Heart, tracheo-bronchial and thoracic spine trauma. Succesful multidisciplinary management: a challenging thoracic politrauma
2014-03-22SergioNicolaFortiParriGianMarcoGuiducciKenjiKawamukaiCarloConiglioGiovanniGordiniFedericoDeIureRoccoTrisoliniSalomoneDiSaverioGregorioTugnoli
Sergio Nicola Forti Parri, Gian Marco Guiducci, Kenji Kawamukai, Carlo Coniglio, Giovanni Gordini, Federico De Iure, Rocco Trisolini, Salomone Di Saverio, Gregorio Tugnoli
1Thoracic Surgery Unit, Presidio Ospedaliero Maggiore–Bellaria, Bologna, Italy
2Department of Emergency, Maggiore Hospital, Bologna, Italy
3Department of Orthopedics and Traumatology-Spine Surgery, Maggiore Hospital, Bologna, Italy
4Thoracic Endoscopy and Pulmonology Unit, Presidio Ospedaliero Maggiore–Bellaria, Bologna, Italy
5Department of Emergency Surgery, Maggiore Hospital, Bologna, Italy
Heart, tracheo-bronchial and thoracic spine trauma. Succesful multidisciplinary management: a challenging thoracic politrauma
Sergio Nicola Forti Parri1*, Gian Marco Guiducci1, Kenji Kawamukai1, Carlo Coniglio2, Giovanni Gordini2, Federico De Iure3, Rocco Trisolini4, Salomone Di Saverio5, Gregorio Tugnoli5
1Thoracic Surgery Unit, Presidio Ospedaliero Maggiore–Bellaria, Bologna, Italy
2Department of Emergency, Maggiore Hospital, Bologna, Italy
3Department of Orthopedics and Traumatology-Spine Surgery, Maggiore Hospital, Bologna, Italy
4Thoracic Endoscopy and Pulmonology Unit, Presidio Ospedaliero Maggiore–Bellaria, Bologna, Italy
5Department of Emergency Surgery, Maggiore Hospital, Bologna, Italy
We reported the case of a 36 years old woman involved in a car accident and admitted to the Emergency Room with critical conditions. A CT scan showed hemopericardium, pneumomediastinum and D2 unstable vertebral fracture; then a sternotomy was promptly performed. After admittance to Intensive Care Unit a bronchoscopy showed a tear of the posterior wall of the trachea and the complete disruption of the left main bronchus with a 2 cm gap beetwen two consecutive cartilage rings. D2 fracture would have required stabilization, but pronation of the patient was contraindicated by the bronchial rupture. On the nineth day the vertebral fracture was stabilized, thus allowing a lateral decubitus and a left thoracotomy. The bronchial laceration was wrapped all around with a pedicled pericardial flap and a bronchial stent was placed inside the gap with a pediatric bronchoscope. Postoperative course was uneventful and the patient was transferred to the Physical Rehabilitation Unit after 23 d. The successful outcome of this case is the result of multidisciplinary management where every decision was shared by each specialist. From the surgical point of view survival is uncommon in such severe association of lesions. The use of pericardium wrap together with a bronchial stent represents an innovative solution to treat a complicated bronchial disruption.
ARTICLE INFO
Article history:
Received 24 October 2014
Received in revised form 22 November 2014
Accepted 12 December 2014
Available online
Bronchial disease
1. Introduction
Blunt trauma of the chest consequent to car accidents can cause rapidly lethal multiple organ injuries. The rupture of a cardiac chamber, most likely an atrium, following blunt chest trauma leads to immediate death in 80%-90% of patients[1]. Trauma of the major airways with bronchial rupture leads to immediate death in many patients and to death after hospitalisation in 30% of the other patients[2]. About 10% of major tracheo-bronchial traumas are associated with cervical spinal cord injury[3]. The combination of cardiac rupture, tracheo-bronchial rupture, cervical and thoracic vertebral fractures after blunt trauma to the chest is one of the toughest challenges that a Trauma Center can face.
