The orthopedic damage control in pelvic ring fractures: when and why-a multicenter experience of 10 years' treatment
2014-03-22GabrieleFalzaranoAntonioMediciSerafinoCartaPedragGruborMattiaFortinaLuigiMeccarielloPaoloFerrata
Gabriele Falzarano, Antonio Medici, Serafino Carta, Pedrag Grubor, Mattia Fortina, Luigi Meccariello*, Paolo Ferrata
1U.O.C. Orthopedics and Traumatology, Azienda Ospedaliera “Gaetano Rummo”, Benevento, Italy
2Department of Medical and Surgical Sciences and Neuroscience, Section of Orthopedics and Traumatology, University of Siena, University Hospital “Santa Maria alle Scotte”, Siena, Italy
3Orthopedics and Traumatology, Klinical Center University of Banja Luka, Banja Luka, Bosnia and Herzegovina
The orthopedic damage control in pelvic ring fractures: when and why-a multicenter experience of 10 years' treatment
Gabriele Falzarano1, Antonio Medici1, Serafino Carta2, Pedrag Grubor3, Mattia Fortina2, Luigi Meccariello2*, Paolo Ferrata2
1U.O.C. Orthopedics and Traumatology, Azienda Ospedaliera “Gaetano Rummo”, Benevento, Italy
2Department of Medical and Surgical Sciences and Neuroscience, Section of Orthopedics and Traumatology, University of Siena, University Hospital “Santa Maria alle Scotte”, Siena, Italy
3Orthopedics and Traumatology, Klinical Center University of Banja Luka, Banja Luka, Bosnia and Herzegovina
Objectives: To report our experience of regional referral center for the pelvis. Methods: We treated 526 pelvic fractures from January 2004 to December 2014 in three regional reference centers for pelvic trauma. Men were 480 and women were 46 and ages ranged from 16 to 93 years old. Car (65%) and farm (20%) crashes were the most frequent causes of pelvis fractures. Injury severity scores ranged from 9.0 to 75.0, with a mean of 37.5. A defined algorithm for fracture management has been in place and employed to assure adequate resuscitation and fracture care.
Results: There were 24 deaths in total (4.56%). Sixty three (11.98%) patients underwent angioembolization for control of bleeding (12 deaths). The average amount of blood transfused was 8.3 IU. Hospital lengths of stay ranged between 1-35 days. Among the 502 alive patients, 55.98% were able to be discharged at home while the remaining 44.02% being transferred to various rehabilitation facilities or extended care facilities. Conclusions: The goal of initial management is to restore vital indicators, urinary excretion function and protect the patient from infectious complications. An emergency decisional algorithm helps manage hemodynamic instability. Initial bone and ligament procedures should reduce displacement and make it possible for the patient to wait until his condition is stable enough for definitive surgical fixation.
ARTICLE INFO
Article history:
Received 30 Nov 2014
Received in revised form 2 Dec 2014
Accepted 23 Dec 2014
Available online 30 Dec 2014
Orthopedic damage control
Pelvic ring fractures
External fixation
Bleeding
C-clamp
Pubis belt
Conservative
Packing
1. Introduction
The severe fractures of the pelvic girdle in patients with multiple trauma often require a stabilization in emergency. The pelvic ring fractures are not uncommon and occurr within the severe trauma, and it is a complex problem that often requires for proper conservative or surgical treatments. specialized professional skills such as those of the surgeon of casualty, the radiologist, traumatologistorthopedist, urologist and eventually the neurosurgeon are required[1]. The pelvic fractures are by high-energy pelvic fractures (HE-PRFs) and low-energy pelvic fractures (LEPRFs). The incidences of HE-PRF and LE-PRF were 23 per 100 000 persons in New South Wales region in Australia[2], and the mortality was 23% divided into: HE-PRF: 7%; LEPRF: 2%; prehospital deaths (PD-PRF: 33%)[2]. In a German multicentric study, among 3 260 patients with pelvic and acetabular fractures, 61.7% of the patients were multiply injured; 12.2% were suffering a complex pelvic trauma defined as a pelvic injury with concomitant soft tissue injury[3].
