long-term follow-up of 2 randomized controlled trials[J]. J Thorac Cardiovasc Surg, 2009, 137(2): 295−303.
[5] Shroyer AL, Grover FL, Hattler B,. On-pumpoff-pump coronary-artery bypass surgery[J]. N Engl J Med, 2009, 361(19): 1827−1837.
[6] Racz MJ, Hannan EL, Isom OW,. A comparison of short- and long-term outcomes after off-pump and on-pump coronary artery bypass graft surgery with sternotomy[J]. J Am Coll Cardiol, 2004, 43(4): 557−564.
[7] Sá MP, Ferraz PE, Escobar RR,. Off-pumpon-pump coronary artery bypass surgery: meta-analysis and meta-regression of 13 524 patients from randomized trials[J]. Rev Bras Cir Cardiovasc, 2012, 27(4): 631−641.
[8] Feng ZZ, Shi J, Zhao XW,. Meta-analysis of on-pump and off-pump coronary arterial revascularization[J]. Ann Thorac Surg, 2009, 87(3): 757−765.
[9] Mishra Y, Wasir H, Kohli V,. Concomitant carotid endarterectomy and coronary bypass surgery: outcome of on-pump and off-pump techniques[J]. Ann Thorac Surg, 2004, 78(6): 2037−2042.
[10] Murzi M, Caputo M, Aresu G,. On-pump and off-pump coronary artery bypass grafting in patients with left main stem disease: a propensity score analysis[J]. J Thorac Cardiovasc Surg, 2012, 143(6): 1382−1388.
[11] D’Ancona G, Saez de Ibarra JI, Baillot R,. Determinants of stroke after coronary artery bypass grafting[J]. Eur J Cardiothorac Surg, 2003, 24(4): 552−556.
[12] Filsoufi F, Rahmanian PB, Castillo JG,. Incidence, topography, predictors and long-term survival after stroke in patients undergoing coronary artery bypass grafting[J].Ann Thorac Surg, 2008, 85(3): 862−870.
[13] Cao L, Li Q, Wang WH,. Influence of previous cerebral infarction on postoperative recovery in patients undergoing coronary artery bypass grafting[J]. Chin J Thorac Cardiovasc Surg, 2010, 26(3): 184−186. [曹 莉, 李 琴, 王文化, 等. 术前脑梗死对冠状动脉旁路移植术后恢复的影响[J]. 中国胸心血管外科临床杂志, 2010, 26(3): 184−186.]
(编辑: 李菁竹)
Long-term outcome of patients with coronary heart diseases and carotid arteriostenosis after coronary artery bypass surgery
LIU Shuai, GAO Chang-Qing*, REN Chong-Lei, XIAO Cang-Song, WANG Rong, WU Yang
(Department of Cardiovascular Surgery, Chinese PLA General Hospital, Beijing 100853, China)
To investigate the effect of on-pump and off-pump procedures on postoperative cerebral complications and survival rate after coronary artery bypass grafting (CABG).From June 2003 to June 2013, a total of 159 patients [(67.0±7.5) years old, 118 males and 41 females] with carotid arteriostenosis and coronary heart diseases, accepted isolated CABG in our department. They were divided into on-pump group (=95) and off-pump group (=64). The prevalence of postoperative cerebral complications and the survival rate after CABG were compared and retrospectively analyzed.Follow-up was done for 146 patients with a rate of 93.6%, and a duration of (46.3±25.3) months, ranging from 6 to 120 months. Ten patients had neurological symptoms, including 2 of cerebral hemorrhage and 8 of stroke. Seventeen patients died during the follow-up (4 due to cerebral complications, 1 esophagus cancer, 1 lung cancer, and 11 cardiogenic reasons) within average 41 months postoperatively (ranging from 4 to 72 months). There was no statistical difference in prevalence of postoperative cerebral complications and the survival rate between on-pump and off-pump groups (>0.05).On-pump and off-pump procedures have no significant difference in the effect on postoperative cerebral complications and survival rate in the patients with carotid arteriostenosis and coronary heart diseases.
coronary artery bypass; coronary disease; carotid stenosis; stroke; on-pump; off-pump
(BWS11J030).
R654.33; R543.3; R543.4
A
10.3724/SP.J.1264.2014.00081
2014−03−28;
2014−04−04
全军医学科技“十二五”重点项目(BWS11J030)
高长青, E-mail: gaochq301@yahoo.com