2. Case report
2.1. Day 1
A 36 years old female was involved in a road car crash while not wearing seatbelts. On scene Glasgow Coma Scale was 6; oro-tracheal intubation was performed, and the cervical spine was stabilized and crystalloid fluid infusion was started. At the Emergency Room, blood pressure was 80/40. Chest X-ray and FAST ultrasound showed no majoralterations. A cardio-pulmonary arrest was successfully treated in the Emergency Room with CPR and ALS, and a weak haemodinamical compensation was restored. A left pleural tube was placed based on FAST diagnosis of left minimal haemopneumothorax.
A subsequent whole body chest CT scan revealed (Figure 1): haemopericardium, pneumomediastinum, D2 unstable vertebral fracture and minor injuries (C2 stable vertebral fracture, non complicated head trauma, multiple pulmonary contusions, multiple non complicated right costal fractures and minimal abdominal effusion).

Figure 1. CT scan of pneumomediastinum, hemopericardium and D2 unstable vertebral fracture.
Cardiocirculatory parameters improved dramatically after 100 cc of blood were drained by us guided by pericardiocentesis. The patient was then transferred to the Operating Room where urgent exploratory sternotomy was performed.
After opening the pericardial sac, more than 300 cc of blood exited and this was immediately beneficial to cardiac kinetics and blood pressure. A 1 cm blunt laceration of the right auricle was detected, clamped with a haemostatic clamp and stitched. No further cardiac lesions were found after complete exploration. No air leakage was detectable from airways and lungs.
The patient was transferred to the Intensive Care Unit where a bronchoscopy, performed to assess the cause of pneumomediastinum, showed a laceration of the trachea in its posterior wall starting at approximately 1.5 cm from the carina, and a 2.5 cm rupture of the left main stem bronchus in its posterior-medial aspect starting from just below the main carina (Figure 2). Only the hematoma of the peribronchial tissue preserved continuity of the airway. Low positive pressure ventilation was maintained, and in spite of the severe multiple traumatic lesions the clinical state of the patient was stable, with no air leakage from the chest drains. A subsequent CT scan demonstrated the reduction of the pneumomediastinum.

Figure 2. Endoscopic view and CT scan of complete rupture of the left main bronchus.
D2 unstable vertebral fracture at this point would have required surgical stabilization, but the pronation of the patient was held contraindicated in presence of the bronchial rupture. The distance between the margins of the bronchial rupture and the absence of cartilaginous rings prevented the feasibility of bronchial stenting.
A thoracotomy for the surgical treatment of the bronchial rupture was contraindicated in presence of the D2 unstable vertebral fracture.
Any treatment was then delayed: the patient was kept under low pressure mechanical ventilation, supine, curarized and under broad spectrum antibiotics. During the following days, chest drainage tubes were positioned bilaterally to drain pleural effusion; bronchoscopies were daily performed. The clinical condition remained stable. No signs of esophageal lesions were detected.
2.2. Day 4
The bronchoscopy showed improved conditions: fibrin and inflammatory tissue was covering tracheal laceration and narrowed the mediastinal chamber around the bronchial rupture; the evolution in a spontaneous stabilization of the bronchial wall was considered possible and vertebral stabilization was delayed.
2.3. Day 7
The bronchoscopic evidence was still stable, but there was no evolution towards spontaneous healing. Due to this stable condition, in order to reduce the risks of neurological iatrogenic damage, surgical indication was considered.
2.4. Day 9
D2 vertebral fracture was stabilized: a posterior fixation, extended from C5 to D4 was performed after detecting the simultaneous spondylolisthesis of C6-C7 vertebrae. In the course of pronation and spinal surgery bronchoscopic check showed that the bronchial wall partially collapsed. Surgery was completed under bipulmonary ventilation with no significant problem (Figure 3).

Figure 3. Stabilization of D2 vertebral fracture and the bronchial wall. A: D2 vertebral fracture was stabilized: a posterior fixation, extended from C5 to D4 was performed after detecting the simultaneous spondylolisthesis of C6-C7 vertebrae; B: The bronchial wall partially collapsed, but there was non evidence of perforation.