The pelvis is a bony structure complex, consisting of several segments that form a solid ring, which protects organs (vascular structures, genital, urinary and gastrointestinal) it contains[1]. The pelvic ring fractures account for 3%-4% of all fractures and occur with an incidence of 20% in poly-traumatized patients, which can be considered a reliable indicator of high-energy trauma[1].The structural damage can be due to a car accident (60%-80%), the fall from the top (10%-30%) or a trauma crush (5%-10%)[1]. Direct result of the intensity of the trauma is the high frequency (90%) of lesions associated to other parts of the body, especially to the central nervous system and the trunk, which often adversely affect the patient’s prognosis[1]. This type of fracture is a significant disease because it is burdened with high social costs. In fact, it is common in the age groups of younger (first cause of death in the first four decades of life) with a high mortality rate and with a high percentage of post-traumatic comorbility often disabling, such as chronic pain, abnormal gait, neurological deficits and urinary and sexual problems (incontinence, impotence in men and alterations in the birth canal in women), so about 70%-80% of patients do not resume work activities prior to the pathological event[1]. We report our experience of regional reference centers for pelvic trauma.
2. Materials and methods
Our perspective research was conducted from January 2010 to December 2014 at the U.O.C. Orthopedics and Traumatology, Gaetano Rummo in Benevento, Italy; U.O.C. Orthopedics and Traumatology Universitaria, AOUS Policlinico Santa Maria alle Scotte in Siena, Italy and Orthopedics and Traumatology, Klinical Center University of Banja Luka Bosnia and Herzegovina. We treated 526 consecutive patients with pelvic ring fractures.
This group of patients was composed of 526 patients with an average age of 34.6 (range 16-93) and gender ratio (M: F) of 6.08:1 (280:46) (Table 1). The range of age are: 16-35 years old (n=242; 46.00%), 36-50 years old (n=226; 42.97%), 51-59 years old (n=40; 7.60%) and >60 yaers old (n=18; 3.43%).
Before trauma, patients’ occupations consisted of agricultural activity, industrial sector, tertiary industry and unoccupied (Table 1). Types of trauma accidents experienced by patients were fall from height, traffic accident, agriculture accident and other accidents (Table 1).
The pelvic ring fractures were classified with Tile’s classification[1] in patients as stable in 24.8% (type A injury), rotationally unstable in 44.7% (type B injury), and unstable in translation in 30.5% (type C injury) of the patients (Table 1).
All patients entering the emergency room had the XR standard and computed tomography (CT) with 3D reconstructions and pre-operative examinations. At admission to the emergency room, the 526 patients had an average injured severity score of 37.5 point (range 9-75) and they had the following associated injures: cerebral concussion, fat embolism, hemopneumothorax, liver injuries, spleen injuries, bowel injuries, urogentital injuries, femur injuries, tibia injuries, rib fractures, clavicle fracture, humerus fractures, forearm fractures, metatarsal fractures, patella fractures, acetabulum fracture, spine fractures, ankle fractures and wrist fractures (Table 2).
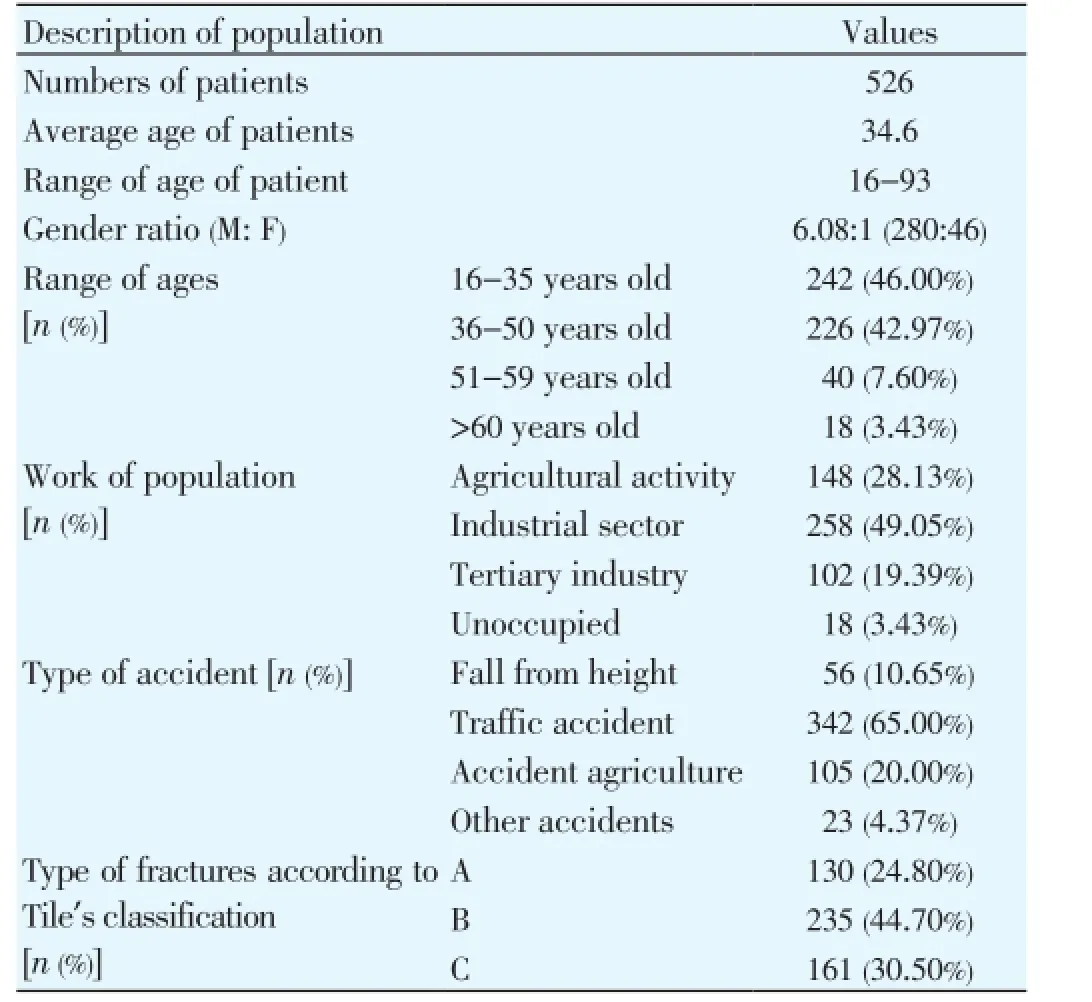
Table 1 Descriptions of population.

Table 2 Description of injured severity score and associated injures in the floating knee.

Figure 1. Alghorithm of treatment of hemodynamically unstable patient suffered of pelvic ring injuries[4].
Upon admission to the emergency room the patients had an average glasgow coma score of 12.5 points (range 8-15) (Table 2). We performed the initial emergency orthopedic treatments according an algorithm[4] and pyramid of total care (Figures 1 and 2). A total of 439 patients (83.47%) were hemodynamic stable, while 87 (16.53%) unstable. The 87 pathients were treated by packing in 24 cases (4.56%) and angio-embolization in 63 patients (11.98%) (Table 2).
The criteria chosen for the evaluation of the treatments was: mortality, amount of blood transfused, length of permanence in hospital, type of demission, miscellanea complication during the treatment in hospital.
Patients were excluded if they died before arriving at hospital. The data were imported in an electronic spreadsheet for further processing and statistical analysis.

Figure 2. The pyramid of total care in pelvic ring injuries.
The orthopedics damage control was performed by external fixation in 352 (84.12%) patients; C-clamp in 10 patients (8.92%); pubis belt in 22 patients (6.96%); circumferential sheeting in 22 patients (4.18%) and conservative in 120 patients (22.81%) (Table 2). Patients were treated according to the Helsinki Declaration of ethical standards.
3. Results
Tweenty four patients died in this group (4.56%) during the permanence in hospital, among which 12 (2.28%) patients died during the angio-embolization for cardiac and pressure shocks. The other 12 (2.28%) patients died after the angioembolization which were classified by: three for deep vein thrombosis; three for intra-cranic problems, four for comorbidities; two disseminated intravascular coagulation (Table 3). Only 63 (11.98%) patients underwent angioembolization for control of bleeding and 3 recived a vena cava filter. The average amount of blood transfused was 8.3 IU (range 2-16 IU).