2.5. Day 10
After accomplishing vertebral stabilization, posterolateral thoracotomy could safely be performed: the aortic arch was mobilized in order to obtain a wide approach to distal trachea and main bronchi. The left main bronchus was exposed and the rupture identified; thick and firm peribronchial inflammatory tissue preserved the continuity of the airway but hindered the feasibility of a bronchial resection-anastomosis (Figure 4). A wide pericardial flap was prepared posteriorly, parallel to the phrenic nerve, to enforce the bronchial wall. In order to obtain adequate stiffness of bronchial wall a covered metal stent (Ultraflex, Boston Scientific®) was placed through the oro-tracheal tube and with the aid of a pediatric flexible bronchoscope over the bronchial gap with a 2 cm proximal margin and a 1 cm distal margin. The pericardial flap was then wrapped 360 degrees around the location of the rupture, to reduce the risk that the endoprosthesis could migrate and damage vital structures (Figure 5). Placement of a silicone stent, which was an alternative we considered, was not feasible because of the need of mechanical ventilation and the high risk of further enlarging of the bronchial lesion while overcoming the rupture with the rigid bronchoscope.

Figure 4. Postero-lateral thoracotomy could safely be performed: the aortic arch was mobilized in order to obtain a wide approach to distal trachea and main bronchi. The left main bronchus was exposed and the rupture identified.
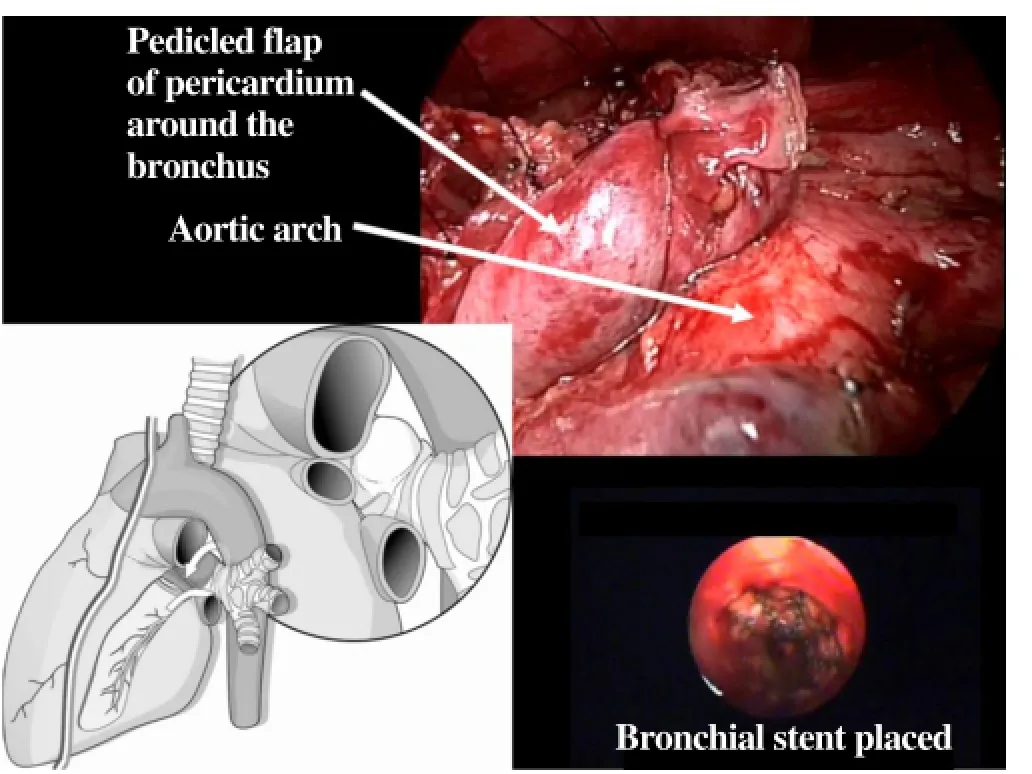
Figure 5. The pericardial flap was then wrapped 360 degrees around the location of the rupture. A covered metal stent was placed over the bronchial gap. (From Forti Parri and Boaron, “Surgical treatment of thoracic trauma: mediastinum”. In: Di Saverio et al. “Trauma Surgery” Volume 2, Springer 2014 with permission).