Average Days for the second surgery (range) was 8.4 days (range 7-12) and in all 406 (77.18%) cases underwent surgery of open reduction and internal fixation (ORIF) withplates and wires (Table 3). Two types of complications were distinguished, damage control and early internal fixation complications (Table 3). A total of 24 (4.56%) complications were in damage control, the most frequent ones included decubitus in 10 (41.67%) patients (4 decubitus by pelvic belt, 3 by circumferential sheeting and 3 by rest in bed), erroneous insertion of an C-clamp implant in 5 (20.83%) and pin tract infection in external fixation in 5 (20.83%) patients and 4 (16.67%) external fixation’s pin implant failure (Table 3). We had 16 early post-operative internal fixation complications requiring repeat surgery that were early wound infection in 4, femur cutaneous nerve injury in 10 and hematoma which needed exploration in 2 patients (Table 3). At the demission, 281 of 502 alive patients were able to be discharged home while the remaining 221 being transferred to various rehabilitation facilities or extended care facilities (Table 3).

Table 3 Description of our results.
4. Discussion
Fractures of the pelvic ring comprise about 2% of all fractures, but the incidence is increasing due to increasing numbers of high-speed vehicular crashes and suicide attempts[5]. Mortality associated with isolated pelvic injury, independent of severity, has been reported to be low (1%-2%)[5]. Among multiply injured victims of blunt trauma, however, almost 20% have injuries to the pelvic ring[5]. Upon arrival in the emergency department, patients should be resuscitated according to the guidelines of the Advanced Trauma Life Support Course of the American College of Surgeons’ Committee on Trauma[4-6]. Hemodynamically unstable pelvic trauma is a major problem in trauma surgery and even in the most experienced trauma centers[4-6]. A long living debate in the literature, with plenty of classifications and protocols, has not still established the best treatment strategy for these patients. Although the source of bleeding is non-arterial in most cases, arterial injury can account for hemodynamic instability in 10%-20% of patients[5,7,8]. Various arteries that cross the pelvis, including the internal iliac, obturator, superior gluteal and pudendal arteries, have been found to be the cause of bleeding in these fractures[9]. More than 40% mortality rate reported in these patients indicates the relatively severe nature of the injury and its associated poor prognosis. Open surgical exploration of arterial bleeding is not recommended: access to the iliac arteries is difficult to gain, and disruption of the pelvic hematoma and consequential loss of tamponed effect can produce massive, uncontrollable and often fatal bleeding[10,11]. In emergency plain radiographs of the chest and pelvis must be obtained at this stage[5]. CT is undeniably the most accurate means to identify peritoneal and especially retroperitoneal injuries, but the CT suite is an unsafe environment for the unstable trauma patient. An essential consideration in resuscitating these patients is thermal control, with a strict avoidance of early hypothermia, which exacerbates traumatic coagulopathies[5]. What the orthopedic trauma surgeon must keep in mind in emergency when called to treat the injuries of the pelvic girdle? These are the questions that must be asked: is a hemodynamicallyunstable fracture? Is it an intra-abdominal bleeding? Is this a biomechanically unstable fracture? We must remember injury severity score is the most important predictor in defining mortality in patients with pelvic fracture and not the type of pelvic instability[12]. The first aid born on the place of accident[4]. Basically, the principles of trauma management of multiply injured patients with lifethreatening hemorrhage from mechanically unstable pelvic fractures are divided into two main time periods. On the one hand, there is the emergency stabilization of the pelvic ring as the most important goal within the acute period to control the bleeding, at least with extraperitoneal tamponed if necessary. On the other hand, once the hemorrhaging has been stopped, the “late” and definitive internal fracture stabilization of the pelvis should be performed depending on the fracture pattern[13]. If the term damage control comes from US Navy: “Capacity of a ship to absorb damage and maintain mission integrity”, which is the right orthopedic device that answers the questions that must be asked prior to the orthopedic damage control in pelvic ring injuries? Circumferential pelvic sheeting provides patient comfort and noninvasive, rapid, and temporary pelvic ring stability. A bed sheet is readily available, inexpensive, easily applied around the pelvis, and disposable[14]. Circumferential pelvic belt compression by means of the pelvic sling is an effective, noninvasive, and safe stabilization approach that is well suited for emergent, temporary management of open-book pelvic fractures at the accident scene[15]. The limit of the principals is the duration: Let in the more than 72 h have a high risk of pressure sores. For this reason, if you need a long-term immobilization, the temporary garrison should be replaced as soon as possible by final external fixation[15]. Another limitation is the inability to dominate with these two devices, the serious biomechanical instability of the pelvis[15]. The conservative treatment is good choice only in very stable pelvic ring injures[1]. The pelvic packing is for patients who remain in extremis with a probable retroperitoneal cause in spite of aggressive resuscitative efforts should not be transported to a distant angiography suite, especially if delay is involved[16]. These are often patients at risk for abdominal compartment syndrome, and who therefore need an open peritoneal cavity for adequate cardiovascular physiologic support after surgery[16]. If we take into account that the pelvis and abdomen are a cylinder and the mathematical formula “V= ϖh/3(r1 2+r1 r2+ r2 r2)”to determine the loss of blood, we understand the need to use two types of devices: C-clamp or external fixation[17,18]. To deal with posteriorly unstable fractures, Ganzet al.developed a pelvic C-clamp, now available in most trauma units[17]. It acts like a simple carpenter’s clamp and can exert transverse compression directly across the sacroiliac joint. Experimental data[17] have shown that an average compression force of 342 N can be applied to the area of this joint[5]. C-clamp application can not only be difficult but dangerous in cases of comminuted sacral fractures. Neurovascular injury can occur due to crushing of the sacrum. Marshet al. have reported pelvic penetration of the stabilizing pins and over-compression of the clamps[19]. The prongs of the C-clamp can be misapplied and have been accidentally placed into the true pelvis through the greater sciatic notch[5]. The anterior pelvic external fixation frame (APEFF) can be applied in the trauma bay, intensive care unit or operating room in around 20-30 min, that is a great advance[5]. Immediate APEFF of an unstable pelvic injury has been the mainstay of acute stabilization for the past few decades[5]. A Lot of authors[4] reported in their paper the reduction of mortality rates from 22% to 8% by adding acute APEFF to their hospital resuscitation protocol. Based on their results, they concluded that skeletal stabilization of pelvic injury should be viewed as a part of resuscitation rather than reconstruction. Köhleret al.[20] and others authors[21-24] have also documented decreased transfusion needs and reduced mortality with the use of anterior external fixator. Therefore we have also recommended immediate application of external fixation for hemodynamically unstable patients, and consider it a life-saving procedure. Another advance of APEFF is the prophylactic stabilization in all patients demonstrating bony instability, as even those patients who are initially hemodynamically stable on presentation may decompensate later[4]. The anterior fixator is thought to contribute to hemostasis by maintaining a reduced pelvic volume, allowing tamponed, and by decreasing bony motion at the fracture site, allowing clots to stabilize[5]. The pelvic fractures most amenable to this form of treatment are the open book fracture, and the unstable shear type when combined with longitudinal traction[21-24]. According Kellam[23], lateral compression injuries incur fewer benefits from this method. We do not agree with Kellam, because we believe adding the assembly of the routine APEFF, pins with power trochanteric and bars in distraction/compression can dominate all vector forces on the different floors of the space they have created the pelvic instability (Example: Figure 3). Dickson and Matta have demonstrated worsening of posterior deformity in patients treated with APEFF and it can aggravate the posterior instability in an unstable fracture configuration[25]. The orthopedic damage control is a moment, the unstable fractures of the pelvis require ORIF[26]. We performed the ORIF at an average of 8.4 (range 7-12) weeks after the orthopedic damage control according the theory of second hit window[27]. All complications occurred after damage control or ORIF are common complications that can occur with the devices used in the treatment of pelvic ring injures[5,15,25,28].