Both surgery and post-operative course were uneventful. The patient was gradually weaned from mechanic ventilation and three days after the bronchial surgery, a temporary tracheostomy was performed to allow easier bronchial cleaning (Figure 6).

Figure 6. CT scan of airways after surgery.
2.6. Day 23
The patient was transferred to the Rehabilitation Unit. The only surgical sequela was the left recurrent palsy, determined despite the isolation and the anatomical preservation of the left recurrent laryngeal nerve.
Complete bronchial healing was expected, even though a periodical bronchoscopic follow up was planned to monitor the possible mid-long term complications of the endobronchial prosthesis.
At 3-year follow-up, the patient has a nearly normal life, the only problems being the retention of mucus within the stent, and the need for periodical coagulation and removal of small granulomas arising form the proximal and distal uncovered tracts of the metallic stent. As the need for bronchoscopic management of these complication is slowly increasing in frequency, the possibility of a surgical management consisting in a bronchial end-to-end anastomosis is being considered.
3. Discussion
Patients with cardiac rupture following blunt chest trauma rarely reach the Operating Room, usually death occurs on scene or early in the Emergency Room. Several mechanisms of cardiac rupture have been debated; in the present case, the most reasonable explanation was the crushing of the cardiac chambers between the sternum and the spine[4]. Often, in patients who survive enough to the Operating Room, small atrial lacerations can be sutured via median sternotomy without the need of cardiopulmonary bypass. Ventricular laceration are instead usually rapidly lethal[5].
The integrity of the pericardial sac is fundamental to retain the cardiac tamponade and its quick diagnosis usually suggests an early transfer to the Operating Room[6]. Pericardial ultrasonography during FAST is usually the most valuable diagnostic tool to confirm the clinical suspect of cardiac tamponade even though in some cases, as the present case, the hemopericardium may not be quantified through ultrasound[7]. Once the cardiac tamponade is diagnosed, an early treatment with pericardiocentesis can be of great importance relieving the label cardiocirculatory balance.
The tracheobronchial damage was, in the present case, undiagnosed after the first chest CT scan. Total lack of air leaks from the pleural drain tube, moderate and stable pneumomediastinum and absence of subcutaneous emphysema allowed us to delay the bronchoscopic evaluation after the emergency sternotomy. Even though an Abruzzini/Perelman transmediastinal approach to the tracheal carina could be performed[8], with a deep and narrow surgical field, the most probable option would have been the left pneumonectomy[9].
Three pathogenetic mechanisms of airways transections can be taken into consideration[2]: the thorax compression with enlargement of its lateral diameter and traction of the main bronchi upon carinal trachea, the thoracic compression with sudden rise in endotracheal pressure, the sudden deceleration with high traction applied to fixed points, in particular to the carina. In only 17% of cases of airway damage, the lesion is located in the left main bronchus and in 8% of cases there are both tracheal and bronchial lesions[10]. The association of heart and left bronchial lesions in our opinion suggest a mechanism of burst from anteroposterior sudden compression.
The lack of air leak on this damage can be explained by the relative integrity of the hematoma of the peribronchial connective tissue. This probably interrupted the air supply which had initially generated the pneumomediastinum.
The absence of major symptoms related to the tracheobronchial damage, made it possible to maintain positive pressure ventilation. The bronchial damage was a clear surgical indication but the simultaneous presence of the unstable D2 vertebral fracture contraindicated the thoracotomic approach to the left main bronchus. Such overlapping of rare circumstances was much more limiting than the more frequent coexistence of a tracheal and bronchial lesions and a cervical spine damage, treatable with a simple external fixation with the patient lying in lateral position[3]. The surgical reparation of the dorsal spine fracture, whose treatment outsides this report, needs the prone position of the patient and consequent high risk of further worsening of the bronchial lesion.
So any further action was delayed to allow a better consolidation of the tracheo-bronchial damage and this approach in three days led to a dramatic improvement of the tracheal healing. Anyway the prolonged Intensive Care Unit stay could lead to the risk of neurological damage. To minimize this risk an active surgical treatment had to be planned in short times.