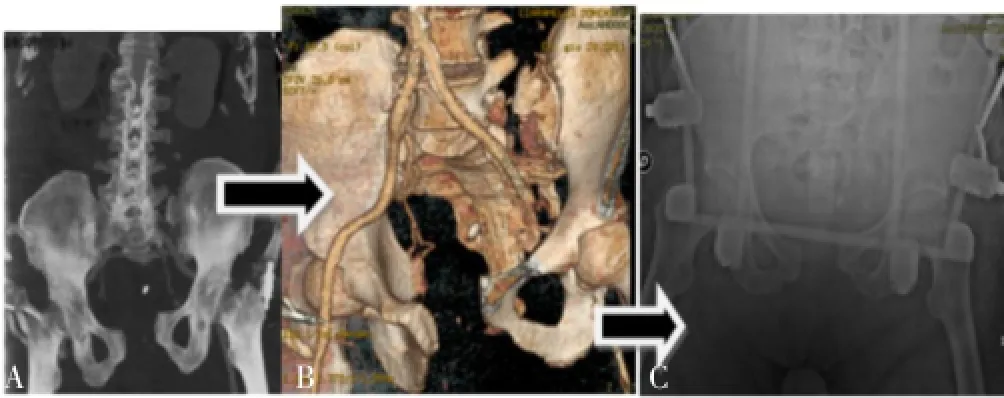
Figure 3. CT, 3D CT and XR of pelvic vertical shear instability.A: CT; B: 3D CT; C: XR showing the reduction of pelvic vertical shear instability by APEFF.
The goal of treatment is to stabilize the initial vital signs, urinary function and protect the patient from infectious complications. A decision algorithm used in emergency helps manage hemodynamic instability. The procedures that allow legamentotaxis and osteotaxis and should be applied in an emergency until the patient’s condition is stable enough for the surgical fixation final.
Conflict of interest statement
The authors report no conflict of interest.
[1] Grubor P, Milicevic S, Biscevic M, Tanjga R. Selection of treatment method for pelvic ring fractures. Med Arh 2011; 65(5): 278-282.
[2] Balogh Z, King KL, Mackay P, McDougall D, Mackenzie S, Evans JA, et al. The epidemiology of pelvic ring fractures: a population-based study. J Trauma 2007; 63(5): 1066-1073.
[3] Gänsslen A, Pohlemann T, Paul C, Lobenhoffer P, Tscherne H. Epidemiology of pelvic ring injuries. Injury 1996; 27(Suppl 1): S-A13-20.
[4] Magnone S, Coccolini F, Manfredi R, Piazzalunga D, Agazzi R, Arici C, et al. Management of hemodynamically unstable pelvic trauma: results of the first Italian consensus conference (cooperative guidelines of the Italian Society of Surgery, the Italian Association of Hospital Surgeons, the Multispecialist Italian Society of Young Surgeons, the Italian Society of Emergency Surgery and Trauma, the Italian Society of Anesthesia, Analgesia, Resuscitation and Intensive Care, the Italian Society of Orthopaedics and Traumatology, the Italian Society of Emergency Medicine, the Italian Society of Medical Radiology-Section of Vascular and Interventional Radiologyand the World Society of Emergency Surgery). World J Emerg Surg 2014; 9(1): 18.
[5] Mohanty K, Musso D, Powell JN, Kortbeek JB, Kirkpatrick AW. Emergent management of pelvic ring injuries: an update. Can J Surg 2005; 48(1): 49-56.
[6] American College of Surgeons. Advanced trauma life support (ATLS) student manual. 6th ed. Chicago: American College of Surgeons; 1997.
[7] Gansslen A, Giannoudis P, Pape HC. Hemorrhage in pelvic fractures: who needs angiography? Curr Opin Crit Care 2003; 9: 515-523.
[8] Huittinen VM, Slatis P. Postmortem angiography and dissection of the hypogastric artery in pelvic fractures. Surgery 1973; 73: 454-462.
[9] O’Neill PA, Riina J, Sclafani S, Tornetta P 3rd. Angiographic findings in pelvic fractures. Clin Orthop Relat Res 1996; (329): 60-67.
[10] Panetta T, Sclafani SJ, Goldstein AS, Phillips TF, Shaftan GW. Percutaneous transcatheter embolization for massive bleeding from pelvic fractures. J Trauma 1985; 25: 1021-1029.
[11] Ben-Menachem Y, Coldwell DM, Young JW, Burgess AR. Hemorrhage associated with pelvic fractures: causes, diagnosis and emergent management. AJR Am J Roentgenol 1991; 157(5): 1005-1014.
[12] Lunsjo K, Tadros A, Hauggaard A, Blomgren R, Kopke J, Abu-Zidan FM. Associated injuries and not fracture instability predict mortality in pelvic fractures: a prospective study of 100 patients. J Trauma 2007; 62(3): 687-691.
[13] Burkhardt M, Culemann U, Seekamp A, Pohlemann T. [Strategies for surgical treatment of multiple trauma including pelvic fracture. Review of the literature]. Unfallchirurg 2005; 108(10): 812, 814-820. German.
[14] Routt ML Jr, Falicov A, Woodhouse E, Schildhauer TA. Circumferential pelvic antishock sheeting: a temporary resuscitation aid. J Orthop Trauma 2006; 16(1): 45-48.
[15] Simpson T, Krieg JC, Heuer F, Bottlang M. Stabilization of pelvic ring disruptions with a circumferential sheet. J Trauma 2002; 52: 158-161.
[16] Ertel W, Keel M, Eid K, Platz A, Trentz O. Control of severe hemorrhage using C-clamp and pelvic packing in multiply injured patients with pelvic ring disruption. J Orthop Trauma 2001; 15(7): 468-474.
[17] Ganz R, Krushell RJ, Jakob RP, Kuffer J. The antishock pelvic clamp. Clin Orthop Relat Res 1991; (267): 71-78.
[19] Marsh JL, Slongo TF, Agel JNA, Broderick JS, Creevey W, DeCoster TA, et al. Fracture and dislocation classification compendium-2007: Orthopaedic Trauma Association classification, database and outcomes committee. J Orthop Trauma 2007; 21(10 Suppl): S1-S133.
[20] Köhler D, Sellei RM, Sop A, Tarkin IS, Pfeifer R, Garrison RL, et al. Effects of pelvic volume changes on retroperitoneal and intra-abdominal pressure in the injured pelvic ring: a cadaveric model. J Trauma 2011; 71(3): 585-590.
[21] Ghaemmaghami V, Sperry J, Gunst M, Friese R, Starr A, Frankel H, et al. Effects of early use of external pelvic compression on transfusion requirements and mortality in pelvic fractures. Am J Surg 2007; 194(6): 720-723.
[22] Gylling SF, Ward RE, Holcroft JW, Bray TJ, Chapman MW. Immediate external fixation of unstable pelvic fractures. Am J Surg 1985; 150(6): 721-724.
[23] Kellam JF. The role of external fixation in pelvic disruptions. Clin Orthop Relat Res 1989; (241): 66-82.
[24] Slätis P, Karaharju EO. External fixation of unstable pelvic fractures: experience in 22 patients treated with trapezoid compression frame. Clin Orthop Relat Res 1980; (151): 73-80.
[25] Dickson KF, Matta JM. Skeletal deformity after anterior external fixation of the pelvis. J Orthop Trauma 2009; 23(5): 327-32.
[26] Templeman DC, Simpson T, Matta JM. Surgical management of pelvic ring injuries. Instr Course Lect 2005; 54: 395-400.
[27] Pape HC, van Griensven M, Rice J, Gänsslen A, Hildebrand F, Zech S, et al. Major secondary surgery in blunt trauma patients and perioperative cytokine liberation: determination of the clinical relevance of biochemical markers. J Trauma 2001; 50(6): 989-1000.
[28] Langford JR, Burgess AR, Liporace FA, Haidukewych GJ. Pelvic fractures: part 2. Contemporary indications and techniques for definitive surgical management. J Am Acad Orthop Surg 2013; 21(8): 458-68.
ment heading
10.1016/S2221-6189(14)60044-5
*Corresponding author: Luigi Meccariello, MD, Department of Medical and Surgical Sciences, and Neuroscience, Section of Orthopedics and Traumatology, University of Siena, University Hospital “Santa Maria alle Scotte”, Viale Bracci 1, 53100 Siena, Italy.
Tel: +39 329 9419574
E-mail: drlordmec@gmail.com
杂志排行
Journal of Acute Disease的其它文章
- Posterior reversible leukoencephalopathy syndrome presenting in a post-partum, 25-year-old-female with concomitant subarachnoid hemorrhage
- Cardioprotective potential of hydro-alcoholic fruit extract of Ananas comosus against isoproterenol induced myocardial infraction in Wistar Albino rats.
- Patients with the tako-tsubo cardiomyopathy-clinical evaluation and outcome
- Acute brain hemorrhage in dengue
- The epidemiology of tick-borne relapsing fever in Bijar County, North-Western Iran
- Heart, tracheo-bronchial and thoracic spine trauma. Succesful multidisciplinary management: a challenging thoracic politrauma