The vertebral stabilization treatment was performed with C5-D4 posterior fixation, after detecting the simultaneous spondylolisthesis of C6-C7 vertebrae. As expected, during the pronation, the bronchial stumps were stretched and compressed. This condition, bronchoscopically monitored, did not trigger any complication but confirmed to be at risk, without any reasonable expectance of spontaneous healing and restore of autonomous ventilation. Furtherly a late complication was expected to be the bronchial stenosis caused by the scarring that commonly follows the untreated bronchial fractures[11].
In the scientific literature there is no report of delayed bronchial reparation at such a short distance from the trauma. The immediate treatment of a bronchial rupture is performed debriding the bronchial margins and suturing the two bronchial ends with single interrupted sutures in Vycril®4/0 and suture buttressing, following the principles of airways reconstruction[12].
The treatment of late stenotic complications in late diagnosis of traumatic damage to the tracheobronchial tree has been widely described in literature and many different techniques have been used. Laser-assisted mechanical dilation[11], stenting[13], and surgery[14] have been widely reported. As for the endoscopic techniques, laser-assisted dilation is associated with risk of perforation and of possible recurrence, while stenting is possibly associated with several complications depending on the site and type ofstent used (metallic versus silicone). As a consequence periodical endoscopic follow-up is mandatory, especially in patients subjected to stent placement. Surgical resection of the stenotic tract, even after many years since trauma, guarantees excellent results and a low incidence of complications.
When planning bronchial repair, a direct resectionanastomosis was considered, but the presence of thick and woody inflammatory tissue would have required a large devascularization of the bronchial tissue. The presence of an optimal spontaneous aerostasis leads to the decision of preserving the airway and reinforcing it on two sides. In order to replace the cartilagineus skeleton of bronchus we positionned a self-expandable, silicon coated metal stent (Ultraflex, Boston Scientific®). The stent could jeopardize the weak airway wall represented by just peribronchial tissue, so a tight autologous tissue buttressing of the bronchus was decided. Several options of autologus tissue transposition were taken into consideration: the intercostal muscle was not viable for the inadequate vascular supply; the prepericardial fat tissue was damaged during the previous sternotomy and a pleural flap was considered too thin to ensure an adequate protection and stiffness. A pedunculated pericardial flap was considered the best option, even considering the excellent outcome of a previous similar case[15]. Other reliable alternatives in the event of complications or unsatisfactory conditions of the pericardium, were an omental flap or an extrathoracic muscle flap. The pericardium is a robust membrane with an excellent blood supply; its adaptability to the surgery of the airways is well established in pediatric surgery for tracheo-esophageal fistulae[16], in oncologic surgery to protect the anastomosis in sleeve resections[17], in heart-lung transplantation[18] and in the reconstruction of the pars membranacea in iatrogenic tracheal lacerations[19].
The preparation of the pedunculated pericardial flap is easy and safe, and the reconstruction of the residual pericardial defect is not necessary except when a pneumonectomy is performed[20].
Conflict of interest statement
The authors report no conflict of interest.
Acknowledgment
I want to acknowledge Dr. Maurizio Boaron, past Director of the Thoracic Surgery Unit of the Maggiore and Bellaria Hospitals. He was a great master able to transfer simply and entirely his surgical and clinical experiences.
[1] Khandhar SJ, Johnson SB, Calhoon JH. Overview of thoracic trauma in the United States. Thorac Surg Clin 2007; 17: 1-9.
[2] Kirsh MM, Orringer MB, Behrendt DM, Sloan H. Management of tracheobronchial disruption secondary to nonpenetrating trauma. Ann Thorac Surg 1976; 22: 93-101.
[3] Rossbach MM, Johnson SB, Gomez MA, Sako EY, Miller OL, Calhoon JH. Management of major tracheobronchial injuries: a 28-year experience. Ann Thorac Surg 1998; 65: 182-186.
[4] Nan YY, Lu MS, Liu KS, Huang YK, Tsai FC, Chu JJ, et al. Blunt traumatic cardiac rupture: therapeutic options and outcomes. Injury 2009; 40: 938–945.
[5] Embrey R. Cardiac trauma. Thorac Surg Clin 2007; 17: 87-93.
[6] Navid F, Gleason TG. Great vessel and cardiac trauma: diagnostic and management strategies. Semin Thorac Cardiovasc Surg 2008; 20: 31–38.
[7] Misao T, Yoshikawa T, Aoe M, Iga N, Furukawa M, Suezawa T, et al. Bronchial and cardiac roptures due to blunt trauma. Gen Thorac Cardiovasc Surg 2011; 59: 216–219.
[8] Perelman MI, Rymko LP, Ambatiello GP. Bronchopleural fistula: surgery after pneumonectomy. Int Trends Gen Thorac Surg 1987; 2: 407–412.
[9] Beale P, Bowley DM, Loveland J, Pitcher GJ. Delayed repair of bronchial avulsion in a child trought median sternotomy. J Trauma 2005; 58: 617–619.
[10] Symbas PN, Justicz AG, Ricketts RR. Rupture of the airways for blunt trauma: treatment of complex injuries. Ann Thorac Surg 1992; 54: 177–183.
[11] Glazer ES, Meyerson SL. Delayed presentation and treatment of tracheobronchial injuries due to blunt trauma. J Surg Educ 2008; 65: 302–308.
[12] Grillo HC. Repair of tracheobronchial trauma. In: Grillo HC, editor. Surgery of the trachea and bronchi. London: Decker Inc Hamilton; 2004.
[13] Madden BP, Loke TK, Sheth AC. Do expandable metallic airway stents have a role in the management of patients with benign tracheobronchial disease? Ann Thorac Surg 2006; 82: 274–278.
[14] Johnson SB. Tracheobronchial injury. Semin Thorac Cardiovasc Surg 2008; 20: 52–57.
[15] Boaron M, Kawamukai K, Forti Parri SN, Trisolini R. Treatment of an acquired esophageal-bibronchial benign fistula using an original combination of techniques. Interac Cardiovasc Thorac Surg 2010; 10: 156–158.
[16] Wheatley MJ, Coran AG. Pericardial flap interposition for the definitive management of recurrent tracheoesophageal fistula. J Pediatr Surg 1992; 27: 1122–1126.
[17] Weisel RD, Cooper JD, Delarue NC, Theman TE, Todd TR, Pearson FG. Sleeve lobectomy for carcinoma of the lung. J Thorac Cardiovasc Surg 1979; 78: 839–849.
[18] Haverich A, Frimpong-Boateng K, Wahlers T, Schäfers HJ. Pericardial flap-plasty for protection of the tracheal anastomosis in heart-lung transplantation. J Card Surg 1989; 4: 136–139.
[19] Foroulis CN, Simeoforidou M, Michaloudis D, Hatzitheofilou K. Pericardial patch repair of an extensive longitudinal iatrogenic rupture of the intrathoracic membranous trachea. Interact Cardiovasc Thorac Surg 2003; 2: 595–597.
[20] Anderson TM, Miller JI Jr. Use of pleura, azygos vein, pericardium and muscle flaps in tracheobronchial surgery. Ann Thorac Surg 1995; 60: 729–733.
cardiumDocument heading
10.1016/S2221-6189(14)60055-X
*Corresponding author: Sergio Nicola Forti Parri, MD, Thoracic Surgery Unit, Presidio Ospedaliero Maggiore-Bellaria, Largo Nigrisoli 2, Bologna, Italy.
Tel: +39 0516478849, +39 3392803842
Fax: +39 0516478209
E-mail: sergionicola.fortiparri@ausl.bo.it
Bronchial stents
Trauma, blunt
杂志排行
Journal of Acute Disease的其它文章
- Acute brain hemorrhage in dengue
- The epidemiology of tick-borne relapsing fever in Bijar County, North-Western Iran
- Cardioprotective potential of hydro-alcoholic fruit extract of Ananas comosus against isoproterenol induced myocardial infraction in Wistar Albino rats.
- Patients with the tako-tsubo cardiomyopathy-clinical evaluation and outcome
- Functional results of osteosynthesis with mini-plate and screws in metacarpal fractures
- Posterior reversible leukoencephalopathy syndrome presenting in a post-partum, 25-year-old-female with concomitant subarachnoid hemorrhage
